- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
First Sign Of Diabetes Might Show Up In Your Eyes—Here’s What To Look For

Credits: Freepik
Diabetes is known for its impact on blood sugar but one of the first and often overlooked warning signs may appear right in front of your eyes—literally. Changes in vision might be the first sign. These early signs of diabetes in eyes and diabetic eye symptoms often appear before traditional diabetes symptoms
The Centers for Disease Control and Prevention (CDC) reports that an estimated 30.3 million adults in the United States have diabetes, and nearly 90% of them have Type 2 diabetes—a condition in which your body becomes resistant to insulin and has difficulty regulating normal blood sugar levels. While the disease is usually linked to complications such as neuropathy or kidney disease, your eyes may be the first organ to exhibit signs of suffering.
The eye is a sensitive organ covered in a close network of blood vessels, particularly in the retina—the thin layer of tissue at the back of your eye that facilitates vision. High blood sugar levels over time can hurt these small blood vessels, making them become inflamed, leaky, or clogged. That's called diabetic retinopathy, and it's one of the first—and possibly most destructive—complications of diabetes.
Over one-third of working-age population with diabetes already have signs of diabetic eye disease, and it is still a major cause of blindness among this group. Many are also unaware they have it—until their eyesight is already compromised.
What is Diabetic Retinopathy?
Diabetic retinopathy often progresses painlessly and without any signs, at least in its early stages. That's why regular eye exams are so important—despite your vision appearing completely normal.
If left uncontrolled, diabetic retinopathy may result in impaired or even complete vision loss. Worse, the damage tends to be permanent. Early detection and therapy can slow or even prevent progression, but the secret is to be vigilant and preventive.
Early Signs of Diabetes in Eyes You Can't Ignore
Floaters
Tiny specks, cobwebs, or worm-like forms floating in your line of sight are usually harmless. But a sudden proliferation of floaters—particularly if there's blurred or obscured vision—may indicate bleeding into the retina, a symptom of diabetic retinopathy.
Dark Spots
Any dimming of vision or blind spots, especially in the central visual field, are warning signs. These "blockages of vision" can indicate swelling of the retina or hemorrhaging—and need to be seen by an ophthalmologist right away.
Blurred Vision
Changes in blood sugar levels can disrupt your eye's ability to focus, causing fleeting or ongoing blurring. This can make it harder to read, drive, or identify faces and can continue to get worse if left unchecked.
Vision Loss or Shadows
Partial blindness, i.e., reduced peripheral vision or inability to see in dim light, can be a sign of advanced retinopathy or retinal detachment. Vision can even black out for a short time—a warning of extreme vascular damage.
If you have any of these symptoms, even if you don't have diabetes, it is important to consult an eye care professional immediately.
What Causes Diabetic Eye Damage?
Diabetic retinopathy occurs when high blood glucose levels start damaging the tiny blood vessels of the retina—the light-sensitive nerve tissue at the back of the eye. The vessels can become clogged, leak fluid or blood, or cause new and fragile, abnormal vessels to grow through a process known as neovascularization. This cascade can result in swelling, inflammation, scarring, and, eventually, retinal and optic nerve damage. In bad cases, the retina can come loose or fluid will pool in the macula (the retina's center portion), producing a condition called macular edema. These issues can lead to permanent loss of vision if left untreated.
Even though any diabetic is susceptible to developing diabetic retinopathy, there are some populations that are particularly at risk. These include those with Type 1 and Type 2 diabetes, especially those with poorly managed blood glucose levels. Pregnant women who develop gestational diabetes and individuals who have had diabetes for longer than five to ten years have a higher risk of retinal complications. Those with coexisting conditions like high blood pressure or elevated cholesterol are at even greater risk, as these issues can accelerate the damage to blood vessels in the eyes. Research indicates that up to 75% of people with Type 1 diabetes will develop some form of retinopathy, while approximately 50% of individuals with Type 2 diabetes show signs—often within the first decade following diagnosis.
Can Diabetic Retinopathy Be Cured?
Regrettably, diabetic retinopathy has no cure. The condition can be prevented from worsening if intervention is made early. Thanks to the advancements in medical technology, a number of treatment avenues can be employed. Anti-VEGF injections are usually used to prevent abnormal vessels from growing on the retina. Laser therapy is also an effective method that involves destroying leaking vessels and preventing vision loss. In more serious instances, vitrectomy surgery might be necessary to eliminate scarring tissue or blood within the eye. Most importantly, the most important thing is to control diabetes properly—adhering to healthy blood sugar levels, blood pressure, and cholesterol can go a long way in preventing serious eye complications in the long run.
Protect Your Vision with These 3 Non-Negotiable Steps
If you’ve noticed floaters, blurriness, or dark spots, don’t dismiss them. These could be more than visual annoyances—they might be early cries for help from your body. Although it's clear that preventive care, lifestyle changes, and monitoring are your best weapons against diabetes-related blindness.
1. Prioritize Lifestyle Interventions
Exercise, proper diet, and weight control are important. Include low-impact activity such as walking, yoga, or swimming. Follow a diet with high fiber, antioxidants, and whole grains and reduce saturated fats and refined carbohydrates.
2. Monitor Blood Sugar and A1C Levels
Regular blood sugar checks and routine monitoring of A1C levels (which measure average glucose over three months) can help you detect and correct abnormal trends. Aim for an A1C below 7%, or as recommended by your healthcare provider.
3. Don’t Skip Eye Exams
Your diabetes care regimen should include a dilated eye exam once a year. These tests alone can detect early signs of diabetic retinopathy. More frequent examinations may be warranted if risks or symptoms rise.
Your vision is not simply a measure of how well you see—it's literally a window to your overall health. In some cases, eye problems might be the first sign that you have diabetes. That's why receiving regular eye exams—even in the absence of obvious symptoms—is a key component of preventive care.
Fact Check: Popular Hair Loss Treatment Ingredient Could Trigger Chest Pain

Credits: iStock
Rebecca Pinto, physiotherapist and nutritionist shared a video on her Instagram account where she cites a case of a man who used hair loss treatment and was admitted to hospital on complain of chest pain. She points out that not everything that is available over the counter is safe to use. She says the key ingredients in many easily available hair loss treatment is minoxidil, which could trigger chest pain or angina as it can lower blood pressure.
Health and Me spoke to Dr Sanjay Bhat, Sr Consultant, Interventional Cardiology at Aster CMI Hospital, Bengaluru to fact check this claim and here is what we found out.
Also Read: AIIMS And ISRO Sign MoU To Advance Research In Space Medicine
Fact Check: Can Minoxidil Cause Severe Chest Pain?
Health and Me asked Dr Bhat if this easily available ingredient could actually cause someone’s life. To this, Dr Bhat explained that it is a commonly used medicine for treating hair loss and is easily available in many pharmacies as a topical solution or form. He said it works by improving blood flow to the hair follicles and helping hair grow. “When used on the scalp as recommended, it is generally safe for most people. However, long-term or excessive use may sometimes cause side effects. Some people may absorb a small amount of the medicine into the bloodstream, which can affect the heart and blood vessels,” he explains.
This could lead to symptoms such as chest pain, rapid heartbeat, dizziness, swelling of the hands or feet, or low blood pressure. “In rare cases, people may go to the emergency room if they feel severe chest discomfort or palpitations. Long-term use without medical advice may also cause scalp irritation or unwanted hair growth on other parts of the body. Therefore, it is important to use minoxidil only as directed and consult a doctor if unusual symptoms appear,” he said.
What To Do If You Feel Chest Pain While Using Minoxidil?
Doctor explains, “If a person develops chest pain after using Minoxidil, the first step is to stop using the medicine and seek medical attention immediately. Doctors will first evaluate the patient to make sure the chest pain is not due to a serious heart problem. This usually includes checking blood pressure, heart rate, oxygen levels, and performing tests such as an electrocardiogram (ECG) and blood tests.”
If minoxidil is suspected to be the cause, treatment mainly focuses on managing the symptoms. Doctors could also give medicines to control heart rate, reduce palpitations, or stabilize blood pressure. Depending on the reports, if the patient has fluid retention or swelling, diuretics may be prescribed to remove excess fluid from the body. Patients may also be monitored in the hospital for a short time if symptoms are severe. Once the symptoms settle, doctors usually advise avoiding minoxidil and may suggest safer alternative treatments for hair loss.
Are There Any Alternative Hair Loss Treatment Without Minoxidil?
The answer is yes. Dr Bhat points out Finasteride, an oral medicine to be one of the common alternatives to minoxidil for hair loss treatments. This medicine works by reducing the hormone DHT, which is linked to male pattern baldness. This also helps in slowing down the hair loss and promoting regrowth.
Platelet Rich Plasma Therapy: This is another alternative available points out Dr Bhat. This is when blood is processed and injected into the scalp to stimulate hair follicles and improve hair thickness.
He also pointed out that doctors often recommend Low Level Laser Therapy, which is a painless treatment using red light lasers to improve blood flow to hair follicles and encourage hair growth.
Lastly, Hair Transplant Surgery is another option for people facing significant hair loss, where follicles from one part of the scalp are moved to bald areas.
“In addition, treatments such as microneedling, nutritional supplements, and treatment of underlying medical conditions may also help improve hair growth,” points out Dr Bhat.
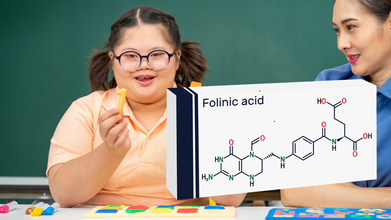
Leucovorin Prescriptions Surge After White House Mentions It For Autism Use, Parents Struggle To Find Drug
Credits: Canva and iStock
Leucovorin, a high-dose vitamin - folinic acid, were mostly used for treating toxic side effects of chemotherapy, until last year when the White House touted it as a potential treatment for some children with autism. New prescriptions for leucovorin double within weeks of announcement and parents have been trying hard to get it prescribed. This is also because many doctors have been hesitant to prescribe a chemotherapy medicine for childhood autism. They have also stated that not enough evidence is available to prescribe this drug officially.
CNN reported that in Austin, Texas, Meagan Johnson spent four days calling pharmacies across the region searching for leucovorin for her three-year-old son Jack, who has autism. She contacted nearly 40 pharmacies around her home in Pflugerville, hoping to locate the medication.
The effort came after a neurologist agreed to prescribe leucovorin on a trial basis. Johnson’s hope was simple: even a small improvement in her son’s communication would mean a lot. At age three, most children can say hundreds of words, but Jack speaks only about 20, many of which only his mother understands.
However, getting the prescription turned out to be far harder than obtaining it.
Across the United States, pharmacies have been reporting growing difficulty keeping leucovorin tablets in stock. Online support groups for parents of autistic children are now filled with posts from families searching for the medication or asking where it might still be available.
Although leucovorin is not approved specifically for autism, some small studies have suggested that it may help certain children who have unusually low levels of folate in the brain. Families who have tried it report possible improvements in language and social interaction.
A study published in The Lancet found that prescriptions for leucovorin doubled within weeks of the public remarks and remained elevated through early December. Researchers analysed electronic medical records covering nearly 300 million patients to identify the trend.
Experts say such spikes can quickly strain the supply of inexpensive generic drugs.
A Classic Demand-Driven Shortage
Pharmacy supply specialists describe the leucovorin situation as a demand-side shortage. Unlike manufacturing disruptions, these shortages happen when demand rises faster than manufacturers can increase production.
Generic drug manufacturers typically plan production schedules a year or more in advance. Because leucovorin had historically been a niche medication, companies were not prepared for a sudden surge in prescriptions.
As demand increased, pharmacies began running out of tablets. Many manufacturers have placed the drug on allocation or backorder, meaning pharmacies can only order limited quantities.
To ease the pressure, the US Food and Drug Administration allowed temporary imports of leucovorin tablets from Canada and Spain. However, the drug has not yet been officially listed on the FDA’s national drug shortage database, a designation that could trigger additional measures to boost supply.
Families Searching For A Treatment
For parents like Johnson, the debate over research evidence matters less than the possibility of progress.
After days of phone calls, a CVS pharmacist finally located a supply at another branch nearly an hour away. Johnson drove the distance to pick up the medication and gave Jack his first dose that same evening.
The moment brought relief, but also frustration.
Drug shortage advocates say the situation was predictable. Because leucovorin is inexpensive and historically prone to shortages, any sudden increase in demand could easily disrupt supply.
Still, families continue to search for it.
Parental Stress Can Lead To Childhood Weight Gain, Experts Say

Credits: Canva
Childhood obesity has been rising steadily across the world, including in India. According to the World Health Organization, the number of children aged 5 to 19 who are overweight or obese has increased more than tenfold over the past four decades.
In India, the Indian Council of Medical Research reports that about 14 percent of children aged 6 to 19 are overweight or obese, with higher rates in urban areas.
Many efforts to prevent obesity focus on healthy eating and physical activity. While these remain essential, research increasingly shows that the stress levels of parents can play a big role in shaping children’s health outcomes.
Stress, simply put, is when the body feels under pressure. Mentally, emotionally, or physically. Parents under stress may have less patience, lower energy, and less ability to maintain healthy routines for their family.
How Parental Stress Leads Childhood Obesity
According to Dr Elissa Epel, a psychologist at the University of California, San Francisco, chronic stress can lead to increased production of cortisol, a hormone that regulates energy and appetite. Higher cortisol levels can make both adults and children crave sugary and fatty foods, which leads them to store more fat in the body.Additionally, a Obesity Reviews 2017 study also found that parents who suffer from high stress levels are more likely to have irregular eating patterns, snack on unhealthy foods, and engage in less physical activity, which contributes to stressful home environments.
This often leads to a pattern of “comfort eating” and fewer structured meal routines in the house, habits that can be easily picked up and adopted by children. This can pave the way for multiple chronic conditions to develop early on in young children.
Socioeconomic pressures can also worsen the risk of obesity in youngsters. Families experiencing financial stress, job insecurity or long working hours may rely more on convenient fast foods or skip family meals altogether.
According to the World Health Organization (WHO), diet and lifestyle patterns learned in early childhood often persist into adolescence and adulthood, which makes early interventions critical.
How Parenting Styles And Household Atmosphere Matter
Parenting style also plays a crucial role in managing childhood obesity. Warm, attentive, and consistent parenting helps children learn healthy habits, regulate their emotions, and develop self-control. Conversely, stressed or overwhelmed parents may struggle with patience and consistency.A 2020 study in Pediatric Obesity showed that children whose parents reported higher stress levels were more likely to gain excess weight over two years compared with children whose parents reported lower stress.
The home environment can shape a child’s relationship with food. If meals are rushed, distracted, or emotionally tense, children may associate eating with stress rather than nourishment. On the other hand, family routines that include relaxed meals, shared cooking, and parental involvement in active play are linked to healthier weights and better mental health outcomes.
Steps Parents Can Take To Monitor Obesity
Reducing parental stress is not about being perfect. It is about creating a balanced environment where healthy habits can thrive. Experts recommend strategies such as:- Mindfulness and relaxation techniques: Simple breathing exercises, meditation, or even quiet reading time can lower stress levels. Psychologist Susan Albers notes that mindful parenting improves parent-child interactions and can reduce unhealthy eating patterns.
- Structured routines: Regular meal times, scheduled physical activity, and predictable sleep patterns create stability for children.
- Self-care: Parents who prioritize sleep, exercise, and mental breaks are better able to support their children’s health.
- Healthy family meals: Cooking together, reducing ultra-processed foods, and encouraging fruits and vegetables fosters both nutrition and bonding.
It’s important to note that stress management alone is not enough. Combining emotional support for parents with healthy eating and activity habits is the most effective approach. The American Academy of Pediatrics highlights that integrated strategies addressing diet, activity and family wellbeing can reduce childhood obesity risk more effectively than focusing on nutrition or exercise alone.
Why This Matters For The Future
Childhood obesity is a complex problem with multiple causes - genes, environment, lifestyle, and now, stress at home. By recognizing that parents’ mental health influences children’s physical health, families, schools, and health practitioners can take a more holistic approach to prevention.The impact of a calm, supportive home can be profound. When parents manage stress, children not only eat better and move more, but they also develop emotional resilience and lifelong healthy habits. As Dr. Epel explains, “A child’s wellbeing often mirrors the adult they live with: less stress in parents can mean a healthier start for children.”
© 2024 Bennett, Coleman & Company Limited

