- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
‘Grey’s Anatomy’ Star Opens Up About Hashimoto’s Hypothyroidism: Know How This Autoimmune Disorder Can Impact Body and Mind
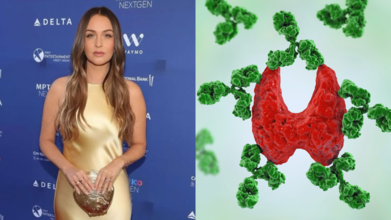
On her “Call It What It Is” podcast with co-star Jessica Capshaw, Grey’s Anatomy star Camilla Luddington revealed she had recently been diagnosed with Hashimoto’s hypothyroidism, an autoimmune condition that quietly messes with your thyroid and, by extension, your entire energy system.
Best known as Dr Jo Wilson, the 41-year-old Luddington admitted she had brushed off her constant tiredness, sluggishness, and need to curl up in bed as signs of getting older or hitting perimenopause. “Makes you a little slothy,” she joked, only half-serious. The truth was more complex and involved a surprisingly common yet under-discussed health disorder.
When “just tired” is something more
It started with a routine blood test. Her doctor spotted “one little thing” and, before she knew it, dropped the phrase “autoimmune disease” into the conversation. But the reassurance came quickly: Hashimoto’s is very common, especially among women in middle age.
Still, common does not mean harmless. Reportedly, Hashimoto’s slowly attacks the thyroid gland, the butterfly-shaped organ at the base of your neck that produces hormones controlling metabolism, temperature regulation, and a surprising list of bodily functions. Over time, the immune system’s misguided attack leads to a drop in hormone production, setting the stage for hypothyroidism.
The symptoms
Fatigue, dry skin, weight gain, and do not forget the cold intolerance, hair loss, and brain fog. According to the Mayo Clinic, these are just the tip of the symptom iceberg for Hashimoto’s, which can also cause constipation, muscle aches, joint pain, irregular menstrual cycles, depression, brittle nails, and even an enlarged thyroid (goitre). Sometimes symptoms creep in so gradually that people do not realise something is wrong.Luddington recognised several of these signs in hindsight, though she had been quick to explain them away. Now, with a diagnosis in hand, she’s on medication and back to exercising — a reminder that treatment can help restore some balance, even if there’s no cure.
Watch the video here:
Who’s at risk and why
Hashimoto’s can strike anyone, but middle-aged women top the risk list. Genetics may be part of the puzzle, along with environmental triggers like infections, chronic stress, or even radiation exposure.
And while the disease typically develops slowly, its reach is wide. If untreated, it can snowball into complications like heart problems, fertility issues, poor pregnancy outcomes, or a rare and life-threatening state called myxedema, where extreme hypothyroidism leads to unconsciousness.
The mental health connection
Hashimoto’s is not just a physical game-changer. Because thyroid hormones influence brain chemistry, untreated hypothyroidism can cause depression, anxiety, and severe mood changes. Luddington herself described feeling constantly run down, with a fatigue so deep it impacted her day-to-day life. This mental strain often gets overlooked, especially when symptoms overlap with other conditions.Treatment that works
Reportedly, thyroid hormone replacement therapy is the gold standard for treatment, often in the form of a daily pill that restores hormone levels. When managed well, it can make symptoms fade into the background. Lifestyle adjustments, such as regular exercise, good sleep habits, and balanced nutrition, can also help.
Luddington’s story is proof that a proper diagnosis can be life-changing and that even those with hectic Hollywood schedules need to listen to their bodies.
Why you shouldn’t ignore “little” symptoms
Feeling tired is not unusual. But when exhaustion comes with hair loss, weight changes, and a tendency to wear sweaters in 25-degree weather, it is worth checking your thyroid. As Luddington learnt, what seems like ordinary wear and tear can sometimes be a hormonal SOS.
If left untreated, Hashimoto’s can quietly chip away at your health for years, leading to cardiovascular risks, mental health struggles, and long-term organ strain. That is why timely diagnosis and treatment are not just medical niceties; they are essential.
The message is simple: fatigue is not always “just life”. Sometimes, it is your body asking for help and that call deserves an answer.
AI Chat Bots Are Giving Inaccurate Medical Advice, Says Study

Credits: Canva
As artificial intelligence becomes a go-to source for quick answers, a new University of Oxford-led study on AI chatbots and medical advice is raising serious concerns about how safe it is to rely on these tools for health guidance.
The research suggests that while AI chatbots can provide medical information, their advice is often inaccurate, inconsistent, and difficult for users to interpret, potentially putting people at risk—especially when dealing with symptoms that need urgent care.
What the Oxford Study Found
The study involved 1,300 participants who were given realistic health scenarios, such as experiencing a severe headache or being a new mother feeling constantly exhausted. Participants were divided into two groups: one group used AI chatbots to understand their symptoms and decide next steps, while the other did not.
Researchers then assessed whether participants correctly identified what might be wrong and whether they made appropriate decisions, such as seeing a GP or visiting A&E.
The results were troubling. People who relied on AI frequently failed to identify the severity of their condition and were often unsure about when to seek professional medical help.
Why Chatbot Advice Can Go Wrong
According to the researchers, one major issue is that people don’t always know what to ask. The study found that chatbot responses varied widely depending on how questions were phrased. Even small changes in wording could lead to completely different answers.
The AI often produced a mix of helpful and misleading information, leaving users to decide which advice mattered. Many participants struggled to distinguish between reliable guidance and unnecessary or confusing details.
As one of the study’s authors explained, when an AI lists multiple possible conditions, users are left guessing which one applies to them—precisely the moment where mistakes can happen.
A Dangerous Gap in Symptom Interpretation
Dr Rebecca Payne, lead medical practitioner on the study, warned that asking chatbots about symptoms could be “dangerous”, particularly when users delay seeking professional care based on AI responses.
Dr Adam Mahdi, the study’s senior author, noted that while AI can share medical facts, people often share information gradually and leave out key details—something chatbots struggle to manage effectively.
Bias, Data, and the Limits of AI
Experts also point out that chatbots are trained on existing medical data, which means they may repeat long-standing biases baked into healthcare systems. As one psychiatry expert put it, a chatbot is only as accurate as human clinicians—and humans are far from perfect.
That said, not everyone is pessimistic.
What Comes Next for AI in Healthcare
Digital health experts argue the technology is evolving. Health-specific versions of general AI chatbots have recently been released by major developers, and these could perform differently in future studies.
The consensus among experts is clear: AI in healthcare should focus on improvement, regulation, and guardrails, not replacement of doctors. Used responsibly, it may support healthcare—but without safeguards, it risks doing more harm than good.
Is This Common Pregnancy Drug Linked To Cancer? Streeting Urges Public Inquiry

Credits: Harm and Evidence Research Collaborative and Association for Women In Science
This common pregnancy drug could be linked to cancer. Wes Streeting has been urged to launch a public inquiry into a miscarriage drug called Diethylstilbestrol, which, reports say has "ruined and devastated" the lives of countless women. On Monday, the Health Secretary Streeting met victims of the pregnancy drugs, which has been linked to cancer, early menopause and infertility.
What Is Diethylstilbestrol?
Diethylstilbestrol, commonly known as DES, is a synthetic form of female hormone estrogen, which was prescribed to thousands of pregnant women from 1940 to 1970s.
The drug was used to prevent miscarriage, premature labor and complications of pregnancy. This was also used to suppress breast milk production, as an emergency contraception and to treat symptoms of menopause.
What Is The DES Controversy?
In 1971, Diethylstilbestrol (DES) was linked to a rare cancer of the cervix and vagina known as clear cell adenocarcinoma, prompting US regulators to advise that it should no longer be prescribed to pregnant women. Despite this, the drug continued to be given to expectant mothers across parts of Europe until 1978. DES has also since been associated with other cancers, including breast, pancreatic and cervical cancers, The Telegraph reported.
Campaign group DES Justice UK (DJUK) is now urging Health Secretary Wes Streeting to order a public inquiry and introduce an NHS screening programme to identify people who may have been exposed to the drug before birth.
Victims described DES as “one of the biggest pharmaceutical scandals this country has ever seen,” warning that “the impact of this terrible drug cannot be underestimated as it has ruined and devastated so many lives,” according to The Telegraph.
In November, Streeting acknowledged that the “state got it wrong” and issued an apology to those affected. He also advised anyone who believes they may have been exposed to DES to speak to their GP.
Susie Martin, 55, from Manchester, whose mother was prescribed DES during pregnancy, told The Telegraph she has undergone between 20 and 30 operations as a result of the drug’s effects.
“The impact of this terrible drug cannot be underestimated as it has ruined and devastated so many lives, including my own,” she said. “The physical and emotional pain has been unbearable. I live with a constant fear that I will need more surgery or develop cancer—and I am far from the only one.”
Calling DES a “silent scandal,” Martin said she hopes the government’s engagement will lead to concrete action. “While I welcome Mr Streeting meeting us, it will only matter if he commits to meaningful steps for victims of this shameful chapter in British medical history, including a screening programme and a full statutory public inquiry,” she added.
What Is Happening With The DES Victims?
The Telegraph reported that compensation schemes have been set up for DES victims in the US and Netherlands, however, UK does not have one yet.
"There are harrowing accounts of harm caused by the historic use of Diethylstilbestrol (DES). Some women and their relatives are still suffering from the associated risks of this medicine which have been passed down a generation, and haven’t been supported. The Secretary of State has been looking seriously at this legacy issue and carefully considering what more the government can do to better support women and their families who have been impacted. NHS England has alerted all cancer alliances to this issue so that healthcare professionals are aware of the impacts of DES and the existing NHS screening guidance which sets out the arrangements for those who show signs and symptoms of exposure,” said a Department of Health and Social Care spokesman to The Telegraph.
WHO Montreal Meeting Focuses On Wearables As A Reliable Method Of Health Tracking, Doctors Welcome To Move

Credits: Canva/Amazon
The World Health Organization (WHO)'s Montreal meeting focused on wearable technology like smartwatches and activity trackers as a reliable source of health tracking. The meeting discussed that wearables could in fact generate objective real-time data, which helps governments design targeted and evidence-based health interventions.
Physicians in the Montreal meetings discussed that wrist-worn devices are more reliable than traditional self-reported surveys. This is because the self-reported surveys could underestimate the levels of physical inactivity.
“Metrics such as step count, moderate-to-vigorous physical activity and sedentary time directly correlate with cardiovascular disease, diabetes and mental health outcomes. Having population-level data allows for early and preventive strategies,” said Dr Venkat Nani Kumar, consultant in internal medicine.
WHO Montreal Meeting: How Have Doctors Reacted The Shift To Wearables?
Doctors in India have welcomed this shift to wearable devices as a better way to generate data and make policies. Dr Kiran Madhala, professor at Gandhi Medical College, Secunderabad, said WHO’s shift reflects rapid advances in artificial intelligence and digital health tools, calling it a progressive step towards improved monitoring of physical activity worldwide.
City-based doctors also underlined the need for inclusive validation of devices. “Wearables must recognise varied movement patterns and step equivalents, especially in ageing populations,” a physician said, while stressing the importance of data privacy and ethical use of health information.
WHO Montreal Meeting: What Are Wearable Health Devices?
As per a 2022 study published in JMIR MHealth and UHealth, wearables refer to devices that are worn by individuals. In health care field, they assist with individual monitoring and diagnosis. Wearables are “seamlessly embedded portable computers...worn on the body," notes another 2018 study published in Telematics Informatics.
A 2018 study published in the journal Sensors noted that wearable health devices are increasingly helping people to better monitor their health status both at an activity/fitness level for self health tracking and at a medical level providing more data to clinicians with a potential for earlier diagnostic and guidance of treatment.
WHO Montreal Meeting: What Are Some Examples Of Wearables?
Blood Pressure Monitor
This is a blood pressure monitor that consists of a cuff that is placed in upper arm with a digital display that provides real time reading of systolic and diastolic blood pressure.
Glucose Monitoring Device
This device estimates your glucose levels in every few minutes. It can be worn in upper arm, with a phone sensor connected to measure readings. It also includes real time glucose alarms to make informed decisions.
Wearable ECG Monitor
ECG patches are interconnected with smartphones, where one can see their readings. They not only measure electrocardiograms, but also detect any abnormalities.
Fitness Tracker
Smartwatches or fitbits that could be worn on your wrist. They help track real time data of your health, steps, heart rate, calorie consumptions, and even sleep patterns. It can also help keep track of oxygen levels.
Integrated Activewear
These activewears come with microscopic sensors to safeguard wearer's body or assist them in reaching their fitness objective.
© 2024 Bennett, Coleman & Company Limited

