- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Explained: Your Seasonal Flu Shot Just Got Upgraded To A Nasal Spray Vaccine That Comes to Your Door

Credits: iStock
Flu season has meant rolling up your sleeve for a shot at the doctor’s office or pharmacy. Now, that’s changing. AstraZeneca has launched FluMist Home, the first FDA-approved flu vaccine that can be delivered to your doorstep and self-administered—no needles required.
This new option, a nasal spray version of the vaccine, builds on FluMist’s two-decade track record. First approved by the Food and Drug Administration (FDA) in 2003, FluMist has long been available at clinics and pharmacies. But in September 2024, the FDA gave the green light for at-home self-administration. Less than a year later, the program is rolling out across 34 states in time for the 2025–2026 flu season.
The stakes couldn’t be higher, last flu season was one of the most severe in recent memory. The CDC estimates up to 82 million illnesses, 1.3 million hospitalizations, and 130,000 deaths from flu between October 2024 and May 2025. Yet vaccination rates remained low, with fewer than half of Americans getting their annual shot.
Experts say that convenience is a major barrier. Between busy schedules, limited access to clinics, and vaccine hesitancy, too many people skip protection. FluMist Home could remove at least one of those hurdles by making the process as simple as ordering online.
“People are increasingly comfortable with managing their health at home—whether through Covid-19 tests or self-injections for chronic conditions,” explains AstraZeneca. “This option takes advantage of that shift and expands access to flu vaccination.”
Do's and Don'ts Of Using Flu Nasal Spray
FluMist Home is FDA-approved for people ages 2 through 49. Adults can use it themselves, while children as young as 2 can receive it with help from a parent or caregiver.
However, it’s not for everyone. Because FluMist is a live, weakened-virus vaccine, pregnant women and people with weakened immune systems should consult their doctors before considering it. Those outside the approved age range must still rely on traditional flu shots.
How FluMist Works?
The ordering process mirrors a telehealth experience. Patients complete a brief medical questionnaire online, which is reviewed by a licensed healthcare provider before the prescription is approved. Insurance covers the cost for most users, with a flat $8.99 shipping and handling fee.
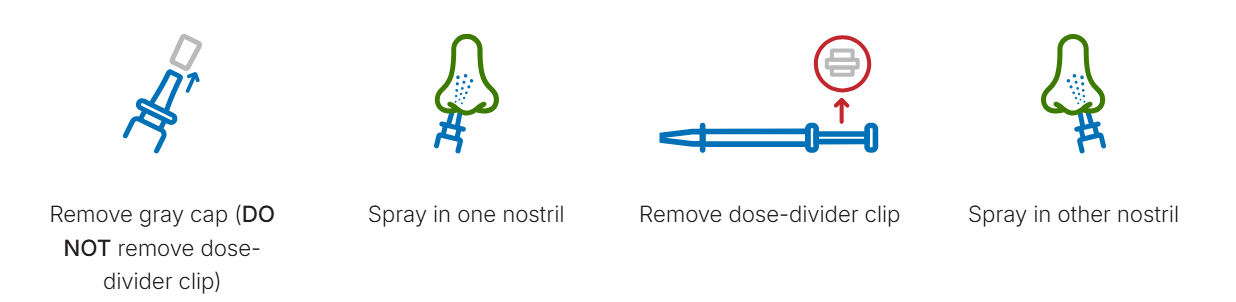
When FluMist arrives, it’s shipped in insulated, temperature-controlled packaging with ice packs to preserve stability. Each vial contains two pre-measured doses one for each nostril—separated by a clip. To administer, simply breathe normally while spraying; there’s no need to inhale deeply. A slight tickle, sneeze, or drip afterward is normal.
Patients can download a vaccination record from the online portal, and—if permission is given—the record is automatically shared with their doctor and uploaded to state vaccine registries.
Effectiveness and Safety
AstraZeneca emphasizes that FluMist Home uses the same formulation and vial as the version given in clinics. Its efficacy is on par with injectable flu vaccines, but the delivery method is needle-free.
The most common side effects are mild: runny nose, nasal congestion, and sore throat in adults. Children may experience low-grade fever. These symptoms generally resolve quickly.
Importantly, the FDA required AstraZeneca to conduct a usability study before approval. Results showed that 100% of participants were able to correctly self-administer the full dose without healthcare supervision.
How This Helps Tackle The Vaccination Gaps?
Needle-free, self-administered vaccines aren’t just about convenience—they may be critical in improving uptake. FluMist Home joins a growing trend of decentralizing preventive healthcare, putting tools directly into patients’ hands.
Historically, nasal spray flu vaccines were popular among children and adults who disliked shots. Now, offering a home option could further broaden access. As public health experts warn about the dangers of simultaneous flu, RSV, and Covid-19 waves, innovations like FluMist Home might play a pivotal role in reducing strain on hospitals.
The CDC notes that every additional percentage point increase in vaccination coverage can save thousands of lives during peak flu seasons. By lowering logistical barriers, FluMist Home could help close that gap.
Nasal Spray vs Shot: What Works Better?
The differences between FluMist and injectable vaccines come down to technology. Traditional flu shots use either killed viruses or specific proteins to teach the immune system how to respond. FluMist, by contrast, uses a live but weakened influenza virus. Both methods are proven to work, but some patients respond better to one than the other.
For people who avoid shots due to fear or discomfort, FluMist offers a gentler alternative. For children, especially, a quick nasal spray can mean less stress and higher compliance.
Could Nasal Sprays Be the Future of Vaccination?
The rollout of FluMist Home may be a harbinger of bigger changes. The pandemic normalized home-based care and accelerated acceptance of mail-order biologics, self-testing kits, and virtual consultations. Vaccines, once the exclusive domain of clinics, could follow suit.
Some researchers are already working on shelf-stable, oral, or patch-based vaccines that could one day make prevention even more accessible. For now, FluMist Home represents a significant step forward in modernizing how people protect themselves during flu season.
Useful Tips for Patients
Storage: Keep FluMist refrigerated (35°F to 46°F) until use.
Timing: Administer early in flu season for maximum protection.
Recordkeeping: Save your vaccination confirmation for medical records and travel purposes.
Disposal: Packaging materials are largely recyclable; chill packs can be reused.
FluMist Home gives people a practical, needle-free, at-home option to stay protected against the flu. While it’s not suitable for everyone, its convenience could boost vaccination rates at a time when respiratory viruses remain a major public health threat.
Early Vs Late Autism: Study Finds Autism Diagnosed At An Early Age Is Different Than One Diagnosed Later In Life

(Credit-Canva)
A large international study from the University of Cambridge suggests that autism diagnosed early in life is fundamentally different from autism diagnosed later on. The findings, published in Nature, analyzed data from more than 45,000 autistic individuals and showed that the timing of diagnosis often reflects distinct biology and development.
The research team suggests this means that the term "autism" likely describes multiple conditions, not just one.
There are many misconceptions about autism in the media, many believe it can be caused by bad parenting, that it can only affect boys as well as that it can be cured. While these may not be true, can it change overtime or develop into something else?
What is Autism?
According to Mayo Clinic Autism Spectrum Disorder (ASD) is a condition that affects how the brain develops. It changes how people understand and interact with the world around them. This causes challenges in two main areas:
- Social Life and Communication: People with ASD often find it hard to talk with others and socialize.
- Behaviors: The condition also involves having interests or behaviors that are very specific and often repeated.
The word "spectrum" is key because it means ASD affects people in many different ways. Some people have mild symptoms, while others have more severe challenges.
Over time, it can make it hard for a person to manage in social situations, school, or at work. Many children show signs of autism within their first year of life. A few children seem to develop normally at first, but then lose some skills and start showing autism symptoms between 18 and 24 months old.
Early Diagnosis vs. Later Diagnosis: What's the Difference?
The study found two distinct groups based on when a person received their autism diagnosis:
Early Diagnosis (Typically Before Age Six)
These children were more likely to show social and behavioral difficulties from a very young age. Their traits are often easier to spot by parents and doctors, leading to a quicker diagnosis. Their underlying genetic profile is distinct and shares less in common with other mental health conditions.
Later Diagnosis (Late Childhood or Adolescence and Beyond)
These individuals often saw their social and behavioral challenges emerge or become noticeable during adolescence. They have a higher risk of developing mental health conditions like depression and Post-Traumatic Stress Disorder (PTSD). Their average genetic profile is surprisingly closer to that of ADHD and depression than it is to the genetic profile of early-diagnosed autism.
What Role Do Genetics Play In Autism?
The findings show that the difference in diagnosis timing is due to more than just how quickly families access care; it's also linked to genetics.
Genetic Overlap
The study found a strong genetic connection between later-diagnosed autism and psychiatric disorders. This suggests that certain genetic factors might make these individuals naturally more prone to mental health issues.
Lack of Early Support
Researchers also stress that not getting support in early childhood likely plays a role. Going undiagnosed makes people more vulnerable to difficulties like bullying, which significantly increases the risk of mental health struggles later on.
The authors hope these findings will change how autism is understood, studied, and supported, allowing for better help for autistic people of all ages.
Think You Don’t Need A Flu Shot? Here’s Who Needs It And Why

Credits: Canva
Flu Shot: With flu season fast approaching, many people wonder when the best time is to get vaccinated. According to the U.S. Centers for Disease Control and Prevention (CDC), for most people who only need one dose, September and October are the ideal months to get the flu shot. The agency recommends that everyone be vaccinated by the end of October. Still, a percentage of the population believes flu shots aren’t essential and can be skipped.
Who Should Get a Flu Shot Every Year?
The CDC and major medical organizations advise everyone aged six months and older to get a yearly flu vaccination. Despite misinformation circulating online, these recommendations have not changed.
Certain groups are at higher risk of severe illness, people over 65, pregnant women, young children, and those with chronic health conditions like asthma, diabetes, heart disease, or weakened immune systems. While about 71% of seniors get their flu shot each year, less than half of other adults do. In children, vaccination rates have declined in recent years, with fewer than 50% receiving the vaccine last year.
Flu Shot: Why Flu Vaccines Matter
Flu vaccines may not prevent every infection, but they are highly effective at reducing severe illness and hospitalizations, says Dr. Sean O’Leary of the American Academy of Pediatrics. Tens of thousands of Americans die from the flu annually. During last year’s severe season, 280 children died from flu-related complications, nearly half of whom had no prior health issues, and most had not been vaccinated.
A rare but serious complication from last season was brain inflammation, which can cause seizures, hallucinations, or even death. Most affected children were unvaccinated.
Flu Shots During Pregnancy Offer Dual Protection
Pregnant women need to be especially cautious. A severe flu infection can lead to hospitalization or even preterm birth. Vaccination protects both mother and baby, since infants too young for their own vaccines benefit from the mother’s antibodies. Research shows flu shots are safe and effective during pregnancy.
Flu Shot: Choosing the Right Vaccine
For adults 65 and older, high-dose flu shots or vaccines with immune boosters are recommended, though a standard flu shot is also effective if those options are not available.
Flu Shot: Cost and Insurance Coverage
Flu shots are generally free under Medicare, Medicaid, and most private insurance plans if administered through in-network providers. Local health departments may also offer low-cost or free vaccines. The at-home FluMist option may require a delivery fee, though insurance should cover the vaccine itself.
Getting a Flu Shot Alongside COVID-19 Vaccine
It is safe to get both the flu and COVID-19 vaccines at the same time. Dr. Philip Huang, director of Dallas Health and Human Services, says this is a convenient way to stay protected. However, availability of COVID-19 vaccines for children may be limited, as federal recommendations have shifted and parents are encouraged to make personal decisions.
4 Early Signs of Colon Cancer You Cannot Ignore, According To Doctor 'See Doctor Soon'

(Credit-Canva)
Bowel cancer, also called colon or rectal cancer, is one of the most common cancers. It is the fourth most common cancer in the United States, and around 150,000 Americans are diagnosed with colorectal cancer every year, according to the Colorectal Cancer Alliance.
The time it's found makes a huge difference in how well a person does. Catching the disease early makes a huge difference in survival.
If the cancer is caught in the very first stage (Stage One), people have a 90% chance of living for five years or more. That's excellent odds. But if it's found much later (Stage Four), the chance of living five years or more drops to only 10%. The lesson is clear: early checking and spotting symptoms can save lives.
Key Early Warning Signs of Colon Cancer
A doctor known as "Dr. Ben", also known as Medicina y Mente online has highlighted four main signs that could point to early bowel cancer. He stressed that if you see these, you should go to your doctor as soon as possible, especially since some of these symptoms only show up when you use the toilet. Here are the four key things to look out for:
Blood in your stool: This is one of the most common early alarms.
Changes in how you go to the toilet: This doesn't mean just one bad day. It means a big difference in your normal habits, such as going from being constipated (having hard, difficult-to-pass stool) to suddenly having diarrhea.
Losing a lot of weight for no reason: If you lose a significant amount of weight without changing how you eat or how much you exercise, it is a concern.
Feeling extremely tired (fatigue): This is tiredness that doesn't go away, even after rest. This is only a worry if there's no other clear reason for the tiredness.
What Are Some Other Symptoms Of Colon Cancer?
It's natural to feel shy, but the NHS strongly advises people to see a doctor if they have been experiencing any symptoms of bowel cancer for three weeks or longer. Doctors and nurses talk about these things all the time, so please don't be embarrassed. Other symptoms of colon cancer that the NHS mentions include:
- Bleeding from your bottom.
- The constant feeling like you need to go to the toilet, even if you just went.
- Pain in your tummy (abdomen).
- Feeling a lump in your tummy.
- Feeling bloated
- Feeling short of breath.
If your stool is very black or dark red, or you have bloody diarrhea, you need to call 111 or get an urgent appointment with your GP. While these symptoms don't always mean cancer, it is very important to get checked to find out what the problem is.
How To Prevent Colon Cancer?
The best defense against bowel cancer is screening. The NHS offers home testing kits for everyone between the ages of 50 and 74.
These home tests can be analyzed to look for tiny signs of cancer even before you feel sick or notice any symptoms. This is the most effective way to catch cancer at the earliest, most treatable stage.
© 2024 Bennett, Coleman & Company Limited

