- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
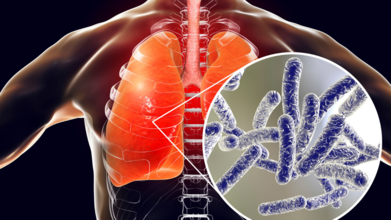
Legionnaires' Outbreak: Death Toll Increases To 6 With 111 Hospitalized, How To Spot The First Symptoms
(Credit-Canva)
A sixth person has died from the Legionnaires’ disease outbreak in Central Harlem, according to New York City health officials. The city is currently investigating the outbreak that began in late July, which has now affected over 100 people.
As of Thursday, 111 people have been diagnosed with the disease. The recent death was of a person who passed away outside of New York City earlier this month, but their death was only recently linked to the outbreak. There are currently seven people hospitalized.
The city has identified and cleaned 12 cooling towers on 10 buildings, including a city hospital and a clinic, where the bacteria were found. These cooling towers, which use water to cool buildings, are believed to be the source of the outbreak.
What is Legionnaires' Disease?
Legionnaires' disease is a severe type of pneumonia caused by a bacteria called Legionella. This bacteria thrives in warm water and can spread through a building’s water system. People usually show flu-like symptoms, such as a cough, fever, and muscle aches, within two days to two weeks after they are exposed to the bacteria.
Health officials are advising anyone who lives or works in the Central Harlem area to contact a doctor if they experience these symptoms.
What Are The First Symptoms of Legionnaires’ Disease?
The disease often starts like a mild flu. For the first couple of days, you might have muscle aches, body aches, and headaches. But after this initial phase, the symptoms get much worse.
You might develop a high fever of 100.4°F or higher, along with chills and extreme tiredness. About half of the people who get sick also experience confusion or delirium. Other symptoms include an upset stomach, with nausea, vomiting, and diarrhea. Since the bacteria attack the lungs, you will likely have a persistent cough that can start out dry but may later produce mucus or even blood. You may also feel short of breath and have chest pain.

How Long Does It Take For Symptoms To Show Up?
The time it takes for you to get sick after being exposed to the Legionella bacteria is called the incubation period. It can be as short as two days or as long as 19 days. Most people, however, start feeling sick around six to seven days after they've been exposed. This is the time the bacteria need to grow inside your body before they cause noticeable symptoms.
What is Pontiac Fever?
Pontiac fever is a milder version of the same infection. Its incubation period is much shorter, usually just one to two days. The symptoms are less severe and include a flu-like sickness with muscle pain, headaches, and a fever. Unlike Legionnaires' disease, Pontiac fever usually goes away on its own without needing a lot of medical care. Because it is so mild, doctors sometimes don't even realize it's Pontiac fever.
How is Legionnaires’ Disease Diagnosed?
Doctors can figure out if you have Legionnaires’ disease using a few different tests. They will often check your blood and urine or look for the bacteria in a sample of your sputum (the mucus you cough up). They may also take a chest X-ray, but this can be tricky because the results look like other types of pneumonia.
The best way to get a clear diagnosis is through lab tests that can directly identify the bacteria. It's also a clue that you have it if your illness doesn't get better with common antibiotics like penicillin. Without treatment, the illness can get much worse and may lead to serious problems like kidney failure, respiratory failure, and even death.
Andhra Pradesh May Ban Social Media for Under-16s To Protect Teenagers

Credit: Canva
Andhra Pradesh may soon follow Australia's steps and ban social media for teenagers under the age of 16 in the state.
Nara Lokesh, Information Technology, Electronics and Communications, Real Time Governance and Human Resources Development Minister for Andhra Pradesh, told Bloomberg at the World Economic Forum 2026 Annual Meeting in Davos, Switzerland: "As a state, we are studying Australia’s under-16 law, and yes, I believe we need to create a strong legal enactment.
"Youngsters below a certain age should not be on such platforms, as they do not fully understand the content they are exposed to. Thus, a strong legal framework may be required."
Also Read: Chikungunya Spreads Across Tamil Nadu: All You Need To Know
TDP national spokesperson Deepak Reddy supported Lokesh's claim and stated: "Children below a certain age are not emotionally mature enough to comprehend the negative and harmful content that is freely available online. That is why the Andhra government is studying global best practices and examining Australia's under-16 social media law."
If implemented successfully, Andhra Pradesh would be the first Indian state to issue the ban and could pave the way for other states to consider such policies. State officials are yet to clarify when the rule will be implemented and if any fines will be attached to it.
Is Any Other State Considering a Ban?
While hearing a write petition in December 2025, the Madras High Court has asked the Union Government to look for possibilities in passing a legislation similar to the ban of under 16s using social media.The petition was to emphasize on the awareness of the stakeholders and parental windows in the device that could control the menace of pornographic material which is easily accessible to children. The court asked Centre to order internet provider service companies to provide a 'Parental Window' to prevent children from accessing such content.
The Madurai Bench of Justices G Jayachandran and KK Ramakrishnan told the authorities of child rights to accelerate this matter. The bench also noted that children could only be prevented from consuming such content only if there is a parental control app on the device.
Judges also noted that parents have a higher responsibility in this, as children are highly vulnerable to such content.
READ MORE: Australia Social Media Ban Explained: Why Government Plans to Restrict Accounts of Under-16s
What Did Australia Do?
To protect the mental health of children, Australia has successfully banned several social media apps including Facebook, Instagram, Snapchat, Threads, TikTok, X, YouTube, Reddit, and streaming platforms Kick and Twitch.
YouTube Kids, Google Classroom and WhatsApp are not covered under this rule as they do not fit those criteria.
While anyone under 16 will be still able to watch most of the content without logging in, however, they cannot have an account on it. Critics are urging the government to widen the ban to include online gaming platforms such as Roblox and Discord, which are currently not covered.
The government says that it will also reduce the negative impact of social media's "design features that encourage [young people] to spend more time on screens, while also serving up content that can harm their health and wellbeing".
A government study which was commissioned in 2025 found that 96% of children aged 10 to 15 used social media, and that seven out of 10 of them were exposed to harmful content. These content were misogynistic and violent in its nature, furthermore, content promoted eating disorders and suicide.
Children and parents will not be punished for infringing the ban, instead, social media companies will face fines of up to A$49.5m, which is equivalent of US$32m for serious or repeated breaches.
Chikungunya Spreads Across Tamil Nadu: All You Need To Know

Credit: Canva
The Directorate of Public Health and Preventive Medicine (DPH) has issued a statewide alert across Tamil Nadu due to a sudden uptick in chikungunya cases in multiple cities.
Cases have been reported across Chennai, Villupuram, Tenkasi, Theni, Cuddalore, Chengalpattu, Kancheepuram and Ariyalur. It remains unknown how many people have been affected and if any deaths have occurred.
Caused by the chikungunya virus, chikungunya virus disease (CHIKVD) is spread by the bite of infected mosquitoes (Aedes aegypti and Aedes albopictus) to humans. The illness usually starts with flu-like symptoms including fever, chills, headache, nausea, vomiting, joint pain and rashes.
Also Read: This Is Why Emmanuel Macron Wore Sunglasses At Davos
Typically, the illness has no clear no symptoms, especially in children and can easily be misdiagnosed as dengue and Zika. While there are no specific antiviral treatments for chikungunya virus infections, medications such as antipyretic and analgesic medications (such as paracetamol) for fever and pain can be used to ease the pain.
Most patients recover completely from the infection, but occasional cases of eye, heart, and neurological complications have been previously been reported with CHIKV infections.
What Are Tamil Nadu Officials Doing To Contain Cases?
To improve virus containment, health officials across the state have been instructed to collect sufficient blood samples in fever-prone areas and ensure laboratory confirmation using IgM ELISA tests, which can detect recent or acute viral infections.Authorities have also emphasized that all government and private hospitals as well as diagnostic laboratories, need to timely report cases to ensure the infection does not spread . Any delay in reporting, officials noted, could allow the virus to spread rapidly within communities.
On the local level, district entomologists and health inspectors have been told to eliminate stagnant water in artificial containers and conduct weekly mass-cleaning drives in high-risk areas.
The DPH has also ordered that all designated dengue and chikungunya wards in hospitals be kept mosquito-free, with adequate bed strength and sufficient mosquito nets for patients.
READ MORE: What Is Chikungunya And How Can It Be Prevented?
Can Chikungunya Spread Easily?
While the illness does not spread directly from person-to-person through touching or coughing; however, in some rare cases, mother-to-baby transmission during childbirth is possible and infected individuals should avoid further bites to prevent spreading the virus.Cases typically emerge mostly in the Americas, Asia and Africa and occasionally in Europe. However, nearly 30,000 CHIKVD cases have been recorded, including 83 associated deaths from 12 countries namely from China, Singapore, Pakistan, France, Argentina, Brazil and Mexico, marking it as one of the biggest outbreaks in the world.
This Is Why Emmanuel Macron Wore Sunglasses At Davos

Credits: AP
French President Emmanuel Macron on Tuesday addressed the World Economic Forum in Davos, Switzerland. As he spoke on the European solidarity amid US President Donald Trumps' treat to annex Greenland, something else seemed to take the attention away. Macron was seen wearing a pair of blue-tinted mirrored aviator sunglasses. The surprising part was that he wore it indoors. French media had already reported that he was seen wearing sunglasses since last week.
Trump also mocked Emmanuel Macron’s sunglasses during his speech at Davos, joking, “what the hell happened?” regarding the French president’s appearance.
Also Read: Nipah Virus Outbreak In India: After Two West Bengal Cases, Tests On Bats Show No Active Infection
Why Was Emmanuel Macron Wearing Sunglasses Indoors?
On Monday, Macron said that reflective glasses were to disguise a minor eye injury that he had sustained after having been spotted with a heavily bloodshot right eye. "Apologies for the shades, but I have to wear them for a while". He further said that it is for a "mild eye condition".
Last week, when he appeared at a military event in southern France with red eye, while addressing the troop, he said, it was "totally benign" and "completely insignificant", he also added, "Please pardon the unsightly appearance of my eye". He also joked about it, calling it "l'oiel du tigre" or the "eye of the tiger". This was a reference to rock band Survivor's song used in the 1982 boxing moving Rocky III. He said, "For those who get the reference, it is a sign of determination".
What Happened To Macron's Eyes?

As per the French media reports, Macron appeared to have a sub-conjunctival hemorrhage. This means there is a broken blood vessel in his eyes. It is harmless, painless, and does not affect the vision. It also cannot cause permanent injury to the eye, and clears within a fortnight.
Macron Wears Sunglasses Indoor: Is It Absolutely Necessary?
Medical doctor and media commentator Jimmy Mohamed told French broadcaster RTL that Macron "opted for this style for aesthetic reasons, because he is a public figure. However, sunglasses are not necessary to protect vision in this condition. Some people wear it to avoid attracting attention.
"Some people might think he's ill, so to avoid being photographed in that state, he decided to wear sunglasses. The glasses protect his image, but not really his eye," said Jimmy Mohamed.
Read: Why Can't I Hear When I Take My Glasses Off?
How Have Netizen Reacted To Macron Wearing Sunglasses?
He has been called 'kéké', which is a French slang for a show off. Others also joked about him being a "cyborg" or emulating Hollywood actor Top Cruise in Top Gun, the 1986 movie that made wearing aviators a fashion statement.
What Is Sub-conjunctival hemorrhage?
Sub-conjunctival hemorrhage or SCH is a common ocular condition defined by extravasation of blood beneath the conjunctiva, producing a sharply demarcated red patch on the scleral surface. The condition is usually painless and does not impair vision. It usually resolves within 1 to 2 weeks, making it a frequent but benign cause of ocular redness.
It usually happens by a sudden pressure increase from coughing, sneezing, vomiting, or heavy lifting. This could rupture tiny eye blood vessels, or from eye trauma like rubbing or foreign bodies, and can be linked to risk factors like high blood pressure, diabetes, blood thinners, or even childbirth in newborns.
© 2024 Bennett, Coleman & Company Limited

