- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
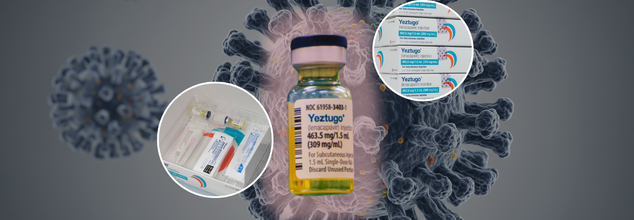
FDA Approves HIV Shot That’s 99.9% Effective; Is This The Beginning Of The End For The Viral Epidemic?
Credits: AP
The U.S. Food and Drug Administration (FDA) approved Yeztugo, a powerful, long-acting injection developed by Gilead Sciences, as a twice-yearly preventive treatment against HIV. The move has ignited widespread hope among global health advocates, signaling what many believe to be the dawn of a new era in HIV prevention.
With a 99.9% success rate in preventing HIV transmission in clinical trials, this injectable therapy formally known as lenacapavir, offers a revolutionary alternative to daily pills and could dramatically reshape the global HIV landscape.
Why Is HIV Drug Approval Such a Big Deal?
For more than 40 years, HIV has eluded a vaccine. While treatment has transformed HIV into a manageable chronic condition for millions, preventing new infections has remained a formidable challenge. Daily oral PrEP (pre-exposure prophylaxis), such as Truvada, has helped, but adherence is difficult for many especially in vulnerable populations.
That’s where Yeztugo changes the game. Its unique mechanism, longevity, and ease of use have the potential to overcome the barriers of daily pill regimens. Administered once every six months by a healthcare provider, it’s the longest-lasting PrEP option ever approved.
“This is a historic day in the decades-long fight against HIV,” said Daniel O’Day, CEO of Gilead Sciences. “We believe this marks a turning point.”
How Does Yeztugo Work?
Lenacapavir is not a vaccine. Instead, it is an antiretroviral that blocks HIV from infecting immune cells and replicating. What sets it apart is its ability to stay in the body for extended periods, providing protection for six months with a single shot.
Gilead conducted two major trials to test the drug’s efficacy in over 2,000 cisgender women in sub-Saharan Africa, the injection showed 100% prevention of HIV infection.
A parallel trial involving men who have sex with men and gender-diverse individuals showed a 99.9% effectiveness rate, with only two breakthrough infections. These outcomes, published in The New England Journal of Medicine, led Science to name lenacapavir its 2024 “Breakthrough of the Year.”
Reported side effects were minimal, limited mostly to injection site irritation, headaches, and nausea.
How The New Drug Affects HIV Treatment And Prevention?
Interestingly, lenacapavir didn’t start as a preventive drug. It was initially approved in 2022 (under the brand name Sunlenca) for treating drug-resistant HIV.
Researchers at Gilead quickly recognized two features that made it ideal for prevention: its long half-life and its ability to disrupt multiple stages of the HIV life cycle.
“We saw a fantastic protective effect after just one injection—even in non-human primate studies,” said Tomas Cihlar, Gilead’s VP of Virology. “That’s when we realized we had to pursue prevention aggressively.”
Could This Replace HIV Vaccine?
In many ways, yes—at least for now. While lenacapavir isn’t a vaccine in the traditional sense, its efficacy closely mimics one. And since traditional HIV vaccine development has repeatedly hit roadblocks, some experts believe lenacapavir may be the next best thing.
“Lenacapavir used by itself for prevention is a huge breakthrough,” said Dr. David Ho of Columbia University, a pioneer in HIV research. “Its potential to curb the epidemic is enormous.”
Yet ironically, the drug’s success could make it harder to develop a conventional vaccine. Why? Because it would now be unethical to assign people a placebo in vaccine trials when such a highly effective alternative exists.
Is There A the Catch?
While the science is exciting, several real-world challenges could stand in the way of Yeztugo’s success, cost, access, and policy chief among them.
Previous injectable PrEP options like cabotegravir, approved in 2021, came with hefty price tags and have yet to make a meaningful global impact. Gilead has not yet announced pricing for Yeztugo, but there’s concern it may follow suit.
Additionally, logistical barriers remain. Yeztugo must be administered in a clinic by a healthcare provider and requires that recipients test negative for HIV before each shot. That’s a significant hurdle for high-risk individuals in low-resource settings.
“There’s huge promise here, but we’ve built a jet without a runway,” said Hui Yang of the Global Fund to Fight HIV, TB, and Malaria. “If we don’t address distribution, affordability, and systemic barriers, the science won’t matter.”
Who Gets Access To HIV Injection?
Gilead has signed royalty-free licensing deals with six manufacturers to produce lenacapavir generics in 120 low- and middle-income countries. But critics point out that many middle-income nations, such as some in Latin America, are left out.
Meanwhile, in the U.S., states with strong support for PrEP programs have already seen a 38% decline in HIV infections. In contrast, states without similar support saw a 27% increase, according to The Lancet HIV.
With Medicaid cuts looming and the Supreme Court considering a case that could overturn the requirement for insurers to cover PrEP without copays, the long-term reach of Yeztugo may be compromised.
“We could be standing on the verge of eliminating new HIV infections,” said Carl Schmid of the HIV+Hepatitis Policy Institute. “But without the right policies, this will remain a medical miracle out of reach for too many.”
What Comes Next In the HIV Battle?
Gilead is already working on a once-a-year formulation of lenacapavir to make prevention even more accessible. The Global Fund aims to reach two million new PrEP users in the next three years, and Yeztugo could be pivotal to that goal.
There’s also ongoing research into self-administered versions of the injection, which would help reduce the need for in-clinic visits—especially vital for reaching marginalized populations.
The FDA’s approval of Yeztugo is more than a regulatory milestone—it’s a paradigm shift in HIV prevention strategy. Whether this breakthrough can live up to its promise will depend on how quickly and equitably it can be delivered.
What Is Acute Gastroenteritis? The Gastric Issue Real Madrid’s Star Footballer Kylian Mbapp Was Hospitalized For

Football fans around the world were stunned when Real Madrid confirmed that Kylian Mbappé, its French captain and marquee signing, was hospitalized for an acute bout of gastroenteritis during the Club World Cup. Although Real Madrid had originally reported that he was absent for the initial match because of illness, there was a formal medical report that confirmed the extent of his illness and in-hospital treatment and tests he required.
Even though Mbappé is recovering now with specific medical treatment outside the hospital, his sudden health fright focused fresh public attention on a prevalent but poorly understood illness: acute gastroenteritis.
What Gastroenteritis?
Gastroenteritis is the inflammation of the stomach and intestines that causes vomiting, diarrhea, cramps in the abdomen, and occasionally fever or muscle pain. Commonly called the "stomach flu," it is not caused by the flu virus and has nothing to do with respiratory infections. Rather, it is usually caused by infection or chemical irritants to the gastrointestinal (GI) tract. There are two main types:
- Infectious gastroenteritis – due to viruses, bacteria, parasites, or fungi.
- Chemical gastroenteritis – due to ingestion of poisonous substances such as some drugs, alcohol, or polluted food/water.
Mbappé's illness is an acute gastroenteritis, which means the symptoms came on suddenly and intensely but would likely pass with good care.
How Gastroenteritis Spreads?
The most prevalent reason for gastroenteritis is the intake of contaminated food or water. It is also spread by contact with infected people or surfaces they have contacted. Some typical situations include:
- Consumption of undercooked meat or seafood
- Inadequate washing of hands after using the toilet
- Drinking unbottled or unfiltered water during travel
Though most individuals recover quickly, individuals with compromised immune systems—such as young children, elderly, or those with chronic diseases—are at a higher risk for developing complications like dehydration and extended illness.
Symptoms Of Gastroenteritis
Acute gastroenteritis usually presents with a combination of the following:
- Sudden onset of watery diarrhea (non-bloody)
- Nausea and vomiting
- Abdominal cramps or bloating
- Low-grade fever
- General fatigue or muscle aches
These symptoms typically occur within 1–3 days of contact with the infection and can last anywhere from 24 hours up to two weeks, depending upon the cause and the immune response of the patient.
In the Mbappé case, the symptoms were bad enough to need hospitalization, which is not usual but required for observation of dehydration, electrolyte disturbances, or ongoing vomiting.
What Causes Gastroenteritis?
The origin of gastroenteritis comes from the inflammatory reaction in the body from a threat within the gastrointestinal system. Pathogens or toxic chemicals entering the system will have the immune reaction summon inflammation to combat invaders and heal damage.
In a majority of instances, it is an acute and transient condition. But if the infection is especially virulent or if the immune system of the body is weakened, inflammation becomes intense, aggravating symptoms and necessitating medical attention. The most common offenders are:
- Viruses (such as norovirus and rotavirus)
- Bacteria (E. coli, Salmonella, or Campylobacter)
- Parasites (Giardia)
- Fungi (uncommon but potential in immunocompromised hosts)
How Serious Is Acute Gastroenteritis?
For otherwise healthy people, acute gastroenteritis is usually self-limiting and resolves with rest and hydration. For elite athletes such as Mbappé, any alteration in the body's fluid and nutrient balance can have a profound impact on performance and recovery. The disease becomes more severe when:
- Dehydration occurs from heavy vomiting and diarrhea
- The symptoms do not improve after a few days
- There is the presence of blood in stool
- There's a loss of ability to retain fluids
- Fever is severe and persistent
In such instances, hospitalization is advisable—as in Mbappé's case—for rehydration, electrolyte balance, and observation.
What You Can Do to Stay Safe?
Although not all gastroenteritis cases can be avoided, the risk may be drastically cut down by sensible and preventive hygiene practices. Here's how:
1. Practice Proper Handwashing
Hand washing with soap and water for 20 seconds or more, particularly before eating and after using the bathroom, is one of the best means of preventing the transmission of GI infections.
2. Safe Food Handling
Do not cross-contaminate when handling food, thoroughly cook meat, and refrigerate perishables immediately. Wash fruits and vegetables before eating.
3. Safe Water to Drink
While traveling, use sealed bottled water, don't drink ice in beverages, and eat only cooked or packaged food to minimize the risk of "traveler's diarrhea."
4. Clean Surfaces
Disinfect surfaces frequently in shared spaces such as gyms, bathrooms, or kitchens to stop the spread of infection.
5. Watch Out for Medication and Drug Use
Excessive alcohol or certain medications use can irritate the lining of the gut and lead to chemical gastroenteritis.
While Kylian Mbappé will soon return to action, his recent hospitalization is a reminder that even the best professional athletes are not beyond the reach of diseases such as gastroenteritis. It also emphasizes the value of early treatment and medical surveillance in more complicated instances.
For the general public, it is imperative that they know about the causes, symptoms, and prevention of gastroenteritis—particularly with increasing travel and food safety as an ongoing global issue. With the right information and good hygiene techniques, most instances of gastroenteritis can be prevented or treated at home. But learning when to seek assistance—such as Mbappé's medical team—is what can turn the tables.
Acute gastroenteritis is widespread, but its effect can be from mild disruption to severe health risk depending on how it is handled. As a world-class sportsman or an average person coping with day-to-day well-being, early recognition of the symptoms, fluid intake, and attention to food and hygiene safety can keep you one step ahead of this miserable but avoidable illness.
Do Covid-19 At-Home Tests Detect The New Variants?

(Credit-Canva)
In many ways COVID-19 has changed the way medicine and treatments work. During peak COVID wave, at-home test kits became a more accepted part of medical care for people, as stepping outside and visiting hospitals could also cause infection. As new strains of COVID keep mutating, many people have brought up concerns regarding the effectiveness of the at-home tests.
The concern is regarding the fact that these at-home test kits are equipped to diagnose the new strains or are there certain strains that can go undetected.
How At-Home COVID Tests Work?
If you start feeling sick with symptoms like a cough, fever, or runny nose, you might worry if it's COVID-19. A simple way to check is by using an at-home COVID-19 test. You can easily find these tests at drugstores, supermarkets, and online stores.
At-home COVID-19 tests are designed to find tiny parts of the SARS-CoV-2 virus, which causes COVID-19. These parts are called antigens. Rapid at-home antigen tests usually give you results in about 15 minutes. If your test is positive, it's very likely you have the virus.
It's important to know that these tests can sometimes give a false negative, meaning you could test negative but still have the virus. However, because these tests are quick and rarely give a false positive, they can be very useful if used correctly.
Do They Work Against New COVID Variants?
At-home COVID tests should work against newer versions of the virus, “The antigen, that the at-home tests look for has remained fairly stable even as the virus mutates and new strains of COVID develop”. Harvard Health experts explain that the part of the virus these tests look for stays pretty much the same, even as the virus changes. Research generally shows that these antigen tests are good at finding different COVID-19 variants.
In a comparative study published in the Microbiology Spectrum journals, researchers looked at 2 types of tests PCR test and rapid antigen tests (Ag-RDTs). They used FIA which is the flourescence immunoassay, a simple and rapid technique that is used to measure compounds like drugs, hormones and proteins and LFIA which is lateral flow immunoassay, that is also used to detect proteins, haptens (a type of molecules), nucleic acids etc. Both rapid tests were 100% accurate at finding the virus when there was a lot of virus in the sample. However, their ability to find the virus dropped to around 30% when there was only a small amount of virus present.
This study confirms that rapid antigen tests (especially FIA and LFIA) work almost as well as RT-PCR tests for finding SARS-CoV-2. The FIA test was particularly good for people who had the virus but no symptoms. Both rapid tests agreed strongly with the gold standard RT-PCR results.
When to Test for COVID?
Harvard Health experts advise using an at-home COVID test if you have respiratory symptoms like a cough, fever, or runny nose. She also suggests testing if you've been around someone with COVID-19, or if you're going to be near elderly people or those with weak immune systems who could get very sick from the virus.
In general, these tests are most effective when you have symptoms. One study found that certain at-home tests caught almost 90% of COVID cases in people with symptoms, but only about half of cases in people who had the virus but no symptoms.
If your test is positive, it means you have the virus. If it is negative, health authorities recommend taking another test 48 hours later to reduce the chance of a false negative.
If you have respiratory symptoms, these combination tests are an easy way to find out if you have the flu, COVID-19, or both, without needing to visit a doctor's office. You can also help public health efforts by reporting your test result (whether it's positive or negative) online.
The best way to protect yourself from both COVID-19 and the flu is to get vaccinated for both. Vaccines lower your risk of getting sick and developing serious complications if you do catch the viruses.
Wildfire Smoke Could Fuel Flu And COVID-19 Outbreaks

(Credit-Canva)
Wildfires are a big concern for US citizens. Since the beginning of 2025, 31,039 wildfires have consumed 1.3 million acres of US land, according to the National Interagency Fire Center. Wildfires are uncontrolled fires that burn wildland and often rural areas. These fires can exhaust forests, grasslands, and many other ecosystems. With the amount of smoke generated, wildfires can severely affect the health of people.
A new study suggests that wildfires might indirectly raise the risk of flu and COVID-19 outbreaks. The smoke from wildfires often forces people to stay indoors, and when more people are gathered in enclosed spaces, infectious diseases can spread more easily. This finding was recently published in the journal PLOS Climate.
Why Staying Inside Puts You at Higher Risk
When wildfires burn, the air outside gets filled with smoke, making people go indoors. This creates perfect conditions for illnesses like the flu to spread, as a researcher from Georgetown University explained. With more people packed together, germs can jump from one person to another more easily. But there's a simple way to lower this risk: just wearing a mask indoors can help a lot.
Following People's Movements During Wildfires
Researchers looked at mobile phone data to see where people went during wildfires. This data showed visits to over 4.6 million places across the U.S., both inside and outside. They focused on the wildfire season in Oregon and Washington in 2020. By checking air quality, they found the areas worst affected by smoke. During that time, especially in August and September 2020, widespread wildfires caused a lot of smoke in these states.
More People, More Risk
The study found a clear increase in indoor activities when the wildfires were burning. In counties across Oregon, indoor activity went up by 14%, and in Washington counties, it increased by almost 11%. Major cities also saw a significant jump: Seattle experienced a 16% rise, and Portland saw an 11% increase in people spending time indoors. This shift means more people were confined together.
Using computer models, the researchers confirmed that more people indoors raises the risk of infectious diseases spreading, especially for highly contagious illnesses like flu and COVID-19. But these models also showed that wearing masks indoors can help slow the spread. They found that even a small increase in mask wearing (just 10% more people) could lower the number of new cases during wildfires. In areas hit hardest by smoke, like parts of Oregon and Washington, more than half the people might need to wear masks to effectively control the disease.
Preparing for Health Risks in a Changing Climate
The researchers advise public health experts to be aware of this connection if wildfire smoke reaches their communities. They should also warn people about the higher risk of infection. The study emphasized that as we face more extreme weather events, our public health plans need to change. We have to address not just the direct environmental harm from wildfires, but also how people react and adapt to these emergencies. By understanding how people behave and planning for it, we can better protect everyone's health in a world where extreme events are becoming more common.
© 2024 Bennett, Coleman & Company Limited

