- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
NHS Warns Long Covid Patients To Avoid This Common Mistake

Credits: Canva
Some people who recover from Covid-19 continue to feel unwell for weeks or even months afterward. This condition, called long Covid or post-Covid syndrome, is diagnosed when symptoms last for more than 12 weeks. If you are experiencing it, doctors say there is one thing you should be cautious about.
Although long Covid is not usually life-threatening, it can cause ongoing discomfort and affect many parts of the body in different ways. According to NHS guidance, symptoms vary from person to person and can shift over time.
While the condition can be difficult to manage, there are several treatment options available. These may include physiotherapy, cognitive behavioural therapy, and nutritional guidance to ease symptoms and improve overall health. If you think you might have long Covid, it’s best to see your GP. They can assess your symptoms, run a few tests, and help you get the right diagnosis and care.
What Is Long Covid?
Long Covid refers to a range of ongoing symptoms that continue even after the initial Covid-19 infection has passed. Many people expect to recover within a couple of weeks, yet some find themselves still struggling with fatigue, brain fog, or changes in taste and smell months later. Foods that once tasted normal may now seem metallic or flavourless, and restful sleep can become rare.
As per Cleveland Clinic, rather than being a single illness, long Covid covers any health issue linked to a Covid-19 infection that lasts three months or more after the first symptoms appear. It can affect anyone, regardless of whether their initial case was mild or severe. The symptoms often resemble those seen in autoimmune, respiratory, heart, or neurological conditions, and can also affect mental health.
Some people experience only mild issues, while others find the effects deeply disruptive. The symptoms might fade and return, shift in intensity, or feel as if the body never fully recovered from the original infection.
Symptoms of Long Covid
As noted by the NHS, long Covid can bring a range of symptoms such as:
- Memory or concentration problems, often referred to as brain fog
- Shortness of breath
- Muscle or joint pain
- Extreme tiredness or fatigue
- Sore throat
- Blocked or runny nose
- Chest pain, tightness, or a racing heartbeat (palpitations)
- Pins and needles or general body aches
- Persistent cough
- Trouble sleeping (insomnia)
- Nausea, weight loss, or loss of appetite
- Fever
- Stomach pain or diarrhoea
- Hair loss or skin rashes like hives
- Changes in senses, including altered taste or smell, vision issues, ear pain, or ringing in the ears (tinnitus)
- Headaches, dizziness, or vertigo
- Anxiety and depression
- Sudden confusion (delirium), especially in older adults
Not everyone with long Covid will experience all these symptoms. Some may appear and fade over time, while new ones can develop unexpectedly.
Avoiding Physical Activity
NHS experts warn that long Covid symptoms can worsen if you are under stress or push yourself to be too physically active. They advise against returning to exercise before consulting a GP or specialist.
Research from the University of Leeds also supports this. While physical activity can sometimes help recovery, overexertion may lead to setbacks or worsening symptoms. The researchers suggested that “personalised physical activity plans that reduce the risks of inactivity without triggering long Covid symptoms should be considered a clinical priority.”
If you suspect you have long Covid and are unsure about how much exercise is safe, it’s best to speak with your GP or a healthcare professional for tailored advice.
Why Is This Psychologist Warning Against Benzodiazepines For Anxiety Treatment?

Credits: CANVA
If you struggle with anxiety or trouble sleeping, your doctor may prescribe lorazepam or alprazolam (commonly known as Xanax). These belong to a class of drugs called benzodiazepines, which work by enhancing the effects of gamma-aminobutyric acid (GABA), a chemical in the brain that helps calm the nervous system.
While both medicines are often used to ease anxiety symptoms, alprazolam is also prescribed to control seizures in people with epilepsy. But despite their short-term effectiveness, one clinical psychologist has warned that depending on these medications without addressing underlying issues can be harmful in the long run.
‘Benzodiazepines Don’t Solve the Root Cause,’ Says Psychologist
Spanish psychologist Fernando Azor, known for sharing mental health insights on TikTok, cautioned his followers about the overuse of benzodiazepines.
In a recent video, Azor explained that while drugs such as lorazepam and alprazolam can help calm anxiety attacks, they only mask symptoms rather than helping people understand what triggers their distress.
He added, “People experiencing anxiety crises often struggle to face the physical sensations, such as a racing heart, blurred vision, or nervousness—that come with anxiety. We automatically see them as dangerous or negative, but in reality, they are natural bodily responses to stress.”
According to Azor, perceiving these sensations as something to eliminate immediately can create a cycle of avoidance and dependency, rather than resilience.
Why Relying on Medication Alone Can Backfire
Azor warned that people often reach for these drugs because they take effect quickly, especially when taken under the tongue. This offers temporary relief, but it reinforces the idea that anxiety symptoms must be avoided rather than understood.
He compared it to feeling hunger: “Being hungry can be unpleasant, but it’s not wrong—it signals the body’s needs. Anxiety works similarly. It’s uncomfortable, but not necessarily harmful.”
By suppressing symptoms too quickly, people may avoid learning coping strategies, which can lead to increased distress and reliance on medication.
Learning to Manage Anxiety Through Therapy
The psychologist highlighted that psychotherapy can help individuals build tolerance for uncomfortable sensations instead of fearing them. Through practical exercises and guided experiences, people can learn to sit with their symptoms and understand them logically and emotionally.
“Therapy helps people see that feeling anxious doesn’t always mean something is wrong,” Azor said. “With the right tools, you can live with those sensations without needing to eliminate them instantly.”
When to Seek Professional Help
If you have been feeling persistently anxious, struggling to control your emotions, or having difficulty sleeping for six months or longer, experts recommend speaking to your general practitioner (GP).
According to NHS guidance, treatment for anxiety may include:
- Medications designed to manage anxiety symptoms
- Talking therapies such as cognitive behavioural therapy (CBT)
- Referral to mental health specialists for more tailored support
While benzodiazepines like lorazepam and alprazolam can offer short-term relief, mental health experts warn that they should not replace long-term coping mechanisms. Building emotional awareness and resilience through therapy and self-regulation remains key to managing anxiety sustainably.
WHO Warns Of Rising Mpox Cases As New ‘Clade Ib’ Strain Spreads Globally—See The List Of Affected Countries
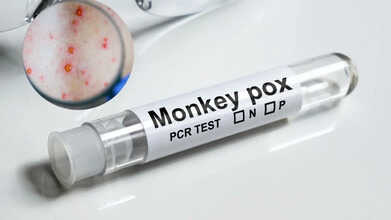
Credits: CANVA
The World Health Organization (WHO) has raised concern over the continued spread of Mpox (formerly known as monkeypox) across Africa and other regions. In the past six weeks alone, 17 African nations have reported active transmission. Between September 14 and October 19, there were 2,862 confirmed infections and 17 related deaths, according to WHO’s 59th multi-country situation report released on October 30.
The Democratic Republic of Congo, Liberia, Kenya, and Ghana have reported the highest number of cases. Infections have increased notably in Kenya and Liberia, while the Democratic Republic of Congo has seen a slight decline and Ghana is beginning to show early signs of improvement.
What Is Mpox and How Does It Spread?
Mpox, previously known as monkeypox, is a viral infection caused by the monkeypox virus, which belongs to the Orthopoxvirus genus. The World Health Organization (WHO) identifies two main clades of the virus, Clade I (subdivided into Ia and Ib) and Clade II (IIa and IIb). The widespread outbreak seen during 2022–2023 was primarily linked to Clade IIb.
Typical symptoms include skin rashes or lesions that last two to four weeks, along with fever, body aches, swollen lymph nodes, fatigue, and headaches.
The infection spreads through close physical contact with an infected person, contaminated objects, or animals carrying the virus. Transmission from a pregnant woman to her baby can also occur.
How Serious Is the Global Mpox Situation Now?
According to the World Health Organization (WHO), a total of 42 countries reported 3,135 confirmed Mpox infections and 12 related deaths in September, with more than four-fifths of all cases recorded in Africa. While most regions have seen infection rates ease, the European and South-East Asian regions are now showing a slight increase.
The WHO stated that all variants, or clades, of the monkeypox virus (MPXV) remain in circulation worldwide. Experts caution that if emerging outbreaks are not swiftly controlled, ongoing community transmission may occur.
It is worth noting that in the same month, the WHO ended Mpox’s designation as a Public Health Emergency of International Concern (PHEIC) after observing a consistent decline in new infections, particularly in heavily affected African countries.
Where Has the New Clade Ib Variant Been Found?
The Clade Ib form of the Mpox virus has been newly detected in Malaysia, Namibia, the Netherlands, Portugal, and Spain. Additional imported cases linked to international travellers carrying the same strain have appeared in Belgium, Canada, Germany, Italy, Qatar, and Spain.
Evidence of local transmission—cases without any recent travel exposure, has been confirmed in six countries outside Africa: Italy, Malaysia, the Netherlands, Portugal, Spain, and the United States. In the U.S., three patients hospitalised in California tested positive for the new variant despite no travel history, according to The Guardian, prompting concern among health authorities.
Following these developments, WHO has officially classified these countries as experiencing community-level spread of the Clade Ib MPXV strain.
How Are Countries Responding to the Renewed Spread of Mpox?
WHO continues to assess the global Mpox threat as moderate among men who have sex with men (MSM) and low for the general population. The agency is encouraging governments to sustain surveillance systems, improve testing capabilities, and maintain access to vaccines and treatment options to prevent wider community outbreaks.
Blood Pressure Medication Recall 2025: Could Your Prescription Be on the FDA List?

Credits: CANVA
Medication recall blood pressure: More than 580,000 bottles of Prazosin Hydrochloride, a commonly prescribed drug for high blood pressure, are being recalled after tests showed potentially unsafe levels of a cancer-linked impurity. The manufacturer has advised patients using the affected medication to reach out to their doctor or pharmacist for guidance.
The recall, issued on October 7 by New Jersey–based Pharmaceuticals USA Inc., involves 55 batches of Prazosin Hydrochloride capsules distributed across the country. The recalled products were sold in 1 mg, 2 mg, and 5 mg doses under the Teva Pharmaceuticals label.
Below is the list of prescription numbers included in the FDA’s recall notice, along with medical advice on what steps to take if your medication is affected.
FDA gov blood pressure medication recall: Which Medicine Is Being Recalled?
Teva Pharmaceuticals USA and Amerisource Health Services have both recalled certain batches of prazosin hydrochloride this month after the U.S. Food and Drug Administration (FDA) detected possible contamination. According to FDA enforcement reports, the affected capsules may contain nitrosamine impurities that exceed the limits set under the agency’s Carcinogenic Potency Categorization Approach (CPCA).
Nitrosamines are a group of chemical compounds that, when present in high amounts, have been linked to an increased risk of cancer. They can form during the production or storage of certain medications.
The FDA classified these recalls as Class II on October 24, indicating that while the affected drugs could cause temporary or reversible health effects, the likelihood of severe harm is considered low.
Current Blood Pressure Medication Recall: Which Lot Are Affected?
The recall applies only to the 1 mg, 2 mg, and 5 mg capsules of prazosin hydrochloride distributed by Teva Pharmaceuticals USA and Amerisource Health Services. It affects select batches identified by specific lot numbers and expiration dates.
The majority of the recalled supply, over 580,000 bottles, came from Teva, with the remainder distributed by Amerisource. Details on the affected products, including the complete list of lot codes and expiry information, are available in the FDA’s official enforcement reports.
As reported by USA Today, the recall includes several dosages and packaging of the medication:
- 1 mg capsules: 181,659 bottles (NDC 0093-4067-01 and 0093-4067-10), from lot numbers 3010544A and 3010545A, with an expiration date of October 2025.
- 2 mg capsules: 291,512 bottles (NDC 0093-4068-01 and 0093-4068-10) from multiple lots, expiring between October 2025 and July 2026.
- 5 mg capsules: 107,673 bottles (NDC 0093-4069-01, 0093-4069-52, and 0093-4069-05) from several batches, with expiration dates extending into 2026.
What To Do If You Have The Recalled Blood Pressure Pills?
If you have any of the recalled prazosin hydrochloride capsules, the FDA recommends contacting your doctor or pharmacist before stopping the medication. In some cases, discontinuing treatment without medical supervision could pose greater health risks than continuing it.
Teva Pharmaceuticals has urged patients to check with their pharmacy to confirm whether their medication is part of the recall and to follow the instructions provided for returning or disposing of the affected pills. The company has already issued recall letters to its customers detailing the process.
Teva noted that no complaints have been reported so far related to the recalled batches. The company added that prazosin, which is used to manage high blood pressure, has several alternative treatments available. “Teva prioritizes patient safety and product quality at every stage of a medicine’s lifecycle,” the statement read.
Patients who have concerns or need further guidance are advised to speak with their prescribing healthcare provider.
© 2024 Bennett, Coleman & Company Limited

