- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
UK Scientists Scan Over 100,000 People, What The Human Imaging Study Could Reveal About Your Health?
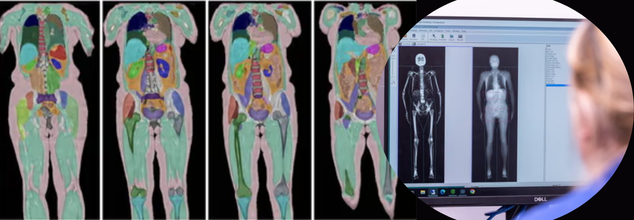
Credits: UK Biobank
In a world-first scientific effort, researchers in the UK have completed the largest human imaging study in history, scanning the bodies of over 100,000 volunteers. The result? More than one billion medical images—and a revolutionary new understanding of how diseases begin, progress, and, crucially, how they can be stopped before symptoms appear.
This landmark milestone is part of the UK Biobank Imaging Study, a government-backed project that has been quietly building one of the most detailed health databases in the world for over a decade. Now, after 11 years of work, the study is delivering insights that could permanently reshape the future of preventive healthcare.
Why Are Scientists Scanning for the Whole Human Story?
Each participant in the study spent about five hours undergoing advanced imaging: magnetic resonance imaging (MRI) of the brain, heart, liver, and abdomen; DEXA scans to assess bone density and body fat; and ultrasounds of the carotid arteries. In total, more than 12,000 images per person were collected.
But the images are just one piece of a much larger puzzle. These scans are linked with each individual’s genetics, lifestyle choices, blood biomarkers, and medical history—many of which have been tracked for over 15 years. It’s this integration of data that allows researchers to identify disease patterns invisible to conventional medicine.
“This massive imaging project is making the invisible visible,” says Professor Sir Rory Collins, principal investigator and CEO of UK Biobank. “We’re seeing how disease takes hold silently, shaped by genetics, lifestyle, and environment long before symptoms begin.”
How the Data Is Already Saving Lives?
The data has already sparked breakthroughs that are changing how diseases are diagnosed and treated across the world. Take dementia, for instance. NHS memory clinics are now using tools developed through UK Biobank to analyze brain scans with far greater accuracy.
In cardiac care, an AI tool trained on UK Biobank data is being used in over 90 countries to scan heart images in under a second—a task that previously took clinicians nearly 15 minutes.
The power of scale can’t be overstated. By comparing hundreds of thousands of images of healthy individuals with those who developed disease, scientists have been able to develop AI-driven models to detect:
- Early signs of liver disease
- Calcification in major arteries
- Brain shrinkage from even mild alcohol use
- Abnormal fat distribution linked to diabetes and cardiovascular disease
Studying the Science of Disease, Before It Strikes
What makes UK Biobank’s imaging study different is its ability to see disease in the making. Researchers aren’t just looking at patients after symptoms appear. They’re watching how organs change over time and using AI to predict what might happen next.
For instance, by comparing a person’s actual heart image to a personalized digital “healthy twin” (an AI-generated model based on age, sex, height, and weight), doctors can identify the earliest signs of cardiac deterioration—before it shows up in routine tests.
The study has also shown that organs can biologically age faster than the rest of the body. This means someone could have a healthy-looking BMI, but their liver or brain might already be at risk. These insights could fundamentally change how we define "at-risk" populations.
Perhaps one of the most eye-opening takeaways from the project is how misleading traditional health indicators can be.
Two people with identical BMIs might carry fat in radically different—and clinically significant—ways. One may store fat in protective subcutaneous layers, while another may accumulate it around vital organs, increasing their risk of heart disease and diabetes.
“Body mass index is a very crude measure,” says Collins. “We now know the health risk associated with different fat distributions can be vastly different.”
COVID-19 and the Hidden Toll on the Brain
The UK Biobank’s imaging database even gave scientists a unique opportunity during the pandemic: analyzing brain scans taken before and after COVID-19 infections. What they found was alarming—evidence of brain shrinkage in areas responsible for memory, smell, and emotion, even in patients with mild symptoms.
This was one of the first pieces of concrete neurological evidence of COVID-19’s lingering effects, made possible only because of the repeat scanning design of the Biobank study.
The entire dataset is housed on a cloud-based platform, currently accessed by over 21,000 researchers from more than 60 countries. Crucially, the platform is open to early-career scientists and researchers in low-resource settings—democratizing access to one of the most powerful tools in modern health science.
To date, the data has been the foundation for more than 16,000 peer-reviewed scientific papers, helping to drive policy changes, update clinical protocols, and accelerate drug discovery.
How These Scans Will Help Predict Illness Years in Advance?
The study’s next phase aims to include repeat scans for all 100,000 participants. With that, scientists will be able to track how changes in the brain, heart, liver, and fat distribution occur over time—and tie those changes to environmental exposures, behaviors, and genetics.
Already, AI models trained on Biobank data are being used to predict the onset of 38 different diseases, often years before symptoms emerge. The ultimate goal? A system where a routine scan could flag risk factors early enough for lifestyle changes or treatment to prevent disease altogether.
This study doesn’t just reveal what’s possible when imaging data is scaled—it shows what’s missing in most health systems worldwide: routine access to whole-body imaging.
Most people never undergo a scan unless they’re already sick. Yet this project proves that diseases like Alzheimer’s, fatty liver, and cardiovascular complications begin quietly, and can be detected early with the right tools.
Imagine a future where whole-body scans, paired with AI and personal data, become a standard part of preventive checkups—just like blood pressure or cholesterol testing. That future isn’t far off. UK Biobank is paving the way.
The UK Biobank’s imaging study is more than a scientific milestone—it’s a mindset shift. Instead of chasing illness after it appears, the study invites us to rethink healthcare as a forward-looking, data-powered practice that identifies risk before it becomes reality.
As Sir Rory Collins said, “We ain’t seen nothing yet.” He’s right. What this study makes clear is that the best time to treat disease is before it starts—and now, we finally have the tools to make that possible.
Measles Can Erase Your Immune System’s Memory—Here’s What That Means
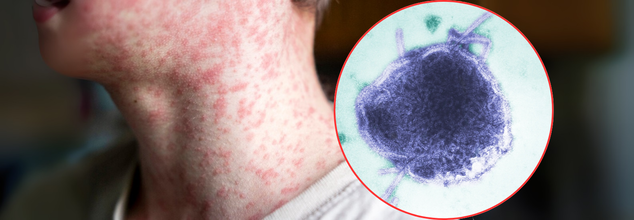
Credits: Canva
As measles outbreaks rise again across the globe, scientists and health officials are sounding the alarm — not just about the virus itself, but a hidden side effect that could be even more dangerous: immune amnesia. This isn’t a metaphor. Measles has the terrifying ability to literally wipe out your body’s immune memory, undoing years of protection built up from past infections and vaccinations.
Measles was once considered largely defeated in many countries. Canada declared it eliminated in 1998. The U.S. was close behind. But in recent years, due to declining vaccination rates, pandemic-related disruptions, and growing vaccine hesitancy, cases are creeping back up.
Measles isn’t just a rash and a fever — it can cause pneumonia, blindness, brain inflammation, and even death. But its legacy may last far longer than the illness itself.
A growing body of research shows that after recovering from measles, many children and adults lose immune protection they had already built against other diseases like the flu, mumps, or even those they were vaccinated for. This phenomenon is called immune amnesia.
What Is Immune Amnesia?
Your immune system relies on memory to protect you. When you fight off an infection or get a vaccine, special cells (B and T lymphocytes) “remember” those pathogens so your body can quickly recognize and neutralize them in the future. Think of it like a security system keeping a watchlist of past intruders. Measles wrecks that system.
“Immune amnesia basically destroys your immune system,” explains Dr. Stephen J. Elledge, professor of genetics and medicine at Harvard Medical School, who has published extensively on the topic. “It infects and kills the cells that store immune memories — plasma cells, B cells, and T cells. It’s like burning down a library full of immunological knowledge.”
A 2019 study in Science, co-authored by Elledge, found that measles can wipe out up to 73% of a person’s immune memory. In other words, after recovering from measles, your immune system might not remember how to fight the flu, pneumonia, or other pathogens it once had under control. That puts you at risk for reinfections — even with diseases you already beat.
What makes immune amnesia so dangerous is how comprehensive it is. Unlike other viruses like influenza, which might weaken the immune system temporarily, measles erases learned immunity, setting your body back to a baby-like state.
The body will still remember how to fight measles (since it had to win that battle to survive), but all the rest — the defenses built from years of exposure and vaccination — could be gone. It can take two to three years to rebuild that immunity, according to a 2015 study, and that rebuilding relies on exposure or re-vaccination.
So, someone recovering from measles could remain vulnerable to severe infections for years — and not even know it.
How Immune Amnesia Affects The Body?
Every virus needs a doorway into the body’s cells. For measles, that doorway is a protein called SLAM, found on immune memory cells. Once the virus binds to SLAM, it infiltrates and destroys plasma cells — the very cells responsible for pumping out antibodies and maintaining immune memory.
It’s like a heist film where the thief knows the combination to the vault — and once inside, doesn’t just steal your valuables, but burns the blueprints so you can never secure the vault again. That’s what makes measles unique — and uniquely dangerous.
Virtually everyone who gets measles experiences some form of immune amnesia, though the extent varies. Children, especially infants under 12 months who aren’t yet vaccinated, are at highest risk. Their immune systems are still developing, and losing what little protection they’ve built can be devastating.
Older adults are also vulnerable because of natural immune decline with age. And anyone with existing health conditions or suppressed immunity could struggle even more to rebuild what the virus has wiped out.
How Vaccine Does More Than Prevent Measles?
Here’s the twist: the measles vaccine doesn’t just prevent measles — it may help strengthen the immune system overall.
Scientists have observed that vaccinated children have lower mortality rates not just from measles, but from other infections too. One theory is that by avoiding immune amnesia, the vaccine helps preserve the immune memory you’ve already built. Another is the non-specific effect — where live vaccines like the MMR (measles, mumps, rubella) train the immune system to better handle unrelated threats.
Either way, the MMR vaccine may be offering a broader shield than once thought.
One dose of the MMR vaccine, typically given at 12–15 months, is estimated to be 85–95% effective. A second dose (often at 4–6 years old) brings that protection close to 100%. And crucially, the vaccine does not cause immune amnesia — only the virus does.
In the 1960s, measles killed an estimated 2.6 million people annually worldwide. Thanks to vaccines, that number dropped drastically. Between 2000 and 2023, over 60 million deaths were prevented but in a world where many haven’t seen the true face of measles, complacency has crept in. Misinformation spreads. Anti-vaccine sentiment grows. And with it, so does the virus.
As of this year, outbreaks have been reported across the UK, Canada, and the U.S., especially in areas with low vaccine coverage. Public health agencies are now urging people to check their vaccination status — not just for themselves, but to protect their communities.
There’s a dangerous myth that measles is just part of growing up — a few days of rash and fever, then you’re done. That couldn’t be further from the truth.
Measles is a highly contagious, immune-erasing virus that can have life-threatening complications. It doesn’t just affect you while you’re sick. It leaves a trail of destruction inside your immune system that can take years to recover from — if ever. Vaccines don’t just protect against measles. They preserve everything your immune system has learned — and may even make it stronger.
The Overlooked Role of Men in IVF: Why Their Silent Strength Is Key to Fertility Success

When couples begin the IVF journey, much of the focus understandably rests on the woman. She undergoes the treatments, endures the physical toll, and often voices the emotional struggles. But the man’s quiet role deserves more credit than it gets. While women express their emotions openly, men often take a more grounded approach. Their silence is not always a sign of suppression. It is frequently a choice grounded in calm, a way of creating emotional space so that the couple can move forward with clarity and purpose.
Acceptance, Not Resignation
According to Dr Seema Jain, Department of Fertility at Cloudnine Group of Hospitals, Pune, acceptance is not about giving up. “Not passivity, not resignation, but a grounded understanding of what is and a steady willingness to walk the journey as it comes," she says.
This attitude creates emotional stability. While one partner may spiral into worry about test results or possible outcomes, men often hold the fort. By staying calmly optimistic, men often give the couple room to breathe and move forward.
The Practical Backbone
It is not just emotional steadiness. Dr Jain shares that in many cases, it is the man who manages appointments, coordinates reports, speaks to multiple departments, or handles financial planning for the treatment.
These behind-the-scenes efforts form the scaffolding of the IVF journey. Emotionally, too, many men help sustain the process with a solution-focused mindset:
- What can we do next?
- Let us talk to the doctor again.
- We will keep going till we get there.
Dr Jain says this attitude offers more than just help. “It creates momentum.”
A Deliberate Kind of Detachment
There is a common misreading of men’s emotional restraint during IVF as indifference. But Dr Jain urges a closer look. “It is a deliberate emotional stance, one that comes from wanting to protect their partner from spiralling further into stress or hopelessness," she says.
She explains that this composure allows men to hold up the practical side of the journey, giving their partners the space to feel. “Their detachment is not coldness; it is clarity. Their silence is not withdrawal; it is support.”
The Man Behind the Success
Behind many IVF success stories, Dr Jain says, is a partner who did not falter. A man who showed up for every scan, absorbed every setback, and smiled through the tears; not because he was not hurting, but because he knew his strength held the family together.
He is the one who said, “Let’s try again.” The one who sat quietly in waiting rooms yet stayed hopeful. “It is time we acknowledge that these men are not silent victims; they are silent champions,” says Dr Jain.
Why Support Matters
Dr Jain emphasises that mental health support for men is essential, not because they are crumbling, but because “they are strong for too long, too often.” Offering them space to talk, reflect, or simply rest is a way to acknowledge the vital role they play. Supporting men ensures that they can continue to lead, hold space, and uplift without being worn down silently.
In a world where fertility conversations often leave men in the background, Dr Jain urges a shift in focus. “Let us stop framing men in fertility only as quiet sufferers. Let us start seeing them as quiet enablers of success.”
Because, as she rightly says, “Thanks to them, many IVF stories are not just possible; they are powerful.”
Giardia Infection from the Well: Doctor Warns Against Drinking Water Straight from ‘Natural’ Sources

For one unlucky traveller, that picture-perfect getaway turned into weeks of misery after he suffered chronic diarrhoea and unexplained weight loss. Upon diagnosis, it was found that he had a Giardia infection due to drinking unfiltered well water. It is a case shared by gastroenterologist Dr Saurabh Sethi, known as doctor.sethi on Instagram, who treated the patient. And he is sounding the alarm, loud and clear, that even the most pristine-looking water sources can be teeming with microscopic parasites.
Giardia is actually a gut-wrecking parasite, common in untreated water like wells, lakes, streams, and even resort town taps. If water has even a trace of contamination, Giardia can wreak havoc in your gut. The parasite flattens the lining of your gut, wrecking your ability to absorb nutrients and leaving you weak, dehydrated, and with loose stools.
Clear water does not equal safe water, especially when it comes to what you drink. Even the crystal-clear mountain spring could be having parasites.
Filter It, Boil It, But Never Drink It Straight
Dr Sethi’s takeaway is simple but critical: always filter or boil well water, no matter how clean it looks. A portable water filter, boiling for at least a minute, or using chlorine or iodine tablets can all kill off lurking pathogens.
For those using well water regularly at home, proper testing and a reliable filtration system are must-haves. Annual checks for bacteria, nitrates, and parasites are boring but essential. And if you are travelling, pack smart. A tiny filter straw or water-purifying tablets can be the difference between a peaceful trip and parasitic mayhem.
Your Gut Deserves Better
The gut is more than just a food tube; it handles your immune system, your nutrient factory, and your second brain. Trashing it with contaminated water is not the safest thing to do.
© 2024 Bennett, Coleman & Company Limited

