- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
9 Signs Your Skin Changes Could Be Psoriasis, According to Experts

You spot an itchy patch, a flaky scalp, or a rash after a bad week and think, “It’s probably nothing. Maybe I just need a better moisturiser.” But sometimes, skin changes are like quiet signs from your immune system, and ignoring them could mean missing a chronic condition hiding in plain sight: psoriasis.
Psoriasis is a chronic autoimmune disease whose symptoms are often mistaken for everyday skin issues. For light skin tones, it can show up red or pink with a silvery white scale; on darker skin tones, it might look purplish, grey, or dark brown, with scaling that’s less obvious.
Dr K R Sharmatha, Senior Consultant, Dermatology, SIMS Hospital, Chennai, says that because psoriasis often hides behind myths, it’s misdiagnosed as something else. So, let’s debunk nine common misconceptions that are actually signs you might have psoriasis, not just a skin infection.
1. It’s dry skin; a moisturiser will fix it
Early psoriasis can look like stubborn red or scaly patches on knees, back, scalp, or elbows, resulting in silvery-white scales on inflamed skin. Moisturisers won’t cut it; targeted treatments and light therapy are the real solutions.
2. If it itches, it’s probably eczema
Psoriasis can itch like eczema, but it’s not just a surface problem. The itching can cause burning and pain, with flare-ups that feel deep and relentless.
3. Flaky scalp = dandruff
Scalp psoriasis is thicker, with defined plaques and red blotches. Medicated shampoos containing coal tar or salicylic acid can help, but it needs proper diagnosis first.
4. Temporary allergy rash after illness or stress
After a sore throat, fever, or a rough life event, small teardrop-shaped red lesions might appear. This is often misread as an allergy rash, but it could be guttate psoriasis, triggered by immune stressors and treatable with immune-regulating medication and UV therapy.
5. Nail crumbling means vitamin deficiency
Yellow nails, tiny dents, or separation from the nail bed could mean nail psoriasis. It can even signal psoriatic arthritis, an inflammatory joint condition.
6. Shiny red patches are sweat rash or fungal infections
Inverse psoriasis shows up as red, shiny patches without scaling, often in the groin, underarms, or under breasts. Its appearance fools people into thinking it’s a sweat rash or fungal infection. Gentle cleansers and prescription creams can help.
7. Skin issues and joint pain aren’t connected
Think again. Persistent stiffness or pain in fingers and knees can be psoriatic arthritis, which may show up without visible skin patches.
8. If it’s not visible, it’s not serious
Psoriasis can affect hidden spots like the inner thighs or inside the mouth, severely impacting quality of life and requiring customised treatment.
9. If it runs in the family, you’re stuck with it
Genetics can play a role, but early intervention reduces severity and prevents complications.
Dr Vaaruni Ravishankar, Consultant Dermatologist, MGM Healthcare, Chennai, explains that psoriasis can be silent, sometimes showing up as fissured palms and soles, oozing skin, persistent groin or armpit rashes, or rough, pitted nails. It can even come disguised as arthritis or link up with autoimmune gut issues.
However, don’t panic, self-treat, or ignore it. Psoriasis is an autoimmune condition triggered by factors like hormonal changes, metabolic issues, genetics, stress, certain medications, infections, and lifestyle factors such as smoking or alcohol. But it’s not contagious.
Diagnosis often involves a clinical exam and, if needed, a skin biopsy to confirm. Dr Ravishankar recommends lifestyle adjustments, stress management, and targeted treatment, from topical formulations to immune-modulating medications or biologics that tackle inflammation. Daily care with pH-balanced cleansers, barrier-repair emollients, and sun protection can keep symptoms under control.
And if skin problems last more than two to four weeks, don’t keep guessing. Persistent discomfort, lack of improvement with fungal creams, or worsening skin could be subtle signs of psoriasis. Myths only delay care and in the case of psoriasis, early attention can change everything.
Where You Get Your Rabies Shot Matters: Doctor Explains Why Rabies Vaccines Should Not Be Given In Buttocks
Credits: Canva and screengrab from Instagram
Dr Srivanjani Santosh, Pediatrician, Social Activist and First Aid trainer, who had earlier spearheaded the ORS campaigned for eight years, urging FSSAI to ban the misuse of the term 'ORS' on non-WHO=standard sugar drinks, has once again shared an important health video on rabies vaccination. Dr Santosh shared that if any mammal, including dog, cat, horse, cow, buffalo, monkey or bat scratch or bit a person, they must be vaccinated with rabies shot.
She also pointed out something many miss: the location of administering the rabies shot. In her video she urged people to not get the shot administered in buttocks, and to only get it on their shoulders or thighs. She also claimed that many clinics and hospitals, despite knowing this fact, are administering rabies vaccination on buttocks.
Also Read: Hangover Star Ken Jeong's Wife Beats Stage 3 Breast Cancer
Why Does Location Of Administration Matter In Rabies Shot?
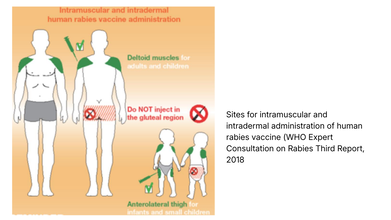
The World Health Organization (WHO) strongly recommends that rabies vaccines must be injected into the deltoid region, which is the upper arm or near the shoulder region in adults.
In small children, the WHO notes that deltoid region, as well as anterolateral area of the thigh muscle, which is also the upper thigh works.
WHO notes that like any other injections, rabies vaccine should not be given in the gluteal region, that is the buttocks, because of low absorption due to the presence of adipose or the fat tissue.
This video comes at the time when a case of a Birmingham woman losing all her limbs to dog's lick has made headlines all over the news. Health and Me also reported on the same.
Read: Woman Loses All Her Limbs After Getting Sepsis From Dog Lick
Health and Me spoke to Dr. Rakesh Pandit, Senior Consultant & HOD, Internal Medicine at Aakash Healthcare, who further explained, that as per guidelines by the WHO, the rabies vaccine should not be given in the buttocks as they have a heavy layer of fat. The body might not properly absorb the vaccine if it is injected into this fat instead of the muscle, which could result in a vaccine failure.
"A vaccine failure in case of rabies is like a death sentence because the disease is one hundred percent lethal once it shows the signs. The injection site for the vaccine depends on the patient's age; older children and adults must receive the vaccine in the upper arm or shoulder, while infants and toddlers must receive it in the thigh. The vaccine must also be administered with the right needle length to reach the required depth," he said.
Dr Pandit further elaborated, "The place of administering the vaccine (arm or thigh, subcutaneous or intramuscular) has an effect on the immune response, speed at which the vaccine is absorbed, pain and the risk of side effects." He said, "Some vaccines give best results when given in muscle for better immunity. Other vaccines may need subcutaneous administration. When given at the correct site, the vaccines ensure maximum effect, safety and reduced local reactions like swelling."
Read: 36% Of Rabies Death Comes From India: This Is What You Should Do After A Dog Bite, Explains Doctor
What Should One Keep In Mind While Getting A Rabies Shot?
Dr Mule points out that even when there are minor scratches, without bleeding, you must get a rabies shot. "Rabies can be contracted through broken skin. Such exposures still require medical evaluation and, in most cases, rabies vaccination."
What Should One Do Immediately After Being Bitten Or Scratched?
- Wash the wound immediately for at least 15 minutes with soap and running water
- Apply an antiseptic such as povidone-iodine
- Do not apply home remedies like turmeric, chili or oil
- Seek medical care promptly for rabies vaccination and possible immunoglobin
Dr Mule points out that the rabies vaccine should be started as soon as possible. "Ideally within 24 hours of a bite or scratch. However, even if there is a delay of days or weeks, vaccination should still be started immediately as rabies has a variable incubation period," he says.
The temperature of the vaccine matters. "Rabies vaccines are temperature-sensitive and must be stored between 2°C and 8°C. Exposure to heat or freezing can reduce vaccine potency. Poor cold-chain maintenance is a known reason for vaccine failure in rare cases," points out the doctor.
Dr Mule points out that the vaccine should be given intramuscularly in the deltoid or upper arms for adults, as gluteal or buttock injections could lead to inadequate absorption and reduce effectiveness.
Study Links Throat Infection To Sudden Skin Inflammation, Psoriasis
Credit: Canva
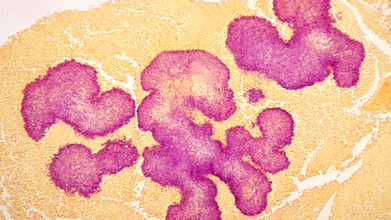
A simple strep throat infection, can trigger sudden skin inflammation, leading to psoriasis, particularly in children and young adults, according to a study.
Researchers from the Karolinska Institutet in Sweden showed that a strep throat infection caused by the Group A Streptococcus (GAS) bacterium, can trigger guttate psoriasis by altering the behavior of key immune cells. Guttate psoriasis is an often sudden-onset form of psoriasis with small, red, "drop-shaped" scaling spots on arms and legs.
While neutrophils -- the most common type of immune cell -- are the first immune cells to respond to GAS infection, the study showed that during a streptococcal infection, the immune cells behavior changes depending on their environment.
Notably, among people with guttate psoriasis, the neutrophils presented with antigens -- fragments of pathogens that signal and guide other immune cells -- get accumulated. Once accumulated, the immune cells activated the T cells, leading to inflammation, explained the researchers in the paper, published in the journal eBioMedicine.
"Doctors have long known that strep throat can precede guttate psoriasis, but the biological explanation has been unclear," said Avinash Padhi, first author of the study and Research Specialist at the Division of Dermatology and Venereology, at Karolinska.
"Our findings suggest a link between infection and skin inflammation through the accumulation of antigen-presenting neutrophils in patients' skin," Padhi added.
How Cells Shape Immune Response
The team analyzed receptor–ligand interactions -- the molecular signals cells use to coordinate immune responses to examine how neutrophils interact with other cells.Magdalini Lourda, senior author of the study and senior research specialist at the Department of Laboratory Medicine, noted that the "results challenge the traditional view of neutrophils as simple first-line defenders".
The findings show that the neutrophils play "a wider role in shaping immune responses, which may be important when designing future treatments."
How Was The Study conducted?
Using single-cell technologies, the team analyzed blood and skin samples of patients with guttate psoriasis. This enabled the researchers to examine thousands of individual immune cells in detail.To find how neutrophils work in psoriasis, the blood neutrophils from psoriasis patients were compared with those from healthy individuals. Blood neutrophils from patients with severe strep-related lung inflammation were also compared.
What Is Guttate Psoriasis?
Guttate psoriasis is a distinct form of acute-onset psoriasis. It is an inflammatory skin disease characterized by the sudden appearance of red, scaly, and smaller skin lesions widespread over the body.
The condition typically follows an infection, most commonly tonsillitis caused by Group A Streptococcus (GAS). Adolescents and young adults are the most affected. It accounts for about 2 per cent of all cases of psoriasis.
Genetics, environmental triggers, such as an upper respiratory tract infection, and the onset of an inflammatory condition in a distant organ are the major risk factors.
The condition may be diagnosed by skin biopsy, throat swab culture, and blood tests.
Hangover Star Ken Jeong's Wife Beats Stage 3 Breast Cancer

Credits: Instagram
Hangover star Ken Jeong's wife Tran Ho Jeong in 2007 discovered a hard lump in her breast while she was breastfeeding their newborn twins Alexa and Zooey. She was diagnosed with stage 3 triple negative breast cancer (TNBC) in 2008.
What Is Stage 3 Triple Negative Breast Cancer?
As per the American Cancer Society, it is an advanced aggressive, and fast-growing cancer that has spread to nearby lymph nodes or tissue, however, does not distant organs. It is characterized by the absence of estrogen, progesterone and HER2 receptors, which requires a combined approach of chemotherapy, surgery, and sometimes also radiations As per the American Cancer Society, TNBC accounts for about 10 to 15 per cent of all breast cancers.
At stage 3, TNBC has grown extensively and invaded nearby tissues and is likely to spread to lymph nodes. However, it has not metastasized to distant organs.
Also Read: Zimbabwe Among the First African Countries to Roll Out Breakthrough HIV Injections
Hangover Star Ken Jeong's Wife Cancer Journey
As doctors said, for Tran, it was a "year of hell". She underwent 16 rounds of chemotherapy when Ken was filming The Hangover. This was then followed by a mastectomy and radiation therapy.
"I am going to survive this. I am going to fight. I have to live for the girls and for Ken," she said. After two years of battle, Tran was finally declared cancer free in 2010. Ken called it "the greatest moment" of his life.
What Happens In Breast Cancer?
As per the World Health Organization (WHO), breast cancer is the most common cancer globally with around 2.3 million new cases every year. At the rate of 1 in every 8 person in both sexes and a quarter of all cancer in women with 70% mortality occurs due to constrained resources.
It is a disease where abnormal breast cells grow out of control and form tumors. If it is left unchecked, the tumors can spread throughout the body and become fatal.
It originates in the milk ducts or the milk-producing lobules of the breast. The earliest form is not life-threatening and can be detected in the early stages. Cancer cells can spread into nearby breast tissue and create tumors that cause lumps or thickening. These invasive cancers can spread to nearby lymph nodes or other organs and metastasis can be life-threatening and fatal.
Signs And Symptoms Of Breast Cancer
The common signs are:
- A breast lump or thickening, often without pain
- Change in size, shape or appearance of breasts
- Dimpling, redness, pitting or other changes in the skin
- Change in nipple appearance or the skin surrounding the nipple (areola)
- Abnormal or bloody fluid from the nipple
Treatment
The treatment depends on the stages and subtypes of the cancer. However, common treatments involve:
- Surgery to remove breast tumor
- Radiation therapy to reduce recurrence of breast cancer around the breast tissues
- Medicals to kill cancer cells and prevent spread
- Therapies like hormonal and chemotherapy or targeted biological therapy
© 2024 Bennett, Coleman & Company Limited

