- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Gamer’s Neck Develops 'Dropped Head Syndrome' After Years Of Looking At His Phone, Doctors Warn Of Debilitating Condition
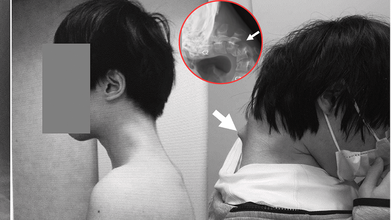
Credits: JOS Case Reports
When was the last time you caught yourself hunched over your phone, neck bent at an unnatural angle? A few minutes scrolling might feel harmless, but for one 25-year-old gamer in Japan, years of that posture ended with a shocking diagnosis, “dropped head syndrome.” His story has left doctors urging young people worldwide to rethink how long they spend staring down at their screens.
In a striking case that has unsettled health experts, Japanese doctors documented how a 25-year-old man grew a serious case of "dropped head syndrome" after years of crouching over his smartphone playing video games. The debilitating but unusual condition left him unable to lift his head, properly swallow food, or sustain a healthy weight.
In the case report released in JOS Case Reports in 2023, the patient's battle started following years of isolation from society in his teenage years. Having endured constant bullying at school, he isolated himself in his bedroom and spent many hours glued to his phone playing games, with his head leaning forward at steep angles for hours on end.
How Smartphone Overuse Weakened His Neck?
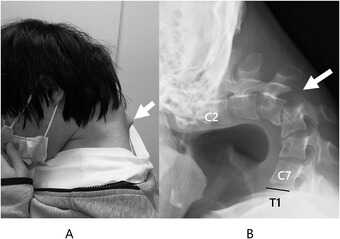
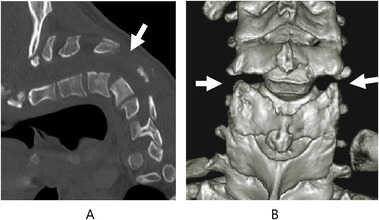
The injury was chronic. For six months, the man suffered from excruciating neck pain before he lost all ability to lift his head. His vertebrae deformed and dislocated over time, scar tissue in his spine formed, and he had trouble swallowing, leading to spectacular weight loss.
Scans established that his cervical spine had been subjected to extreme stress through unnatural posture over many years. The muscles and ligaments that were meant to keep the head upright no longer worked, and his chin would sag onto his chest.
The doctors first tried to treat it conservatively using neck collars, but the patient complained of numbness and pain, compelling the team to embark on surgery.
How Did The Doctors Treat 'Dropped Head Syndrome'?
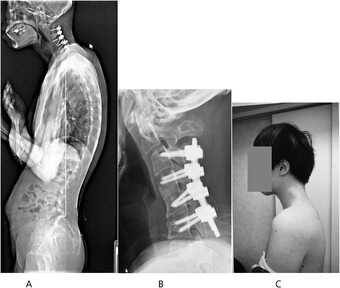
Surgeons carried out an intricate procedure that entailed removing bruised bits of vertebrae and scar tissue, followed by the implantation of metal rods and screws to stabilize and realign the spinal posture. Six months passed before the patient regained the ability to keep his head level.
At one-year follow-up, swallowing problems had cleared up, posture was stable, and quality of life had dramatically improved.

The group concluded that the condition was caused by an "underlying developmental disorder" but that the long-term consequences of prolonged smartphone use with this posture were the biggest contributor to his illness.
What Is Dropped Head Syndrome?
Dropped head syndrome (DHS), also referred to as "floppy head syndrome," is an uncommon disorder that involves, at times severe, weakness of the neck muscles, resulting in a "chin-on-chest" posture.
It is most commonly linked to neuromuscular disorders like amyotrophic lateral sclerosis (ALS), Parkinson's disease, or specific muscular dystrophies. The patients tend to use their hands to support their heads and can have difficulties with eating, talking, and walking.
In ALS, DHS happens in approximately 1–3% of the patients and is typically progressive with a grim prognosis. But as this Japanese case suggests, DHS may also arise due to non-neurological etiologies such as trauma, drug abuse, or—as in this instance—chronic mechanical stress of posture.
Can Screen Time Be Associated With Dangerous Conditions?
Although this instance is unusual, physicians caution it shows an expanding medical danger associated with mobile phone addiction. Over 6.8 billion individuals across the globe currently have access to smartphones, with four to seven hours of average screen time per day. Among game players and youth, use can be much higher.
Protracted downward neck posture—a sometimes termed "tech neck"—is already associated with headache, eye strain, and degeneration of the cervical spine. This is the extreme example of DHS and serves to illustrate how serious the effects can be when posture is neglected.
How Does Dropped Head Syndrome Affect Everyday Life?
DHS is more than just an inconvenient posture. The deformity affects simple functions such as swallowing, speaking, and breathing. It inhibits mobility, renders everyday activities challenging, and results in social withdrawal and isolation. In younger individuals, it even generates a chain of physical disability that multiplies mental health issues.
In this patient's life, bullying during childhood and later ostracism provided fertile ground for technological dependence. His case is particular about pointing to the juncture of mental well-being, online tendencies, and bodily well-being—a synergistic combination that is all the more pertinent in contemporary societies.
Organizations like the American Academy of Orthopaedic Surgeons have already warned of increasing incidence of posture-related spinal disorders in young people. The majority will never suffer from DHS, yet milder but chronic neck and back ailments are sweeping up teenagers and young adults.
Elizabeth Jarman from Médecins Sans Frontières, citing parallel access problems with diabetes care, emphasized that the first step to prevention is awareness. In the case of digital health, professionals are calling for schools, workplaces, and families to include posture education and frequent movement as part of daily practice.
Can Dropped Head Syndrome Be Prevented?
Prevention of dropped head syndrome due to posture is easy in principle:
- Avoid repetitive forward flexion of the neck.
- Take frequent breaks from screen time.
- Do neck-strengthening and posture-improving exercises.
- Employ ergonomically arranged seating and screen configurations.
But putting these measures into practice takes awareness and discipline—two qualities usually lacking in the fast-engagement era of mobile gaming and social media.
Is Surgery the Only Option for DHS Treatment?
For cases as bad as the Japanese gamer's, surgery is still the only real option. Surgical procedures are not without hazard, though, from infection to nerve damage. Even if successful, recovery is long and needs rigorous rehabilitation.
Due to the relative infrequency of DHS, there is no gold standard for surgical treatment. Each case has to be assessed on its merits, weighing risks against benefits.
This is an extreme case, but it is one that should serve as a warning to young people everywhere. The frequency of "tech neck" complaints in clinics, alongside rising screen time, indicates there could be more cases of spinal deformities emerging if awareness is not given high priority.
As the Japanese physicians who attended to the gamer stressed, the illness might have been precipitated by the integration of physical posture and pre-existing susceptibilities, but excessive use of smartphones in uncomfortable positions may produce unimaginably tragic results.
Could You Reverse Hair Loss And Regrow Bald Spots? New Chemical Agent Could Increase Hair Density by 20%

(Credit- Canva)
Hair is one of the key aspects of a person’s look. A simple haircut can completely change the way you look. So, you can imagine how losing one’s hair can affect them. While it happens to many people, it can completely change the way they view themselves. Although it is a normal part of aging, many men face this challenge from a young age due to many reasons like genetics, male-patterned baldness etc.
While there are ways you can tackle major hair loss like hair transplant, not everyone can afford it. However, a new drug called PP405 might be a game-changer for baldness. Instead of just slowing down hair loss, this new topical drug actually helps "wake up" your hair follicles that have gone to sleep. In early tests, it showed promising results, making hair thicker for some people who used it. If this treatment works in bigger trials, it could be a whole new way to fight baldness.
How the New Hair Growth Drug Works?
The new drug, PP405, is a topical cream that you apply to the scalp. It's different from older treatments because it doesn't just try to slow down hair loss. Instead, it works by waking up the hair follicles that have become dormant, or "asleep." Scientists found that in many people with hair loss, the stem cells in their hair follicles aren't dead—they've just stopped working. This new drug specifically targets these dormant cells to get them growing hair again.
In an early study, led by dermatologist Qing Yu Christina Weng, MD, chief medical officer of Pelage Pharmaceuticals, the results were very promising: some patients saw their hair become more than 20% thicker. The new hair wasn't just thin, "baby hair"; it was thick, mature hair. A key safety feature is that the drug is designed to get into the skin where it's needed without being absorbed into the rest of the body.
Can You Regrow Hair With Medicine?
Dermatologists are excited about the new drug's potential because it offers a completely new way to treat hair loss. However, they are also being cautious. The study so far was small and short, and the results haven't been fully checked by other scientists yet. The drug still needs to go through much larger studies, which could take a few years.
Right now, the only FDA-approved treatments for hair loss are finasteride and a topical solution called minoxidil. While doctors sometimes use an oral version of minoxidil, these treatments don't work for everyone, especially for those with severe hair loss. This leaves many people with limited options, often turning to expensive and unproven treatments like special injections or lasers.
Does The New Hair Growth Drug Work?
If PP405 passes its larger trials, it could be a huge breakthrough. It would be the first new FDA-approved hair loss treatment in over 25 years. This could be especially helpful for people who have more severe hair loss and haven't had success with other medications.
The researchers also believe this drug might one day be used to treat other types of hair loss, such as hair thinning caused by certain medications or hormonal changes. However, experts say that before the drug is used for other conditions, it must be thoroughly tested in larger groups of people to prove it is safe and effective.
Dermatologist Reveals Why Using The Same Skincare Day And Night Could Be Ruining Your Skin

Credits: Health and me
Your skincare shelf might be quietly sabotaging your glow—and you don’t even know it. Think about it: the same cream you swipe on at 7 a.m. is also applied at 11 p.m. But your skin isn’t static; it’s a living, breathing organ with different priorities depending on the time of day. Morning skin is on defense, battling sunlight, pollution, and blue light, while nighttime skin is in repair mode, regenerating and replenishing. Using the same products both times may be convenient, but convenience could come at the cost of healthier, radiant skin.
Skincare seems simple on the surface—wash, moisturize, repeat. Many of us follow the same routine morning and night, believing that if a product works once, it works all day. But according to dermatologist Dr. Vikram Lahoria, this approach may be doing more harm than good. Your skin operates on a circadian rhythm, and the way it behaves during the day differs significantly from its nighttime activities. Understanding these differences—and adjusting your routine accordingly can be the difference between healthy, glowing skin and clogged pores, premature aging, or irritation.
How Your Morning Skincare Is A Shield?
Dr. Lahoria explains, “During the day, your skin is exposed to sunlight, pollution, dust, and even the blue light from screens. Its main role is protection. That’s why your morning routine should focus on creating a barrier against these environmental stressors.”
A typical morning routine starts with a gentle cleanser to remove oils and sweat accumulated overnight. This is followed by a light, hydrating moisturizer that won’t feel greasy or clog pores. The most crucial step in your AM routine is sunscreen. No matter the weather, SPF shields your skin from UV rays, reducing the risk of premature aging, pigmentation, and even skin cancer.
Adding an antioxidant serum, particularly one with vitamin C, can further protect against free radicals generated by pollution and UV exposure. “Think of it as giving your skin armor before stepping into the world,” says Dr. Lahoria.
How Your Night Skincare Is To Heal and Recharge?
Once the sun sets and the day winds down, your skin switches gears. “Nighttime is when your skin works hardest to repair itself,” Dr. Lahoria notes. Without sunlight and environmental stressors, skin cells can focus on regeneration and replenishment.
Night creams and serums are designed to support this process. Ingredients like retinol, peptides, hyaluronic acid, and glycolic acid target fine lines, improve texture, and lock in moisture. A thorough cleanse is essential before applying these products to remove makeup, sweat, and dirt that could block pores overnight.
“Nighttime is when your skin absorbs products most efficiently. The lack of UV exposure means potent actives like retinol can work without the risk of sun-induced irritation,” explains Dr. Lahoria.
Why Using the Same Products All Day Can Backfire?
Using identical products morning and night ignores the skin’s shifting priorities. “It’s like feeding your body the same meal for breakfast and dinner,” says Dr. Lahoria. “In the morning, your skin needs protection. At night, it needs repair. One product cannot optimally serve both functions.”
Daytime exposure to retinoids or AHAs, for instance, can increase sensitivity to sunlight, potentially causing irritation, pigmentation, or damage. Conversely, using sunscreen at night is unnecessary, and while it won’t harm your skin, it doesn’t contribute to repair either. Tailoring your routine ensures that ingredients work when they are most effective, rather than canceling each other out or creating unintended side effects.
Why The Order of Products Is Important?
Timing is not the only consideration—the order in which you apply your skincare products matters too. Dr. Lahoria advises layering from thinnest to thickest. This ensures lightweight serums penetrate deeply before being sealed in by heavier creams or oils. Incorrect layering can hinder absorption or even reduce the efficacy of active ingredients.
For example, a vitamin C serum should be applied before moisturizer, while a heavier night cream should go last. By following this approach, each product can work as intended, maximizing benefits without waste or interference.
Personalising Your Routine to Your Skin’s Clock
Your skin, like your body, has a circadian rhythm. During the day, its priority is defense; at night, it focuses on repair. “Ever wonder why your skin behaves differently in the morning than it does at night? That’s your internal clock at work,” Dr. Lahoria points out.
Adjusting your routine according to this natural rhythm ensures your skin gets the right nutrients at the right time. In the morning, protect; at night, repair. Over time, this approach improves skin health, prevents premature aging, and enhances the results from the products you invest in.
Morning and Night Routine Tips
Dr. Lahoria summarizes an effective framework:
Morning:
- Gentle cleanser to remove overnight oils
- Light moisturizer for hydration
- SPF to protect against UV damage
- Optional antioxidant serum for pollution defense
Night:
- Thorough cleanse to remove dirt, makeup, and pollutants
- Serums or creams containing retinol, peptides, hyaluronic acid, or glycolic acid
- Night cream to lock in moisture and support cell repair
Following these guidelines ensures that your skin is supported according to its natural needs, rather than treated with a one-size-fits-all approach.
Skincare is not just about selecting the “right” products—it’s also about using them at the right time. Dr. Lahoria concludes, “Your morning and evening routines should act like a tag team. Each plays its role in protecting, repairing, and energizing your skin. Your clock isn’t just ticking, it’s guiding your glow.”
By understanding your skin’s natural cycles, choosing the right ingredients for day and night, and applying them in the correct order, you ensure your skin remains healthy, radiant, and resilient—without unnecessary irritation or damage.
Half of People With Diabetes Go Undiagnosed, Lancet Study Warns

(Credit- Canva)
A disease that globally affects people, numbers ranging in the millions, Diabetes is a silent killer that many people suffer with. 2022 stats showed that the number of people who were living with diabetes was 830 million, which steadily rose from the 200 million in 1990. According to the World Health Organization, more than half of the people who had diabetes live or are living without getting medication for it. A lot of them didn’t even know they had diabetes, and a recent study revealed how many exactly.
Before you know the number ask yourself a question: Do you know your blood sugar level?
This is a question that either people who have gotten their sugar levels tested would know, or cautious people who get regular check ups would know. A new study suggests that many people with diabetes don't, which could lead to serious health issues down the line. According to a study published in The Lancet Diabetes & Endocrinology, a staggering 44% of people aged 15 and older who have diabetes are undiagnosed.
The study, which looked at data from 204 countries, found that about one in nine adults worldwide has diabetes. In the U.S. alone, 11.6% of Americans have the condition. While higher-income countries are generally better at diagnosing people, the problem is widespread. Globally, only 56% of people with diabetes are aware of their condition.
Why Are So Many Diabetic People Undiagnosed?
A surprising finding is that younger people are much less likely to be diagnosed. Only 20% of young adults with diabetes know they have it. This is partly because routine screenings are more often recommended for people over 35. Many people with diabetes don't experience clear symptoms until complications—like heart, kidney, or nerve damage—start to appear, which is more common in older adults.
Early diagnosis is crucial. Experts say that knowing you have diabetes early allows for timely management that can prevent or delay these severe, long-term complications.
Many people with diabetes have no symptoms in the early stages, which is why regular screenings are so important. However, be on the lookout for these common signs:
- Increased thirst or hunger
- Frequent urination
- Blurry vision
- Unexpected weight loss
- Fatigue
Even after diagnosis, there's another challenge: proper management. The study found that only about 40% of people with treated diabetes were able to get their blood sugar under control. This highlights the need for better support and treatment plans to help people manage their condition effectively.
Can You Prevent Diabetes?
While you can't prevent Type 1 diabetes, you can significantly lower your risk of developing the more common Type 2 diabetes. Here are some simple steps you can take:
Improve your diet. Eat fewer red and processed meats, and incorporate more plant-based foods, like a Mediterranean diet.
Limit ultra-processed foods. Choose whole foods like fruits and nuts over highly processed snacks.
Stay active. Regular physical activity, such as a 15-minute walk each day, can lower your risk of developing diabetes and other chronic diseases.
© 2024 Bennett, Coleman & Company Limited

