- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
25-Year-Old Fitness Trainer Got Diagnosed With A Rare Type Of Blood Cancer After Ignoring Subtle Signs
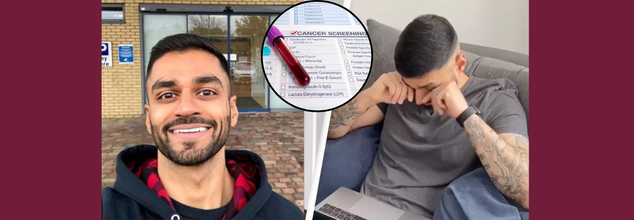
People who work out daily and maintain a healthy diet are deemed invincible and the epitome of discipline, strength, and self-consciousness but for Dilan Patel, a 25-year-old U.K.-based fitness coach, started waking up in the middle of the night sweating profusely night after night, he attributed it to an overheated room or the result of high-intensity workouts. For almost two years, he ignored the warning signs until his body could no longer be ignored. What was initially a nagging irritation was diagnosed as Stage 4B Hodgkin lymphoma, an uncommon blood cancer.
Patel was 23 and like most young adults, establishing his career, pumping iron at the gym, and planning his future. Life was structured and good. But an odd trend persisted that he could not dispel.
"I'd wake up two or three times during the night, totally soaked. My clothes, my bed sheets—everything was wet," he said in a viral Instagram reel for its brutal honesty. "I thought I was just overheating from sleeping under too many blankets. I didn't think anything of it."
But it wasn't just night sweats. He had constant itchiness, which he ignored as dry skin, and visible lumps on his neck, which he explained away as muscle growth from weightlifting. "Everything had an explanation—or so I thought," he remembered.
Gradually, the symptoms worsened. The fatigue became unstoppable, and the night sweats intolerable. Patel consulted medical advice only then. What ensued was a diagnosis that would make his world spin around: Hodgkin lymphoma, an uncommon form of cancer that impacts the lymphatic system.
By the time it was detected, the disease had advanced to Stage 4B. Imaging revealed five tumors—one of which had already spread to his lung. The news was devastating.
“I couldn’t believe it,” he said. “I’d spent two years brushing off the warning signs. My body had been screaming at me.”
What is Hodgkin Lymphoma?
Hodgkin lymphoma is a type of blood cancer that starts in the lymphocytes, a form of white blood cell essential to the immune system of the body. It most commonly occurs in the lymph nodes but, as happened in Patel's situation, if not diagnosed promptly, can infect the lungs, liver, or bone marrow.
While uncommon—only around 2,200 new cases are diagnosed annually in the U.K., and less than 0.5% of all cancers—it's one of the more curable cancers if caught in time. Cancer Research UK says that approximately 75% of patients who are diagnosed with Hodgkin lymphoma are still alive ten years later.
In spite of its treatability, the disease is virulent and has the potential to severely compromise quality of life. Survivors have a higher risk of secondary cancers, cardiovascular disease, and respiratory complications from treatment.
Symptoms and Signs of Hodgkin Lymphoma
One of the biggest problems with Hodgkin lymphoma is that its symptomatology is misleading. The disease may have vague signs that resemble less severe illnesses:
- Unexplained fever
- Drenching night sweats
- Persistent fatigue
- Painless inflamed lymph nodes in the groin, underarms, or neck
- Unexplained weight loss
- Intense itching, particularly after a bath
In Patel's situation, all these symptoms existed, but every one of them had an "everyday" cause that delayed his diagnosis. This is common, particularly for young adults, who usually equate these signs with stress, exercise, or changing seasons.
Although the exact cause of Hodgkin lymphoma is still unclear, Epstein-Barr virus (EBV), the same virus that causes mononucleosis, is believed to play a role in the development of approximately two out of five cases. Genetics, a weakened immune system, and environmental exposures are also being researched as possible risks.
Interestingly, although there has been an increase of 38% in rates since the 1990s, adults aged over 70 have registered the steepest rise. But there's also been an increase of 21% amongst younger adults, especially those in the 20-40 group to which Patel belongs.
Why Fitness Enthusiasts Shouldn't Ignore "Minor" Symptoms?
Fitness professionals are usually the epitome of health. But that self-image can postpone diagnosis, as it did for Patel. Lumps are attributed to muscle gain. Fatigue is considered a normal effect of intense training. Itching and night sweats are attributed to diet or dehydration.
This is a cautionary tale, particularly for young adults who may think that they're too healthy to get sick. Hodgkin lymphoma doesn't care about lifestyle or dietary habits. Even people who look the healthiest can be quietly fighting a serious disease.
Hodgkin lymphoma is routinely treated with chemotherapy, and in certain instances, radiation. As good as the prognosis is, however, early detection remains the best weapon against the disease and reducing long-term side effects.
Even with his advanced diagnosis, however, Patel's tale is also one of determination and vigilance. He's sharing his message from his platform- Don't ignore what your body is trying to tell you.
“If there's one thing I’ve learned from this experience,” he said, “it’s to pay attention to your body. Those little signs? They’re there for a reason. Don’t wait until it’s too late.”
Sudden Cardiac Arrests Could Be Linked To Bodybuilding: Study

(Credit-Canva)
One of the most grueling and difficult fitness regime people go through is bodybuilding. The regime was made to enhance the muscles of the human body. As a sport, it is bodybuilders who train their muscles to artistically display the pronounced muscle mass, symmetry as well as overall aesthetics. Building muscles mass includes doing exercises like strength training, resistance training devices as well as cardio. These exercises help bodybuilders keep their body fat at the lowest possible.
Being the epitome of health, many people believe that body builders live healthy and long lives. However, a new study shed light on the concerning link between bodybuilding and sudden deaths.
Major Health Risks Related To Bodybuilding
Bodybuilders may spend endless hours building impressive muscles, but a new study shows their hard work might harm their hearts. Research in the European Heart Journal found that many male bodybuilders die suddenly from heart issues. What's more, professional bodybuilders are five times more likely to have a sudden heart attack than amateurs.
Researchers highlighted that the risk of death for male bodybuilders is notably high. They noted that competing at a professional level seems to increase this risk, with pros having many more sudden heart deaths. This study started because of more and more reports of early deaths and heart attacks in the bodybuilding world.
The study also found that about 15% of bodybuilder deaths were classified as "sudden traumatic deaths," which include car accidents, suicides, murders, and overdoses. Experts stressed that these findings show we need to think about the mental impact of bodybuilding culture, noting that mental health issues can sometimes get worse with drug abuse, leading to risky or self-harming behaviors.
Study Methodology and Findings
Researchers looked at information from 20,300 athletes who competed in International Federation of Bodybuilding and Fitness (IFBB) events between 2005 and 2020. The IFBB is the main group for bodybuilding contests worldwide. The study followed these athletes' health until July 2023, for over eight years on average. During this time, 121 bodybuilders passed away.
A shocking 38% of these deaths were due to sudden cardiac death, meaning their hearts just stopped. Sadly, 11 of these cases happened to active competitors who were, on average, just under 35 years old. Experts pointed out that sudden heart death can happen even to young, seemingly healthy people without known heart problems, though it's rare.
What Increases The Risk?
Experts pointed to several practices common in bodybuilding that can strain the cardiovascular system:
Extreme strength training: Intense physical exertion can put immense pressure on the heart.
Rapid weight loss strategies: Severe dietary restrictions and dehydration can disrupt the body's delicate balance.
Widespread use of performance-enhancing substances: These can have detrimental effects on heart health.
How Does It Affect Your Heart?
These things can cause irregular heartbeats and changes to the heart's structure over time. Autopsies of five bodybuilders in the study showed that four had enlarged hearts and thicker heart muscles, which make heart failure more likely.
Professionals face a higher risk because they often push these practices harder for longer periods and feel more pressure to get extreme physiques. Experts warned bodybuilders, that aiming for physical perfection is great, but trying for extreme body changes at any cost can be very risky their health and heart.
Your Chronic Health Struggles Could Be Doubling Your Risk Of Depression- Here’s What To Know

Credits: Canva
Living with a chronic illness can be like fighting an uphill battle—physically, mentally, and emotionally. But new research indicates the cost may be even deeper than most people know: long-term physical illness may dramatically raise your risk of developing depression.
As a revolutionary study in Nature Communications Medicine explains, individuals with many chronic conditions are much more likely to experience a mental health breakdown. This finding explains the essential, but frequently overlooked, connection between body and mind.
Traditionally, healthcare systems everywhere have addressed physical and mental illness as separate silos. But new science is presenting a different picture—one where body and mind are highly intertwined.
In the recent U.K. Biobank study, researchers followed over 142,000 adults aged between 37 and 73, all of whom had at least one chronic illness but no prior diagnosis of depression. The findings were eye-opening: individuals with multiple physical conditions were up to 2.4 times more likely to be diagnosed with depression over the next decade compared to those without chronic illnesses.
The report's co-author, Professor Bruce Guthrie from the University of Edinburgh, underscored the significance: "Healthcare tends to think of physical and mental ill health as two totally separate things, but this research indicates that we must do better at predicting and treating depression in individuals who have physical illness."
Which Conditions Have the Highest Risk?
While any long-term illness will erode mental toughness, some combinations greatly increase depression risk. Among the study's most surprising findings:
Individuals with migraine illness or chronic respiratory disease had twice the risk of depression.
A combination of heart disease and diabetes raised depression risk by almost 78%.
Gastrointestinal illnesses such as IBS, celiac disease, and liver disease were associated with an 83% increased risk of depression in women and a twofold increase in risk in men.
These figures are more than just statistics—they represent real individuals facing a double burden of illness and emotional distress. And with 1 in 12 people in high-risk groups developing depression over a decade (compared to 1 in 25 among those without chronic conditions), the data calls for urgent attention.
Why Is Depression Always More Than Just Feeling Sad?
In order to comprehend why this is important, it's necessary to know what depression actually is. Clinical depression, also known as major depressive disorder, is a mood disorder that extends far beyond fleeting sadness. It's a complex illness that influences the way individuals think, feel, and behave. Symptoms can involve:
- Constantly feeling sad or hopeless
- Loss of interest in activities once enjoyed
- Fatigue or loss of energy
- Trouble concentrating or making decisions
- Changes in appetite or sleep habits
- Physical symptoms like sudden pain
- Integers of suicide or harming oneself
Depression is not a personal failing or something you can simply "snap out of." It is a genuine medical illness that more often than not needs to be treated by professionals—such as therapy, medication, or both.
Biological and Emotional Roots of Depression in Chronic Illness
Why chronic illness would so greatly increase the risk of depression? Experts consider the causes to be multifactorial.
Physiologically, certain chronic diseases interfere with brain chemistry or hormonal equilibrium, both of which play a critical role in regulating mood. Such conditions as thyroid disease or diabetes, for example, can have a direct effect on neurotransmitters associated with depression.
Emotionally, the ongoing juggling act of pain, tiredness, and doctor visits can be draining. Throw in social isolation, financial burden, or loss of autonomy, and it is not hard to understand how emotional well-being can start to fray.
When to Seek Help?
If you or someone close to you is living with a chronic illness, it is important to remain aware of depression symptoms. Early treatment makes a real difference in the outcome of care and the quality of life.
Do not wait until things get worse. If you see signs such as lingering unhappiness, loss of initiative, or constant exhaustion, seek professional attention. A visit to a primary care doctor or mental health expert can be an important first step.
This new research supports what many patients have long intuited—real wellness can't be realized without attending to body and mind. It's high time for medical providers, policymakers, and insurers to adopt a more integrated strategy for the management of chronic disease that encompasses preventive screening and treatment for mental illness.
Lead researcher Lauren DeLong said it best: "We noticed obvious links between physical health conditions and the occurrence of depression, but this research is just the start. We hope our research will encourage other scientists to explore and disentangle the connections between physical and mental health conditions."
Is It Safe When You Skip Your Period While On Birth Control?

Credits: Canva
Periods can be a mild inconvenience for some and for others, they're a cause of disabling pain, mood swings, or health complications. As medical science continues to advance, one question keeps raising eyebrows and eyebrows: Is it actually safe to miss your period on the pill? The short answer? Yes, and in many cases, it can even be beneficial but before tossing aside your placebo pills, it’s important to understand what’s happening to your body, the science behind menstrual suppression, and the myths versus facts surrounding it.
For many people, the motivation to skip a period is rooted in convenience. Maybe you’re planning a beach vacation, attending a wedding, or simply want to avoid the monthly disruption that comes with cramps and mood swings.
Beyond lifestyle, others find relief from more severe health conditions. Painful cramps, mood swings, endometriosis, anemia, and even fibroids are all legitimate reasons for wanting to control or prevent menstruation.
People with chronic pelvic pain, hormonal issues, or neurological conditions like menstrual migraines can also benefit from less frequent menstruation.
What Happens When You Skip a Period on Birth Control?
The menstrual cycle induced while on the pill is not actually a period it's a withdrawal bleed from the placebo (hormone-free) week. If you avoid that week and stick with active pills or use other continuous birth control like the ring or implant without interruption, you stop that withdrawal bleed.
"There is no medical need for the body to bleed each month with the use of hormonal birth control. It's a pattern created decades ago to imitate the natural cycle not because the body requires it.
By keeping the hormones at a steady level through continuous use, users can actually abolish regular bleeding altogether.
Even with the evidence for menstrual suppression, falsehoods prevail in cyberspace. Social media influencers such as those on TikTok advise against "suppressing natural processes" or assert that long-term hormonal birth control causes infertility.
Medical practitioners warn against such a tide of online misinformation. There is no scientific evidence that avoiding periods through birth control negatively impacts fertility. These stories usually come without context, are not peer-reviewed, and give rise to unnecessary fear.
Depending on anecdotal guidance rather than medical experience can be hazardous particularly when it impacts reproductive choices.
What Are The Risks Involved?
Though missing your period with birth control is safe medically for most, it's not completely side effect-free. One typical problem is breakthrough spotting or bleeding, particularly if you miss several cycles consecutively.
It's also worth mentioning that since menstruation is a visual indicator of pregnancy detection, becoming period-free could make it more difficult to detect an unplanned pregnancy early on. That is why correct and consistent use of your contraceptive is paramount.
In exceptional circumstances, long-term use of hormonal birth control can marginally boost the risk of blood clots or cardiovascular problems, particularly in smokers or those with existing conditions but missing your period doesn't add to those risks above the baseline created by the birth control itself.
If you're thinking about missing your period consistently, talk to a health care provider. You'll figure out the best option together — whether that is extended-cycle pills, hormonal IUDs, rings, patches, or implants.
Your health care provider will also assess if you're a good fit based on your history, lifestyle, and general wellness objectives. Most importantly, they'll walk you through what to anticipate and how to watch for any unusual symptoms.
Skipping your period using hormonal birth control is not only safe, it can be incredibly beneficial for many people. Whether you’re looking to gain more control over your schedule, reduce painful symptoms, or manage a chronic health issue, menstrual suppression is a validated, doctor-approved choice.
Nevertheless, it is a personal choice that can be made with a doctor's counsel. With proper information and assistance, you can gain control over your cycle according to your lifestyle and health.
© 2024 Bennett, Coleman & Company Limited

