- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Dealing With Health Anxiety: When Normal Concerns Become Overwhelming Fears

HEALTH ANXIETY
For years, Rhea found myself consumed by every minor ache or twitch, convinced it was something life-threatening. Despite endless doctor visits and tests confirming her health, the anxiety never faded. Learning that my brain was just trying to protect me helped me break the cycle and reclaim peace of mind.
If you’ve ever scrolled through health websites after a simple headache, convinced it’s something severe, you might recognize the pattern of health anxiety. This condition is characterized by persistent worry about having or developing a serious illness, even in the absence of symptoms or with very minor symptoms, such as a scratchy throat or mild discomfort.
People with health anxiety often imagine the worst-case scenarios, such as cancer or heart disease, and despite medical reassurance, their fear doesn't fade.
It’s essential to understand that our brains are wired to react to potential threats. When you have health anxiety, your brain's instinct to protect you can go into overdrive. Instead of recognizing that a scratchy throat might be a sign of a cold, your brain may jump to the conclusion that it’s something more severe, like cancer.
This reaction is not irrational—it's your brain trying to keep you safe. A helpful way to manage these thoughts is by reminding yourself, "My brain is trying to protect me. This is a normal response."
Here’s a step-by-step process to help calm yourself during health anxiety:
1. Acknowledge the Protective Role of Your Brain: Remind yourself that your brain is acting out of instinct, trying to shield you from harm.
2. Pause Without Judging Your Thoughts: Allow the thoughts to come, but don’t engage with them emotionally or act impulsively.
3. Breathe and Calm Your Immediate Reaction: Taking deep breaths can reduce the intensity of your anxiety and help you regain control over your thoughts.
4. Take a Break: Instead of reacting immediately to your thoughts, distract yourself with another activity, whether it’s taking a walk or engaging in a hobby.
5. Challenge Your Thoughts Later: Once you’ve calmed down, ask yourself whether there’s actual evidence to support your fears or if you're simply reacting out of anxiety. Ask, "Have I felt this before and it turned out to be false?"
How Health Anxiety Looks Like?
When you notice thoughts like these, remind yourself that your brain has a natural, protective response, that’s why it reacts impulsively to danger. It’s what it’s supposed to do. Here’s a step-by-step example of how to work through this when it happens:
- Tell yourself - “my brain is trying to keep me safe, this is what it’s supposed to do”
- Allow yourself a moment to let the thoughts happen without judgment or reaction.
- Take a few deep breaths to calm your immediate emotional response.
- Take time out instead of reacting - go do something else.
- After time has passed ask yourself - is there real evidence to support this thought?
- What are other possible explanations for my experience apart from this though?
- Have I had similar thoughts before that turned out to be false?
What is Health Anxiety?
Health anxiety involves the misinterpretation of normal bodily sensations as signs of serious illness. For instance, a muscle twitch might be feared as a symptom of ALS, or a headache might be seen as a sign of a brain tumor. These sensations are real, but they aren’t always dangerous. The key issue is the constant worry and fear surrounding normal bodily changes.
The difference between anxiety and health anxiety lies in how one reacts to bodily sensations. With general anxiety, people might experience symptoms like dizziness, rapid heartbeat, or muscle tension.
However, in health anxiety, these physical symptoms are misinterpreted as evidence of a serious disease. Even after medical reassurance, the anxiety persists, creating a vicious cycle of worry, research, and doctor visits.
Recognizing Health Anxiety
Health anxiety differs from ordinary health concerns in its intensity and persistence. It’s normal to worry about our health from time to time, especially when experiencing genuine symptoms like a stomachache or headache. However, health anxiety goes beyond typical concern. You might experience health anxiety if:
- You have no significant symptoms, yet you still fear that you’re gravely ill.
- Medical reassurance doesn’t alleviate your worry. Even after doctors and tests confirm your health, you continue to feel anxious about possible illnesses.
- You compulsively research health information online, leading to even more anxiety.
- News about diseases can make you worry that you have or will contract them.
- Your health worries are affecting your daily life, interfering with work, family time, or hobbies.
People with health anxiety often focus on severe illnesses, such as cancer, HIV, or dementia, rather than minor ailments like the flu or a sprained ankle. Their fear can become so overwhelming that it drives them to seek unnecessary medical testing, spend hours in doctors' offices, and engage in excessive health monitoring. It’s a cycle that often begins with a benign symptom and escalates into a belief that something is seriously wrong.
For many individuals with health anxiety, visiting the doctor and getting tests done might seem like a way to calm their nerves. However, for those whose anxiety has spiraled out of control, testing rarely offers lasting relief.
While a negative test result may temporarily reduce worry, the anxiety soon returns, often focusing on a new symptom or fear. In some cases, repeated testing and doctor visits become habitual, further reinforcing the anxiety rather than alleviating it.
How to break the Cyclic Thoughts of Health Anxiety?
The cycle of health anxiety is challenging to break because it often involves compulsive behaviors like Googling symptoms, seeking reassurance, and avoiding doctors out of fear. If you or someone you know experiences health anxiety, the first step is recognizing the pattern and seeking professional help, such as therapy.
Cognitive Behavioral Therapy (CBT) has been proven to help manage health anxiety by teaching individuals how to challenge their thoughts and reduce compulsive behaviors.
Disclaimer: This article provides general information and is not a substitute for professional medical advice. If you are experiencing health anxiety, please consult a healthcare professional.
Lung Cancer Is Not Just a Smoker’s Disease; Here is What is Putting You at Risk

It is true that lung cancer is commonly seen among smokers. About 85 per cent of all lung cancers are directly related to tobacco use, especially smoking. However, nearly 10–20 per cent of lung cancers each year occur in people who have never smoked or who have smoked fewer than 100 cigarettes in their lifetime.
It is also the fifth most common cause of cancer-related death worldwide. Even if you have never smoked in your life, there is a possibility that you may still get lung cancer. While smoking has traditionally been seen as the leading culprit, other risk factors are increasingly being recognised.
Pollution, Family History and Hidden Risks
“We have seen that there are many other factors which may lead to the development of lung cancers. The most important ones are air pollution, especially in Southeast Asia and the Indian subcontinent," says Dr Kamran Ali, Principal Consultant, Lung Transplant and Thoracic Surgery, Max Super Speciality Hospital, New Delhi. He explains that pollutants from vehicles and industry, such as benzene and heavy metals, can contribute to lung cancer risk.
Long-term exposure to polluted air may cause persistent inflammation in the lungs, weakening the immune system and making it easier for cancer cells to grow. He warns about exposure to radon gas, which is found in soil and can sometimes creep into homes.
Long-term exposure to second-hand smoking or third-hand smoking also increases risk, says Dr Ali, pointing out that many people underestimate these dangers. He adds that genetic susceptibility also plays a role: "If your parents have lung cancer or your sibling has lung cancer, it does increase the risk of lung cancer for you as well.”
He also explains a lesser-known cancer, saying, “There is a separate intake entity called mesothelioma which arises from the surface of the lung. It is not from the lung itself. It is from the surface of it which is associated with asbestos.” Although asbestos is now banned, it was previously used in roofing and packaging industries. Dr Ali cautions against exposure to other heavy metals like chromium.
How Non-Smoker Lung Cancer Differs
Non-smoker lung cancers are slightly different from smokers’ lung cancers. “Classically, non-smokers’ lung cancer is usually an adenocarcinoma, which is found in the outer third of the lung surface,” he explains, adding that it often presents more vaguely than smoking-related cancers: “It also presents as a vague or a diffuse involvement of the lung rather than like a nodule or a mass.”
Dr Ali says it is typically slow-growing and less likely to spread to other parts of the body compared to lung cancer in smokers.
Watch for the Silent Signs
So lung cancer is a silent killer. If you have symptoms like a cough that worsens over time or a cough that does not go away, blood while you cough, unexplained weight loss, shortness of breath, or chest pain, you need to consult your local thoracic surgeon. The expert stresses that early detection is critical for effective treatment.
Prevention Starts with Awareness
To lower your risk, Dr Ali shares these preventive measures:
- Refrain from venturing out of your house when the air pollution level is in a severe state outside.
- If necessary to go outside, use an N95 mask in polluted areas.
- You should use air purifiers indoors to filter out harmful particles.
- Incorporate fresh fruits and vegetables in your daily diet.
- Drink plenty of water to keep you hydrated.
- You can practise some appropriate breathing exercises to enhance your lung function.
- If you have a strong family history of lung cancer, you must meet a thoracic surgeon or oncologist to get yourself evaluated.
UK Scientists Scan Over 100,000 People, What The Human Imaging Study Could Reveal About Your Health?
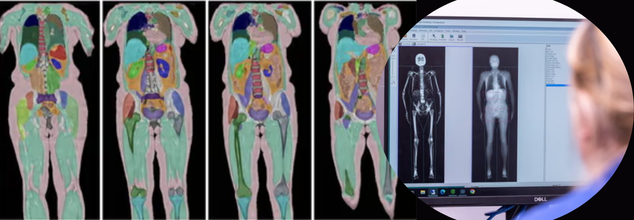
Credits: UK Biobank
In a world-first scientific effort, researchers in the UK have completed the largest human imaging study in history, scanning the bodies of over 100,000 volunteers. The result? More than one billion medical images—and a revolutionary new understanding of how diseases begin, progress, and, crucially, how they can be stopped before symptoms appear.
This landmark milestone is part of the UK Biobank Imaging Study, a government-backed project that has been quietly building one of the most detailed health databases in the world for over a decade. Now, after 11 years of work, the study is delivering insights that could permanently reshape the future of preventive healthcare.
Why Are Scientists Scanning for the Whole Human Story?
Each participant in the study spent about five hours undergoing advanced imaging: magnetic resonance imaging (MRI) of the brain, heart, liver, and abdomen; DEXA scans to assess bone density and body fat; and ultrasounds of the carotid arteries. In total, more than 12,000 images per person were collected.
But the images are just one piece of a much larger puzzle. These scans are linked with each individual’s genetics, lifestyle choices, blood biomarkers, and medical history—many of which have been tracked for over 15 years. It’s this integration of data that allows researchers to identify disease patterns invisible to conventional medicine.
“This massive imaging project is making the invisible visible,” says Professor Sir Rory Collins, principal investigator and CEO of UK Biobank. “We’re seeing how disease takes hold silently, shaped by genetics, lifestyle, and environment long before symptoms begin.”
How the Data Is Already Saving Lives?
The data has already sparked breakthroughs that are changing how diseases are diagnosed and treated across the world. Take dementia, for instance. NHS memory clinics are now using tools developed through UK Biobank to analyze brain scans with far greater accuracy.
In cardiac care, an AI tool trained on UK Biobank data is being used in over 90 countries to scan heart images in under a second—a task that previously took clinicians nearly 15 minutes.
The power of scale can’t be overstated. By comparing hundreds of thousands of images of healthy individuals with those who developed disease, scientists have been able to develop AI-driven models to detect:
- Early signs of liver disease
- Calcification in major arteries
- Brain shrinkage from even mild alcohol use
- Abnormal fat distribution linked to diabetes and cardiovascular disease
Studying the Science of Disease, Before It Strikes
What makes UK Biobank’s imaging study different is its ability to see disease in the making. Researchers aren’t just looking at patients after symptoms appear. They’re watching how organs change over time and using AI to predict what might happen next.
For instance, by comparing a person’s actual heart image to a personalized digital “healthy twin” (an AI-generated model based on age, sex, height, and weight), doctors can identify the earliest signs of cardiac deterioration—before it shows up in routine tests.
The study has also shown that organs can biologically age faster than the rest of the body. This means someone could have a healthy-looking BMI, but their liver or brain might already be at risk. These insights could fundamentally change how we define "at-risk" populations.
Perhaps one of the most eye-opening takeaways from the project is how misleading traditional health indicators can be.
Two people with identical BMIs might carry fat in radically different—and clinically significant—ways. One may store fat in protective subcutaneous layers, while another may accumulate it around vital organs, increasing their risk of heart disease and diabetes.
“Body mass index is a very crude measure,” says Collins. “We now know the health risk associated with different fat distributions can be vastly different.”
COVID-19 and the Hidden Toll on the Brain
The UK Biobank’s imaging database even gave scientists a unique opportunity during the pandemic: analyzing brain scans taken before and after COVID-19 infections. What they found was alarming—evidence of brain shrinkage in areas responsible for memory, smell, and emotion, even in patients with mild symptoms.
This was one of the first pieces of concrete neurological evidence of COVID-19’s lingering effects, made possible only because of the repeat scanning design of the Biobank study.
The entire dataset is housed on a cloud-based platform, currently accessed by over 21,000 researchers from more than 60 countries. Crucially, the platform is open to early-career scientists and researchers in low-resource settings—democratizing access to one of the most powerful tools in modern health science.
To date, the data has been the foundation for more than 16,000 peer-reviewed scientific papers, helping to drive policy changes, update clinical protocols, and accelerate drug discovery.
How These Scans Will Help Predict Illness Years in Advance?
The study’s next phase aims to include repeat scans for all 100,000 participants. With that, scientists will be able to track how changes in the brain, heart, liver, and fat distribution occur over time—and tie those changes to environmental exposures, behaviors, and genetics.
Already, AI models trained on Biobank data are being used to predict the onset of 38 different diseases, often years before symptoms emerge. The ultimate goal? A system where a routine scan could flag risk factors early enough for lifestyle changes or treatment to prevent disease altogether.
This study doesn’t just reveal what’s possible when imaging data is scaled—it shows what’s missing in most health systems worldwide: routine access to whole-body imaging.
Most people never undergo a scan unless they’re already sick. Yet this project proves that diseases like Alzheimer’s, fatty liver, and cardiovascular complications begin quietly, and can be detected early with the right tools.
Imagine a future where whole-body scans, paired with AI and personal data, become a standard part of preventive checkups—just like blood pressure or cholesterol testing. That future isn’t far off. UK Biobank is paving the way.
The UK Biobank’s imaging study is more than a scientific milestone—it’s a mindset shift. Instead of chasing illness after it appears, the study invites us to rethink healthcare as a forward-looking, data-powered practice that identifies risk before it becomes reality.
As Sir Rory Collins said, “We ain’t seen nothing yet.” He’s right. What this study makes clear is that the best time to treat disease is before it starts—and now, we finally have the tools to make that possible.
You Are Starting Your Day All Wrong! A Neuroscientist Reveals The 20-Minute Morning Tweak That Could Unlock Your Creativity, Motivation And Focus

Checking our phone as soon as we wake has become a new normal, leaving far behind good old healthy practices like yoga, stretching, reading a newspaper or simply relaxing on the balcony. What has become a habit now is to reach for our phone before we have even fully opened both eyes. Scroll through Instagram, check the news, peep your inbox, maybe? So nobody is alone in this. But according to this neuroscientist, your brain hates this. Yes, hates!
Your Brain’s Morning Superpower
The moment you wake up, your brain enters what Dr. Wendy Suzuki, a neuroscientist and Dean of the College of Arts and Sciences at New York University, calls peak neuroplastic mode, meaning it is in its most malleable, adaptable, and brilliant state, ready to learn, problem-solve and innovate.
“You have been starting your day out all wrong, and your brain hates it. If your first move in the morning is checking your phone, your brain misses out on its most powerful window of the day. Right after waking up, your brain is in peak neuroplastic mode,” she says in a video shared on Instagram.
Along with this neuroplasticity boost, your brain also experiences a natural rise in dopamine and cortisol levels in the early hours. Dopamine and cortisol (in their optimal, non-stress-inducing doses) help sharpen your focus, increase creativity, and get you mentally primed for the day.
But the moment you expose your just-woken-up brain to a screen, that power surge gets zapped.
Screens Hijack Your Mind
You know that itchy, anxious feeling you sometimes get after doomscrolling in bed? That is no coincidence. Dr. Suzuki says dopamine and cortisol are naturally high, giving you a boost in motivation, creativity, and focus. But screens hijack that potential.
By checking emails or diving into social media, you are handing over the reins of your brain’s agenda to external noise like other people’s updates, demands, and drama. Instead of using that precious cognitive spike for yourself, you are giving it away. Think of it as spending the best part of your mental energy budget on junk.
The 20-Minute Reset Experiment
Do not worry; Dr. Suzuki is not asking you to throw your phone away. The fix is refreshingly simple. Just delay screen time by 20 minutes. No fancy apps, no complicated rituals. Just give your brain a 20-minute grace period to breathe, stretch, and be.
"For the next five mornings, delay screen time by just 20 minutes. Instead, stretch. Write down three things you want to focus on or just sit with your coffee and your thoughts. Watch what happens when you give your brain space to lead," she says.
Sounds easy, right? But do not underestimate the impact. Those 20 minutes could become the most productive part of your day. They can set the tone for intentional action instead of reaction.
Make Your Brain the Boss of Your Morning
Tomorrow, when your alarm goes off, resist the twitchy urge to swipe. Let your brain stretch its legs first. Stretch your body, jot down your day’s top three priorities, or just sit still and sip your morning brew.
© 2024 Bennett, Coleman & Company Limited

