- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Can You Crack These Brain Teasers? Put Your Logic To The Test!
Quiz- brain teasers
Get ready to test your brainpower! These four brain teasers will challenge your logic, family relations, and problem-solving skills. See how many you can solve!
1) Two fathers, two sons go fishing. They each catch one fish, yet in all, only three fish are caught. How is that possible?

(Image courtesy: Freepik)
2) A man looks at a photograph and says, "Brothers and sisters, I have none. But the father of that man in the picture is my father's son." Who is the fellow in the photograph?

(Image courtesy: Freepik)
3) What comes once in a minute, twice in a moment, but never in a thousand years?
4) I am an odd number. Take away one letter, and I become even. What number am I? brain teasers such as these are excellent ways to challenge your brain and hone your thinking skills. How many do you think you could solve? Let us know!
Answers
1) There are only three people—grandfather, father, and son. The father is both a son and a father
2) The man in the photo is his son
3) The letter "M"
4) Seven (remove the "S" and you get "even")
Surgeons Transplant First-Ever Gene-Edited Pig Lung Into A Brain-Dead Man

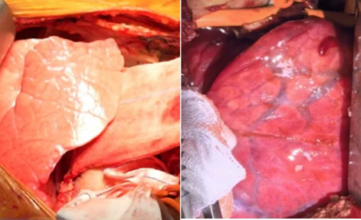
Credits: Health and me
In a breakthrough that will possibly redefine the future of organ transplantation, a team of surgeons in China have successfully performed a transplant using a genetically modified pig lung into the chest of a 39-year-old brain-dead man. The lung functioned for nine days and opened up unprecedented insights into xenotransplantation, the practice of transplanting animal organs into humans. Although the experiment was short-lived, it has ignited hope to amass the millions left waiting each year for life-saving transplants.
For decades, the worldwide shortage of donor organs has stranded millions waiting for a life-giving transplant that might never occur. In the United States alone, over 103,000 individuals were waiting in line for an organ transplant in 2023, but fewer than half received one. Each day, approximately 13 patients die while waiting. And now, an experimental procedure from China is testing the limits of science: for the first time, surgeons have implanted a genetically engineered pig lung into a human.
The recipient, a 39-year-old male who was declared brain-dead following a hemorrhage, survived for nine days with the transplanted lung before the experiment was terminated at the request of his family. Although the organ did not survive long-term, the procedure represents a dramatic advance in xenotransplantation, the utilization of animal organs in humans.
On May 15, 2024, a surgical team at the First Affiliated Hospital of Guangzhou Medical University performed the historic surgery. The donor organ was taken from a genetically modified miniature pig with six CRISPR edits intended to render it compatible with human biology. The edits silenced three pig genes that induce immune rejection and introduced three human genes that control inflammation and immune response.
The lung was carefully transplanted into the man's chest; the other lung was left intact to support function. Over the following hours, the medical team watched for signs of "hyperacute rejection," the immediate and catastrophic immune response that usually destroys foreign organs within minutes. To their surprise, this did not occur.
But soon difficulties arose. By the 24-hour mark, the new lung began to develop inflammation and fluid retention. By day three, there was antibody-mediated rejection. Although there were initial indications of stabilization, the transplant lung was unable to combat the overwhelming immune response. On day nine, in accordance with family desires, physicians discontinued the experiment.
Why Lungs Are Harder to Transplant?
While kidneys and hearts have challenges to overcome in transplantation, such as size matches, lungs have their own set of challenges. Their intricate structure, suited for oxygen and carbon dioxide exchange, predisposes them to injury and inflammation. In addition, lungs are the only transplanted organ completely exposed to the external environment — each breath introduces bacteria, viruses, pollen, and toxins that the immune system needs to screen out.
Achieving the balance between suppressing the immune system sufficiently to avoid rejection but not so much that the patient is lethally susceptible to infection has been one of medicine's most formidable challenges. Indeed, repeated success with human-to-human lung transplants was only made possible in the 1980s, two decades after kidney and heart surgery had been successfully accomplished. Introducing cross-species transplantation into the equation yet again increases the science's complexity.
The Global Organ Shortage Crisis
The World Health Organization has projected that only 10% of the world's demand for organ transplants is now being filled. In the United States, the supply-demand gap increases yearly even with attempts to raise donor registration levels. With developments in organ preservation and sharing networks, still thousands of patients never receive the opportunity for an operation.
This is where xenotransplantation may revolutionize things. Pigs have emerged as the animal donor of choice due to their organ size, physiological proximity to humans, and ease of genetic modification. Pig heart valves have been successfully implanted in humans for over 30 years. Genetically altered pig kidneys and hearts have been transplanted into human recipients more recently with varied degrees of short-term success.
Historical Timeline of Xenotransplantation Milestones
Over the last few years, there have been a proliferation of milestone procedures that have registered global attention:
- In 2022, American surgeons implanted a genetically altered pig heart into a living patient, who lived for two months.
- Last January 2024, a Massachusetts man received a genetically altered pig kidney and remains alive with the organ functioning.
- Chinese scientists tried to transplant a pig liver into a brain-dead patient, results being limited.
The pig lung transplant represents a new frontier, pushing the boundaries of xenotransplantation research. Every effort gives valuable information regarding how animal organs respond in humans and what the largest hurdles are.
What Makes This Pig Lung Different?
The pig lung utilized in the Guangzhou experiment was obtained from a Bama miniature pig kept in a pathogen-free facility by Clonorgan Biotechnology based in Chengdu, China. This provided the assurance that the animal was not exposed to infections that would otherwise be passed on to the human recipients.
It is the CRISPR alterations that rendered this experiment possible. By deleting pig genes for sugars identified as "foreign" by the human immune system and adding human immune-regulating proteins, researchers sought to "humanize" the lung. Although the rejection reaction still happened, the failure of hyperacute rejection — long the most immediate hurdle — to occur indicates that gene editing is closing the gap.
What Are The Medical and Ethical Challenges Beyond This Medical Miracle?
Despite this milestone, experts caution that pig lungs won’t be saving lives in hospitals anytime soon. The risks of infection, rejection, and long-term complications remain significant. In addition, the ethical considerations of using animal organs, particularly genetically modified ones, are far from resolved. Critics argue that resources might be better invested in advancing bioengineered or lab-grown organs rather than relying on animals.
But to patients presented with the stark reality of organ deficiencies, the prospect of a limitless alternative source is difficult to resist. Families who agree to such experimental surgeries do so in the belief that their contribution will help pave the way for a future where others will not have to wait in vain.
The results of the Guangzhou team, reported in Nature Medicine, highlight both the potential and dangers of xenotransplantation. Though rejection is still the biggest obstacle, the advancements within a few years are remarkable. What was previously considered science fiction is slowly becoming a reality, though through industrious trial and error.
For the time being, lung xenotransplantation is an experimental frontier and not a clinical option but as genetic engineering progresses and our understanding of immune regulation becomes more profound, it may one day be able to assist in revolutionizing transplantation medicine. If researchers can one day bypass the immune system's hurdles, the 103,000 individuals already on the US transplant waiting list and hundreds of thousands worldwide may at last have new hope.
Strange Covid-19 'Razor Blade' Symptom That Has US Doctors Shocked: It Starts With This Common Sign

(Credit-Canva)
Medical officials are warning about a big jump in COVID-19 cases. This increase is being caused by a new version of the virus, which people are calling "Razor Blade COVID." The reason for this name is because its main symptom is a sore throat that feels incredibly painful, almost like swallowing razor blades. In some areas, doctors are seeing as many positive tests this month alone as they did during the previous three months combined.
What Is The New 2025 Covid Symptoms?
This new type of COVID-19 is part of the Omicron family and has been spreading across the country for a while, but cases are now climbing in one particular state. Many people who get sick with it are surprised when they test positive for COVID because they thought they just had strep throat or another common illness. If you suddenly get a really bad sore throat along with other flu-like symptoms, it's a good idea to take a COVID test at home. If that test is negative, you should see a doctor to check for other problems like strep or mono.
Who Needs To Take Covid Precautions?
With students back in classrooms, it’s normal to see more sickness going around. However, the same simple rules for preventing the spread of COVID still apply. Health experts continue to recommend that everyone stay up to date on their COVID booster shots. Here are some key steps to take for your safety.
- Stay home if you are sick.
- Wear a mask while recovering from illness.
- Cough into your elbow to prevent the spread of germs.
While COVID-19 is likely here to stay, experts adds that we have the knowledge and tools to manage it. He encourages people to know when to get tested and when to seek medical help.
What Are The 3 New Symptoms of Covid 2025?
The good news is that the symptoms of the new "Stratus" variant are similar to other recent types of Omicron. This means you don't need to learn a whole new list of symptoms. They are often like those of the common cold or flu and can include:
- Fever, coughing, and a runny nose
- Headache or body aches
- In some cases, stomach issues like nausea or diarrhea
If you feel sick and test positive, it’s a good idea to let people you've been in contact with know. For most people, symptoms will go away on their own with rest, fluids, and over-the-counter medicine. However, if symptoms get worse or don't go away, you should see a doctor.
How Can We Stay Protected From COVID 2025?
Even with the new variant, health experts are not overly concerned because most people in the U.S. have some protection from either a previous infection or vaccination. Our bodies have special "memory" cells that can recognize and fight off new variants, which helps prevent severe illness.
However, some people are at higher risk. The CDC recommends that adults over 65, people with certain health conditions, and those with weakened immune systems stay up-to-date on their COVID-19 vaccines. While vaccine policies have recently changed, experts still agree that vaccination is the best way to protect yourself from getting seriously sick.
22-Year-Old Woman Dies Due To Allergic Reaction After the Routine CT Scan

(Credit-Canva)
A young woman, 22-year-old Leticia Paul, sadly passed away following a severe allergic reaction to a special dye, called a contrast agent, used during a CT scan. This tragic event happened on Wednesday, August 20, at the Alto Vale Regional Hospital in Rio do Sul, Brazil. Reports say that during the scan, Leticia experienced anaphylactic shock. This is a sudden, extreme, and very dangerous allergic reaction that can cause a person's throat to close up, making it hard to breathe, and their blood pressure to drop dangerously low.
What Caused Her Allergic Reaction?
Reports show that her allergic reaction was to ‘contrasting agents’ used in a CT scan. According to Radiologyinfo, for Patients, doctors use special liquids called contrast agents to make organs and blood vessels stand out in medical scans like CT or MRI. These are not permanent dyes; they're temporary substances that help highlight specific body parts, making it easier for doctors to find and diagnose problems. They can be swallowed, injected, or given rectally and are naturally cleared from the body afterward.
What Is Anaphylactic Shock?
According to the UK National Health Services, anaphylaxis is a very serious and fast-acting allergic reaction. It's an emergency that happens when your body overreacts to something it's allergic to, like certain foods, medications, or insect stings. This reaction can be so severe that it becomes life-threatening.
Following the allergic reaction, Paul was intubated at the hospital. Her aunt, Sandra Paul, confirmed to local news outlets that her niece died less than 24 hours later, on Thursday, August 21. Sandra Paul also shared that her niece had a history of kidney stones and was undergoing a routine checkup at the time of the incident.
Also Read: What Does Finn Wolfhard's Journey Highlight About Young Stars Dealing With Mental Health Issues?
How To Recognize An Anaphylactic Shock – First Symptoms
The signs of anaphylaxis appear very suddenly, usually just minutes after coming into contact with the substance you're allergic to. The symptoms can be different for everyone, but here are the most common things to look out for:
Swelling
A major sign is swelling, especially in your throat or on your tongue.
Breathing Problems
Anaphylaxis can make it hard to breathe. You might start breathing very fast, or you could hear a wheezing sound when you breathe. Your throat might feel tight, making it difficult to swallow, and your voice could become hoarse. You might also have a persistent cough.
Blood Pressure Drop
This is a very dangerous part of the reaction. It can make you feel faint, dizzy, or even cause you to pass out. Your skin might feel cold and clammy, and it can look pale, grey, or even bluish. If you have darker skin, you can often see this change on the palms of your hands or the soles of your feet.
Other Reactions That May Also Happen?
You might also feel very tired or confused, which is another sign that your body is in distress. It’s also common to get a rash that is swollen, raised, and very itchy.
What Are Some Precautions You Should Take For Allergies?
If you suspect you're having an anaphylactic reaction, use your adrenaline auto-injector right away, even if your symptoms seem mild.
It's also a good idea to wear medical alert jewelry, such as a bracelet, that details your allergy. This can provide crucial information to others in an emergency. Finally, do not store your adrenaline auto-injectors in places that are too hot or too cold, like a refrigerator or in direct sunlight.
© 2024 Bennett, Coleman & Company Limited



