- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
257 Active Cases of COVID-19 In India - What Is The New Strain And Safety Guidelines To Follow?

(Credit-Canva)
With cases rising in countries like Singapore, Hong Kong, China and Thailand experts have warned against the new JN.1 variant of Omicron, which is causing the current spike. The new COVID wave has highlighted the JN.1 variant of Omicron, which is causing the current spike in the numbers. With 257 active cases in India, the conversation regarding safety, new guidelines and health concerns have begun.
Initial Rise In COVID-19 Cases
The infections in Singapore increased to over 14,000 in early May, when previously the numbers had been 11,100 in the last week of April. This rise in numbers was due to the two subvariants of JN.1 namely LF.7 and NB.1.8. Experts have mentioned that India could face a similar wave as the immunity of the population decreases.
Currently, in India, while the situation is nor dire, more cases are being reported. Kerala has the most cases with 69, followed by Maharashtra with 44, and Tamil Nadu with 34. Other states such as Karnataka, Gujarat, Delhi, Haryana, Rajasthan, and Sikkim have also reported new infections. The two COVID-19 related deaths have been confirmed at KEM Hospital in Mumbai, causing some concern locally in that area. However, an important thing to note is that these cases had previously confirmed critical illnesses, one patient suffering with nephrotic syndrome, while the other was a cancer patient.
Health experts from important groups like the Indian Council of Medical Research (ICMR) and the National Centre for Disease Control (NCDC) have stated that India's overall situation is still under control.
What Is JN.1 Variant of Omicron?
According to John Hopkins Bloomberg School of Public Health, a new variant called JN.1 has emerged. It's a "child" of BA.2.86. JN.1 has one or two new mutations that are able to surpass immunity and are thus spreading easily.
COVID-19 variant called BA.2.86, which is a sub-variant of Omicron appeared in late 2023. Scientists noticed it because it had around 30 more changes, or mutations, in comparison to other variants. These mutations helped it to better avoid our body's defenses, or immunity.
However, BA.2.86 never became the most common variant in late summer or early fall of 2023.
What Are The Symptoms of JN.1 COVID Strain?
The symptoms observed in the current COVID-19 wave differ slightly from earlier strains. While cough and sore throat remain prevalent, new symptoms include nausea, vomiting, brain fog, and eye irritation (conjunctivitis). The JN.1 variant, specifically, presents symptoms similar to previous COVID-19 strains like dry cough, fever, sore throat, fatigue, and loss of taste or smell, but reports from institutions like Johns Hopkins suggest it may be more likely to cause gastrointestinal issues, especially diarrhea.
Do We Need Booster Shots For Safety?
Even though the current number of cases is low, it's really important to keep watching the situation closely. According to the New England Journal of Medicine, the U.S. has recommended yearly COVID-19 boosters for almost everyone, unlike Europe which limits recommendations to older or high-risk individuals. However, many Americans and healthcare workers haven't been getting these boosters, and general trust in vaccines is falling.
Moving forward, the FDA is changing its approach. They will approve COVID-19 vaccines for those over 65 and anyone over 6 months old with high-risk health conditions, based on how well the vaccine helps the body create antibodies. For healthy people aged 6 months to 64 years, the FDA will require more rigorous studies (randomized controlled trials) to show the actual clinical benefits before approving boosters.
State Of COVID –19 Globally
Around the world, Singapore has seen a 28% jump in its weekly COVID-19 cases. Hong Kong also recently reported 31 COVID-related deaths, which is its highest number in a year. Experts are advising people in India to be careful. They are urging everyone to follow safety rules, especially in crowded or risky places, to avoid any problems.
Core Preventive Strategies For COVID-19
While there have been no urgent changes to the guidelines regarding preventive measures of covid, here are the core strategies for prevention one must partake in according to the Centers Of Disease Control and Prevention.
Stay current on COVID-19 vaccines, practice good hygiene, and improve indoor air quality to reduce germ spread. If sick, isolate yourself and know when to safely resume activities. Consider masking and social distancing, and seek prompt medical care if at higher risk for severe illness.
Measles Scare At Shakira Concert: Can Infection Spread Through Touch?

Recently Shakira, pop icon, set the stage ablaze at MetLife Stadium on May 15 during her Los Mujeres Ya No Lloran World Tour and the 82,500-seat arena pulsed with energy, light, and fans from all over the country. But within days, a New Jersey health agency warning has cast a foreboding shadow over the night's celebrations.
A concert attendee, recently diagnosed with measles, could have infected thousands of others who gathered in the packed stadium—prompting key questions about public health, immunization, and how measles is spread in close quarters. The question that's now echoing far beyond the stadium entrances: Can measles actually spread by touch?
As per the New Jersey Department of Health, the infected person—a non-state visitor—was at the concert from 7:30 p.m. to 1 a.m. Nobody knows where inside the stadium the person was sitting or how many were directly around them. However, the contagious nature of the measles virus is such that physical proximity is not always required for infection.
Health officials called for an alert telling concertgoers to watch for symptoms and to steer clear of direct trips to health facilities unless they are absolutely necessary, in an effort to avoid spreading more exposure. Instead, they suggested calling healthcare providers first so special precautions can be made.
Can Measles Spread Through Touch?
Measles, or rubeola, is one of the most contagious viruses that have ever been known by science. It is spread mostly by respiratory droplets when an infected individual coughs or sneezes. But wait, there's more. According to the Centers for Disease Control and Prevention (CDC), the virus remains suspended in the air for as long as two hours after an infected individual has vacated the area—and it can also be deposited on surfaces. So to answer your question, yes, measles can spread by touching.
If an individual touches an infected surface—such as a handrail, seat armrest, or bathroom door—and then also touch their eyes, nose, or mouth, they risk infection. This is particularly worrying in places such as concert halls, where tens of thousands of individuals touch communal surfaces within a short period of time.
Perhaps most disturbing is how sneaky the measles virus is. A person infected with the virus can begin to spread the virus four days before the characteristic rash shows up—and continue to spread it for four days afterward. That leaves many people who spread the disease not knowing they are ill, which makes public health responses in crowded events more difficult.
Symptoms may take 7 to 14 days to develop, which is why health officials are calling for alertness at least until June 6. Early measles symptoms mimic the flu: high fever, dry cough, runny nose, and watery, red eyes. The telltale rash—flat red spots beginning at the hairline and spreading downward—may follow later, after the virus has already been spread to others.
Why the Measles Outbreak in 2025 Is Alarming?
The Shakira concert incident isn’t an isolated case. The U.S. is in the midst of its worst measles outbreak in three decades. As of mid-May 2025, the CDC has reported 1,024 cases across 31 states—more than triple the total number of cases in all of 2024. Fourteen distinct outbreaks have been recorded so far this year, and a staggering 92% of cases are connected to these outbreaks. Three people have died.
There are several reasons why a disease believed to be almost eradicated in the U.S. is making a comeback. Among them are decreased vaccination coverage, false information on vaccine safety, and lack of global immunization due to compromised access to healthcare during the COVID-19 crisis.
Who's Most at Risk?
Though measles may infect anyone who is not immune, there are some groups that are particularly susceptible. Those who are too young to be vaccinated with MMR (measles, mumps, and rubella) are at risk, as well as those with weakened immune systems or certain medical conditions that make it impossible for them to be vaccinated. Those who have not been given both doses of the MMR vaccine or who never caught measles are also at greater risk.
The CDC estimates that as many as 90% of non-immune contacts of a patient with measles will become infected.
As of Tuesday, there were no other confirmed cases related to the concert. Nevertheless, health officials are warning anyone who went to the concert and starts showing signs to stay out of public areas and reach out to a healthcare provider right away.
The outbreak has stimulated renewed calls for vaccination and awareness. "This is not an individual health matter but a public health threat," said one CDC official. "Vaccination is our strongest protection, and all who can be vaccinated should be.
The irony isn't lost on many: what was meant to be a unifying event for people around the country might now stand as a national reminder of the residual potency of contagious disease—and the value of public health vigilance.
While Shakira's tunes will ring on in the ears of fans, the possible health effect of the night might resonate much further. As the tale is told, it is a wake-up call and also a chance to reiterate the value of vaccination, early diagnosis, and safe conduct during possible epidemics.
World’s First Gonorrhoea Vaccine Rolled Out In England Amid STI Surge- How Does It Help In Treatment?
In a breakthrough new public health initiative, England will be the world's first country to implement a vaccine against gonorrhoea—a milestone in the battle against sexually transmitted diseases (STIs) and antibiotic resistance. The UK's National Health Service (NHS) has announced that from August 1, 2025, there will be a phased deployment of the vaccine to England through local sexual health services.
The programme, hailed as a “landmark moment for sexual health,” arrives amid a worrying surge in gonorrhoea cases and increasing concerns over drug-resistant strains. So, who qualifies, how effective is the vaccine, and what does this mean for STI prevention globally? Here's a detailed breakdown.
Gonorrhoea is the second most prevalent bacterial STI in the UK, and it's increasing. England reported more than 85,000 cases in 2023—the highest ever since records started in 1918. Although gonorrhoea can be treated with antibiotics, the bacteria responsible for it—Neisseria gonorrhoeae—have increasingly developed resistance to first-line treatments like ceftriaxone, threatening the prospect of untreatable infection.
Symptoms of gonorrhoea may vary from discharge and dysuria to lower abdominal pain and rectal pain. However, most individuals remain asymptomatic and spread the infection unknowingly. With increasing transmission rates among high-risk groups, the imperative for preventive measures has never been more evident.
What is The New Vaccine for Gonorrhoea?
Astonishingly, the gonorrhoea vaccine is not a new invention. It is called 4CMenB and is already used to give protection against meningococcal group B disease, a severe bacterial illness that causes meningitis and sepsis. The vaccine is included in the UK schedule for routine childhood immunization and is given at eight weeks, 16 weeks, and one year old.
How Does It Protect Against Gonorrhoea?
The vaccine includes proteins of Neisseria meningitidis—the causative agent of meningitis—which are genetically close to Neisseria gonorrhoeae. Such cross-reactivity is considered to provide immunity to some extent against gonorrhoea. The UK's Joint Committee on Vaccination and Immunisation (JCVI) studies estimate it to be 32.7% to 42% effective. It is no silver bullet, but it's a major breakthrough in STI prevention given that previous infection with gonorrhoea provides minimal or no immunity.
Who Is Eligible for the Vaccine?
The rollout will not be universal—at least for now. Rather, it will focus on groups who are most vulnerable. These include gay and bisexual men who have had multiple sexual partners or have a history of previous STIs. The people who qualify will be invited by local sexual health services and vaccinated from this August.
Along with the gonorrhoea vaccine, patients will receive mpox (previously monkeypox), human papillomavirus (HPV), and hepatitis A and B immunizations—completing an all-encompassing STI prevention package.
The vaccine rollout is not merely about cutting down on infections—it's also a pre-emptive move against antibiotic-resistant gonorrhoea. Between January 2024 and March 2025, the UK Health Security Agency (UKHSA) noted 17 instances of ceftriaxone-resistant gonorrhoea, of which nine were extensively drug-resistant (XDR). These statistics are worrying and highlight the necessity of non-antibiotic alternatives to infection control.
As Dr. Amanda Doyle, NHS England's national director of primary care and community services, put it, "This rollout is a big step forward. Not only will it keep people safe, but it also prevents the spread of resistant bacteria—one of the biggest threats to medicine today."
If uptake is high, projections from Imperial College London suggest the programme could prevent over 100,000 cases and save the NHS nearly £8 million over the next decade. But its success could reverberate well beyond the UK. Other nations—including Scotland and Northern Ireland—are already evaluating similar plans. Should the vaccine prove successful, it could pave the way for global STI immunization strategies.
However, experts caution that unknowns exist. How long does immunity last? Will booster shots be needed? As the data rolls in in the real world after launch, these questions will hopefully be answered.
Can STIs Be Prevented Through Vaccines?
The gonorrhoea vaccine is part of a small but expanding list of immunizations to prevent STIs. To date, there are highly effective vaccines for HPV, hepatitis A, and hepatitis B. These are administered routinely to risk groups and have greatly decreased infection where they have been introduced.
But vaccines against bacterial STIs such as chlamydia and syphilis are still out of reach, and there is no vaccine for HIV or hepatitis C. Prevention must continue to rest on safe sex habits, routine screening, and antibiotic therapy—so the arrival of the gonorrhoea vaccine is an important step in filling an enormous gap in sexual health protection.
Although not a magic bullet, the first ever gonorrhoea vaccine programme is a public health triumph. And by being the first nation to introduce such an initiative, England is pioneering a move that has the potential to revolutionise STI prevention worldwide.
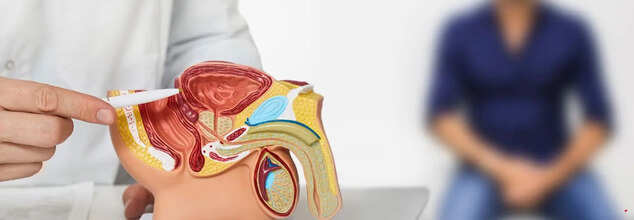
5 Early Symptoms Of Prostate Cancer That Shouldn't Be Overlooked
Credit: Canva
Former US President Joe Biden's office confirmed on Sunday that he has been diagnosed with prostate cancer. Earlier, a small nodule was found in his prostate gland, however, not much had been revealed about his medical evaluation. It was last week when Biden went to see the doctors after urinary symptoms, and a prostate nodule was found. He was then diagnosed with prostate cancer on Friday, with the doctors revealing that the cancer cells have spread to the bone.
Last month, Former Deputy PM of Australia and Nationals MP Barnaby Joyce said that he had been diagnosed with prostate cancer. Joyce, who was recently re-elected to his New England seat, underwent surgery following the diagnosis. This is not it, earlier in February, British monarch King Charles III was diagnosed with enlargement of his prostate glands (also known as benign prostatic hyperplasia (BPH), for which he was treated. While undergoing treatment for this condition, he was also diagnosed with cancer. The cancer was not prostate cancer but was discovered during the course of treatment for the enlarged prostate.
So are there any signs and symptoms of prostate cancer that can go ignored? According to health experts, the answer is yes. Here's a list of symptoms that must be paid attention to:
Frequent Urination, Especially at Night: An increased need to urinate, particularly during nighttime hours, can be an early indicator. This symptom may be overlooked or attributed to ageing or other benign conditions.
Difficulty Starting or Stopping Urination: Experiencing trouble initiating or halting the flow of urine might suggest prostate issues. This can be subtle and often goes unnoticed until it becomes more pronounced.
Weak or Interrupted Urine Flow: A decrease in the strength of the urine stream or a flow that starts and stops can be a sign of prostate enlargement or cancer. Men may dismiss this as a normal part of ageing.
Blood in Urine or Semen: The presence of blood in urine or semen is a more noticeable symptom, but can still be overlooked or attributed to other causes. It's essential to consult a healthcare provider if this occurs.
Persistent Pain in the Lower Back, Hips, or Thighs: Ongoing discomfort or pain in these areas may indicate that prostate cancer has spread. Such pain is often mistaken for muscle strain or arthritis.
What Do We Know About Prostate Cancer?
Prostate cancer is a type of cancer that occurs when malignant cells form in the prostate gland, which is a walnut-sized gland in the male reproductive system. Prostate cancer treatment guidelines have shifted their path a bit in recent years, with many men opting for active surveillance rather than immediate treatment for slow-growing tumours. However, about 50% of men on "watchful waiting" will require further treatment within 5 years because of the tumour progression.
© 2024 Bennett, Coleman & Company Limited

