- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Valley Fever Cases Surge In California-How To Identifiy This Lung Infection
Credit: Canva
California may be heading toward another record year of Valley fever infections, with early 2025 data already showing a troubling increase in reported cases. Health officials have confirmed over 3,100 infections across the state—figures that surpass last year’s numbers for the same period and nearly double those recorded in 2023.
Valley fever, medically known as coccidioidomycosis, is a serious lung infection caused by the Coccidioides fungus, which thrives in the dry, dusty soils of the western U.S. California, where the disease was first identified, consistently reports the highest number of cases nationwide. If left untreated, the illness can lead to severe, long-term respiratory issues and even death if it spreads to the brain.
“There is no question that the number of cases is enormously higher than before,” said Dr. Royce Johnson, director of the Valley Fever Institute at Kern Medical. “If you want to see me, you’d have to wait until July, and that goes for my colleagues, too,” he told NBC News, highlighting the growing strain on healthcare systems in affected regions.
The majority of recent infections have been reported in Kern, Los Angeles, Monterey, and Fresno counties—areas long known as hotspots. But the illness is now expanding its reach. In Contra Costa County, located in the East Bay region, cases have tripled compared to 2023. Nearby Merced and San Bernardino counties are also reporting significant spikes.
“It appears to be spreading out,” noted Gail Sondermeyer Cooksey, an epidemiologist with the California Department of Public Health.
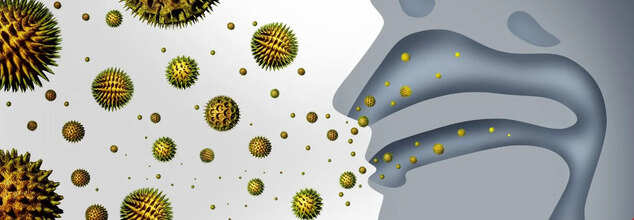
Valley fever infections occur when people inhale spores released into the air from soil containing Coccidioides. These spores can be stirred up by wind, construction, and agricultural activities. While anyone can get infected, those most at risk include people over 60, individuals with weakened immune systems, pregnant women, diabetics, and those of Black or Filipino descent. Outdoor workers also face higher exposure.
Symptoms typically resemble those of the flu and may include fatigue, cough, fever, shortness of breath, and skin rashes. While most recover, about 10 percent develop chronic lung issues, and approximately 1 percent experience dissemination of the infection to the skin, bones, joints, or brain.
Health experts also point to a concerning link between climate change and the disease's rising prevalence. Shifts from prolonged drought to intense rain—common in California’s recent weather patterns—create favorable conditions for the fungus to grow and later release spores as the land dries.
“As climate change alters the timing and intensity of precipitation in California, we see longer high-risk periods for Coccidioides exposure,” said Simon Camponuri, a PhD researcher at the University of California, Berkeley.
With forecasts predicting a hot and dry summer following recent floods and mudslides, health officials are bracing for continued spikes in Valley fever cases in the coming months. Public health campaigns are urging increased awareness, especially among vulnerable populations and those living in high-risk regions.
Childhood Obesity In India To Surge To 56 Million By 2040, Says Global Report

Credit: Canva
Childhood obesity in India is expected to surge to a whopping 56 million by 2040 -- nearly a 20 percent rise from 2025, according to an alarming new global report released today by the World Obesity Federation.
The World Obesity Atlas 2026, released on World Obesity Day -- observed globally on March 4 -- revealed that of the 56 million, about 20 million children in the country will be obese, while the remaining will be overweight.
Globally, the number of children aged 5-19 years living with obesity or overweight is predicted to increase to 507 million by 2040 -- from 419 million in 2025.
Overweight Children: India Second-Highest Globally In 2025
Among children aged 5-9 years, 14.921 million were overweight or obese in 2025
In children aged 10-19 years, more than 26.402 million were overweight or obese.
India was among the top 10 countries -- second after China -- that accounted for over 200 million school-age children, aged 5-19 years, with high Body Mass Index (BMI).
Between 2010 and 2025, India had a 4.8 percent increase in the prevalence of high BMI and obesity among children aged 5-19 years.
"The increase in childhood obesity worldwide shows we have failed to take seriously a disease that affects one in five children," said Johanna Ralston, chief executive at the World Obesity Federation.
"Governments urgently need to step up prevention and management efforts for children living with overweight and obesity, and ensure that they receive the care they need," Ralston added.
High BMI To Surge Chronic Disease By 2040 In India
By 2040, the report also projected a substantial increase in the risk of diseases among children aged 5-19 years due to a high BMI in India. This includes:
- Hypertension (high blood pressure) expected to spike by 4.21 million from 2.99 million
- hyperglycemia (high blood sugar) to 1.91 million from 1.39 million
- high triglycerides (excess fats in the blood) to 6.07 million from 4.39 million
- metabolic dysfunction-associated steatotic liver disease (MASLD) to 11.88 million from 8.39 million
The key preventable risk factors in the country include:
- 74 percent of adolescents aged 11-17 fail to meet recommended physical activity levels
- Only 35.5 percent of school-age children (primary and secondary) receive school meals
- 32.6 percent of infants aged 1-5 months experience sub-optimal breastfeeding
- 13.4 percent of women aged 15-49 are exposed to high BMI
- 4.2 percent of women aged 15-49 live with Type 2 diabetes
- Children aged 6-10 consume an average of 0-50 ml of sugary drinks per day
Obesity: A Global Health Concern
Globally, the number of school-age children living with obesity now exceeds those living underweight.
Currently, more than one in five (20.7 per cent) 5-19 year-olds worldwide are living with obesity and overweight -- an increase from 14.6 per cent in 2010.
In 2025, about 177 million children aged 5-19 years were living with obesity. The number is expected to jump to 228 million in 2040.
By 2040, the Atlas also predicts that 227 million children aged 5-19 years will be living with obesity compared to 142 million living with underweight.
Notably, most of the world’s school-age children aged 5-19 living with obesity reside in the middle-income countries. By 2040, this is estimated to be as many as 169 million children.
Call To Action
The World Obesity Federation called for strong action to reverse current trends. These include imposing:
- taxes on sugar-sweetened beverages,
- restrictions on marketing to children (including digital platforms), implementation of global physical activity recommendations for children, protection of breastfeeding,
- healthier school food standards,
- integration of prevention and care into primary health systems.
Tamil Nadu Increases Preventative Chickenpox Measures As Cases Rise

Credit: Canva
Tamil Nadu health authorities have ramped up surveillance efforts and implemented preventive and control measures to curb rising chickenpox cases in the state.
The Directorate of Public Health (DPH) and Preventive Medicine has instructed all health officers to intensify active and passive surveillance in all government and private health facilities, schools, colleges and hostels.
They were also directed to ensure that all suspected and confirmed cases are entered into the Integrated Disease Surveillance Programme (IDSP) line list with complete demographic and clinical details.
All medical officers across the state have further been asked to be alert to differentiate chickenpox from other rash illnesses such as measles, rubella, and hand, foot and mouth disease.
This comes weeks after doctors across Pune also warned against the exponential rise in chickenpox cases this winter.
Dr Shirish Kankariya, head of paediatrics at Apollo Hospital Swargate, said he had seen around 15 chickenpox patients in Jan alone, and the current season has brought a visible uptick in cases.
"Chickenpox cases have risen. We are also seeing infections in older children and adult family members, who never had the disease earlier," he told Times of India.
Dr Prateek Kataria, consultant pediatrician and neonatologist at Sahyadri Hospital also noted that out-patient departments (OPDs) have recently seen a large increase confirmed chickenpox cases this year.
He also told the publication: "We are seeing many children with chickenpox in the OPD even among those who have taken both doses of the vaccine. This is expected because the vaccine does not guarantee 100% protection, but vaccinated children usually develop milder illness and do not need hospitalization."
What Is Chickenpox And How Does It Spread?
Chickenpox, caused by the varicella-zoster virus, is extremely contagious and spreads through respiratory droplets or direct contact with someone who is infected. In children, it often starts as a mild rash accompanied by fever, but it can spread quickly in crowded areas.
The virus can also be transmitted through coughing or sneezing, and it is most infectious a day or two before the rash appears and in the early days of the rash. In individuals with weak immunity, the dormant virus may reactivate later in life, causing shingles (herpes zoster).
How To Detect Chickenpox Symptoms Early?
Spotting chickenpox early means looking for general warning signs like fever, fatigue, headache, and loss of appetite, which usually appear one to two days before the rash.
The rash itself starts as tiny red spots that later form fluid-filled blisters and eventually scab over. Paying attention to these early symptoms, especially after known exposure, can help identify the infection sooner.
How To Spot A Chickenpox Rash
The first rash usually shows up as small red bumps on the face, chest, or back. These bumps quickly turn into blisters filled with fluid, which are contagious. Over a few days, the blisters break and crust over, forming scabs. It’s common to see spots, blisters, and scabs all at the same time, according to the CDC.
Stages Of Chickenpox
The Mayo Clinic explains that chickenpox progresses in three main stages:
- Incubation Stage (10–21 days): After exposure, the virus remains inactive. Infected individuals typically show no symptoms during this period.
- Prodromal Stage (1–2 days): Early signs include fever, tiredness, headache, loss of appetite, and body aches. This is also when the virus can start spreading to others.
- Rash Stage (5–10 days): Red, itchy spots appear first on the face and chest, spreading across the body. These spots develop into fluid-filled blisters that scab over within a few days. Mild fever, itching, and discomfort are common during this stage.
Breast Cancer To Reach Over 3.5 Mn By 2050, Deaths To Surge 44% Predicts Lancet Study

Credit: Canva
A new study published in The Lancet Oncology journal today revealed that breast cancer continues to be the most common cancer among women worldwide, and predicted that the number of new cases of the deadly disease will reach more than 3.5 million globally in 2050 -- rising by a third from 2.3 million in 2023.
The Global Burden of Disease analysis with data from 204 countries revealed that despite advancements in breast cancer treatments, yearly deaths from the disease will rise by 44 percent -- from around 764,000 to 1.4 million.
While breast cancer disproportionately impacts countries with limited resources, maintaining a healthy lifestyle, including not smoking, getting sufficient physical activity, lowering red meat consumption, and having a healthy weight were found to prevent over a quarter of healthy years lost to illness and premature death.
“Breast cancer continues to take a profound toll on women’s lives and communities,” said lead author Kayleigh Bhangdia from the Institute for Health Metrics and Evaluation (IHME), University of Washington, US.
“While those in high-income countries typically benefit from screening and more timely diagnosis and comprehensive treatment strategies, the mounting burden of breast cancer is shifting to low- and lower middle-income countries where individuals often face later-stage diagnosis, more limited access to quality care, and higher death rates that are threatening to eclipse progress in women’s health,” Bhangdia added.
Inequalities In Breast Cancer Burden
The study revealed that the rates of new cases remain highest in high-income countries (HICs), but are growing fastest in low-income countries (LICs).
Women in low- and lower-middle-income countries accounted for 27 percent (around 628,000) of new cases globally, exposing likely disparities in timely diagnosis and shortages of quality treatment, including radiotherapy machines, chemotherapy drugs, and pathology labs, and standard treatments.
In 2023, an estimated 2.3 million new breast cancers were diagnosed worldwide in women (with 73 percent or 1.67 million cases occurring in high- and upper-middle-income countries). Of these, 764,000 ended in deaths (with 39 percent or 300,000 deaths occurring in low- and lower-middle-income countries).
Further, the number of years of healthy life lost due to poor health and early death more than doubled from 11.7 million years in 1990 to 24 million years in 2023.
Women in low- and lower-middle-income countries also contribute to more than 45 percent of all the ill-health and early deaths from breast cancer globally (nearly 11 million years of healthy life lost).
Three-fold Rise In Pre-menopausal Breast Cancer
The study reported a three-fold rise in pre-menopausal breast cancer in women aged 55 or older in 2023 -- compared to women aged 20-54 years.
However, rates of new cases have risen in women aged 20-54 years (up 29 percent) since 1990, with rates in older women remaining relatively unchanged.
Major Lifestyle Risk Factors
In 2023, 28 percent of the global breast cancer burden (6.8 million years of healthy life lost to disability, illness, and early death) was linked to six potentially modifiable risk factors. These include:
- High red meat consumption -- linked to nearly 11 percent of all healthy life lost
- tobacco use (including second-hand smoke; 8 percent),
- high blood sugar (6 percent),
- high body mass index (4 percent),
- high alcohol use and low physical activity (both 2 percent)
Substantial progress has been made in reducing the global breast cancer burden linked to high alcohol use and tobacco between 1990 and 2023, which declined by 47 percent and 28 percent, respectively.
© 2024 Bennett, Coleman & Company Limited

