- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Medical Memoir: How Chikungunya, A Tanzinian Virus Affected Millions Throughout The World

(Credit-Culture Collections/Canva)
'Medical Memoir' is a Health & Me series that delves into some of the most intriguing medical histories and unveils how medical innovations have evolved over time. Here, we trace the early stages of all things health, whether a vaccine, a treatment, a pill, or a cure.
With 7000 cases of chikungunya diagnosed in China, strict measures have been taken to ensure the outbreak doesn’t spread. The health officials have employed ‘COVID’ style restrictions to ensure the disease remains contained, with elephant mosquito who prey on Aedes mosquitoes, drones that identify mosquito breeding sites as well as people wearing masks are fogging parks and streets with insecticides.
Chikungunya is a viral disease spread by mosquitoes that causes fever, a rash, and severe joint pain. The name comes from a word that means “disease that bends up the joints,” describing the painful, stooped posture of those infected. The virus, known as CHIKV, is transmitted by Aedes mosquitoes and can cause severe complications, though it is rarely fatal.
However, this is not the first time history has witnessed Chikungunya, in fact the timeline of its identification stretches as far as the 1950s.
Origins of Chikungunya
According to the World Health Organization, chikungunya is a viral disease spread by mosquitoes. Its name comes from a language in Tanzania and means "that which bends up the joints," referring to the severe joint pain that can cause people to stoop over. The virus, called CHIKV, is related to the O'nyong nyong virus and was first identified in Tanzania in 1952. While typically not fatal, it can cause severe fever, rash, and long-lasting joint pain, with some cases leading to heart, liver, or neurological problems.
How Chikungunya Spreads and Transfers?
The primary way chikungunya is transmitted is through the bite of infected female Aedes mosquitoes, particularly the Aedes aegypti and Aedes albopictus species. These are the same mosquitoes that spread other diseases like dengue. In Africa, the virus is believed to be maintained in a cycle involving wild primates and various forest-dwelling Aedes mosquitoes. However, in urban areas, especially in Asia and elsewhere, the virus is spread mainly by mosquitoes living in cities.
The Journal of Infectious Diseases explains that over time, different genetic types (genotypes) of the chikungunya virus have emerged, including the Asian, West African, and East/Central/South African (ECSA) genotypes. A new variant, the Indian Ocean Lineage (IOL), appeared in 2004 and caused severe epidemics, mainly in Asia. A key mutation in this new variant, known as E1-A226V, made the virus much more effective at being transmitted by the widespread Aedes albopictus mosquito. This enhanced transmission is a major reason why the virus has spread so quickly to new regions, including parts of Europe and the Americas, which have also seen outbreaks in recent years.
Historical Timeline of Global Chikungunya Outbreak
For centuries, the virus was mainly found in parts of Africa. It was first officially identified in Tanzania in the 1950s. Over the next few decades, it also appeared in Asia, often causing outbreaks that were sometimes confused with dengue fever.
Before 2004
The disease's global spread took a dramatic turn in 2004 when a new and more infectious strain of the virus appeared in Kenya. This strain had a special mutation that made it much better at being transmitted by the Aedes albopictus mosquito. Because this mosquito species is so widespread, this new strain was able to travel and cause huge epidemics in new places.
2004 and Beyond
The new strain quickly spread to islands in the Indian Ocean, then to India and Southeast Asia. In 2007, it reached Europe, causing an outbreak in Italy. By 2013, the virus had made its way to the Americas, starting in the Caribbean and then rapidly spreading throughout North, Central, and South America. This was a major event because the people in the Americas had no prior immunity to the virus, making them very vulnerable to infection.
Today, chikungunya has been reported in more than 110 countries. The combination of a highly infectious virus strain and the widespread presence of mosquito carriers has made it a significant public health problem around the world. Scientists continue to monitor the virus's spread and look for ways to control its mosquito vectors to reduce the burden of this painful disease.
The virus has since caused outbreaks in Europe, starting with a case in Italy in 2007, and in the Americas, with the first local cases reported in the Caribbean in 2013. The lack of immunity in these new populations and the widespread presence of the mosquito vectors led to rapid transmission. Today, chikungunya is a major public health concern, with outbreaks occurring worldwide.
Despite chikungunya being a global threat, there is currently no specific vaccine or treatment available. Efforts to combat the disease focus on supportive care to manage symptoms and preventive measures to control mosquito populations. The rapid spread of chikungunya, especially in tropical and subtropical regions and increasingly in temperate areas, underscores the critical need for public health officials and researchers to work together to find effective solutions, from better diagnostic tools and vaccines to robust vector control programs.
Breast Cancer Signs That Do Not Feel Like Cancer, Explain Doctors

Credits: iStock
On World Cancer Day 2026, we at Health and Me is focussing on the most common cancer among women in India. Breast Cancer, which accounts for over 216,000 new cases every year, as per the 2022 data. This means, 28.2 per cent of female cancers are attributed to breast cancer. What is more tragic is that one woman is diagnosed with breast cancer every four minutes, and one dies every eight minutes in the country.
While, we all know that finding a lump is the red flag, there are other signs that women often miss that delays their detection. Health experts are increasingly warning that this narrow understanding may be delaying early diagnosis for many patients. New medical insights suggest that several lesser-known changes in breast tissue, skin and nipple appearance may signal cancer but often go unnoticed or get dismissed as harmless hormonal changes.
Read: More Than A Diagnosis: Cancer Survivors Share The Small Wins That Helped Them Heal
Breast Cancer Is Not Just A Lump
Data from a consumer survey commissioned by The Ohio State University Comprehensive Cancer Center shows that 93 percent of adults identify a lump as a symptom of breast cancer. But fewer than half are aware of several other warning signs that could appear much earlier.

Experts warn that this knowledge gap can be risky because not all breast cancers form lumps that are easily felt. Breast medical oncologist Ashley Pariser explains that screening mammography remains the most effective tool for detecting breast cancer at its earliest and most treatable stages. She adds that being familiar with the normal look and feel of one’s breast tissue helps people detect subtle changes faster and seek timely medical care.
Pariser notes that many breast changes can occur due to aging or childbirth. Still, she stresses that breast cancer can present in multiple ways, making it important for individuals to report unusual symptoms without delay.
Signs That Should Not Be Ignored
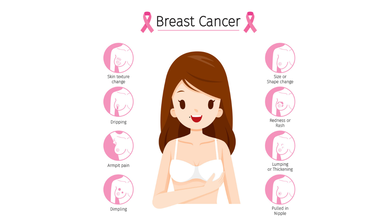
According to Dr Kanchan Kaur, Oncoplastic Breast Surgery Specialist, structural changes in the breast are among the most overlooked early warning signs. She highlights that while lumps are common indicators, deformations in breast shape such as flattening, indentation or dimpling should not be ignored.
Read: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Dr Kaur also points out that an unusual increase or decrease in breast size, particularly when it affects only one breast, and sudden changes in breast symmetry may signal an underlying issue. She advises that these signs warrant clinical evaluation even if they appear painless or gradual.
Another concerning sign is skin texture change. She explains that a reddish, pitted texture resembling the surface of an orange or a marble-like area under the skin can indicate deeper tissue abnormalities. Any area of the breast that looks or feels noticeably different from surrounding tissue should be assessed by a doctor.
Nipple Changes Can Be Early Red Flags
Both research findings and clinical observations highlight nipple changes as key indicators that are often missed. Survey results from Ohio State University show that only about one-third of respondents recognized nipple inversion or retraction as a symptom of breast cancer.
Dr Kaur notes that nipples can provide early clues about breast disease. Symptoms such as newly inverted nipples, dimpling around the nipple, scaly red rashes, burning or itching, and ulceration should prompt medical attention.
Read: Oncologists Warns Of The Cancer Rising Among Women in India
Clear or bloody nipple discharge that is unrelated to pregnancy or breastfeeding is another warning sign. While discharge can occur due to benign causes, experts recommend prompt evaluation to rule out cancer.
Specialists at Moffitt Cancer Center caution that symptoms such as breast tenderness, swelling or changes in fullness are often mistaken for routine hormonal fluctuations. Because these symptoms frequently overlap with premenstrual changes, many women delay consulting a specialist.
Experts from the center advise that persistent breast pain, swelling or unusual fullness that does not resolve within a few days should be medically evaluated. They emphasize that sudden nipple inversion, discharge or skin texture changes require immediate attention.
World Cancer Day 2026: India’s 10 Most Common Cancers, Explains Doctor
Credits: Canva
Cancer trends in India are changing rapidly, driven by lifestyle patterns, environmental exposure, infections, and limited access to early healthcare in some regions. According to Dr Puneet Gupta, Chairman of Oncology Services at Asian Hospital, understanding early warning signs and adopting preventive habits can significantly improve survival outcomes.
“Cancer patterns in India are the results of multiple factors ranging from lifestyle, environmental exposure, infections and access to timely care,” Dr Gupta explained, adding that early symptoms can appear months or even years before the disease reaches advanced stages.
Breast Cancer: The Most Common Cancer In Women
Dr Gupta noted that breast cancer is frequently seen in women, especially after the age of 40. He highlighted that the disease often develops silently and without pain.
He explained that warning signs may include lumps in the breast or under the arm, changes in breast shape, skin dimpling, inward turning of the nipple, or unusual discharge. “Do not ignore these changes,” he cautioned. Regular self-examination, along with timely imaging tests such as mammography, ultrasound, or MRI, can help detect breast cancer early.
Cervical Cancer: Strongly Linked To HPV Infection
Cervical cancer mainly affects women between 30 and 60 years. Dr Gupta emphasised that HPV infection remains the leading risk factor. Early symptoms can include abnormal vaginal bleeding, bleeding after intercourse, or persistent pelvic pain, although early stages often remain symptom-free.
He stressed that routine Pap smear screening and HPV vaccination play a crucial role in prevention and early diagnosis.
Lung Cancer: Rising Risk Beyond Smoking
While lung cancer remains more common in men, Dr Gupta pointed out that cases among women are rising as well. Smoking is the primary cause, but exposure to fine particulate air pollution (PM2.5) also contributes to the risk.
He warned that persistent cough, chest pain, breathing difficulty, unexplained weight loss, or coughing blood require immediate medical evaluation, particularly in people with a history of tobacco use.
Oral Cancer: A Major Concern In India
Oral cancer remains widespread due to tobacco, gutka, areca nut consumption, and HPV infection. Dr Gupta explained that long-lasting mouth ulcers, red or white patches inside the mouth, jaw stiffness, or swallowing difficulty are early red flags. Regular dental and oral examinations can help detect early cancerous changes.
Colorectal Cancer: Lifestyle-Linked Risks
According to Dr Gupta, colorectal cancer is increasingly being diagnosed in adults around 40 years of age. Sedentary lifestyles, low-fiber diets, and excessive red meat intake are major contributing factors.
He said symptoms such as blood in stool, persistent bowel habit changes, abdominal pain, or unexplained anaemia should not be overlooked. Early screening and genetic testing in high-risk individuals can significantly improve outcomes.
Stomach Cancer: Often Shows Subtle Symptoms
Dr Gupta explained that stomach cancer may initially present as indigestion, early fullness, nausea, or unexplained weight loss. It is often associated with long-term Helicobacter pylori infection, smoking, and salt-heavy diets. Persistent digestive discomfort warrants medical attention.
Prostate Cancer: Common But Often Slow Growing
Prostate cancer typically affects men above 50 and usually progresses gradually. Dr Gupta noted that difficulty urinating and frequent nighttime urination are common early symptoms. Regular check-ups help detect the disease before complications arise.
Esophageal Cancer: Linked To Lifestyle And Nutrition
Tobacco use, alcohol consumption, poor nutrition, and iron deficiency increase the risk of esophageal cancer. Dr Gupta advised that swallowing difficulty, chest discomfort, or unexplained weight loss should prompt evaluation through tests like endoscopy or barium swallow.
Ovarian Cancer: Often Missed Due To Vague Symptoms
Dr Gupta explained that ovarian cancer frequently goes undetected due to non-specific symptoms such as bloating, abdominal discomfort, or early satiety. Women with persistent symptoms, particularly those with a family history of breast or ovarian cancer, should seek medical evaluation.
Liver Cancer: Screening Is Crucial For High-Risk Groups
Liver cancer often develops in individuals with chronic liver disease. Symptoms such as jaundice, abdominal swelling, or persistent pain usually appear late. Dr Gupta stressed that hepatitis vaccination and screening among high-risk groups are vital for prevention.
Lifestyle Changes And Screening Can Reduce Risk
Dr Gupta emphasized that although cancer cannot be completely prevented, a significant proportion of cases are linked to modifiable risk factors. Avoiding tobacco, maintaining a healthy weight, consuming balanced nutrition, managing stress, and staying physically active can lower risk.
He added that vaccinations against HPV and hepatitis further reduce cancer risk, while regular screening helps detect cancers at pre-cancer or early stages. “Education, prevention and early detection make the difference between late-stage disease and long-term survival,” Dr Gupta concluded.
Prenatal Vitamins vs Multivitamins: Experts Reveal What Women Need

Credit: Canva
While you may have seen multiple women, who are not pregnant, taking prenatal vitamins to improve their skin, hair and nail quality, experts say you should steer clear and only stick to multivitamins to ensure your body stays healthy all-year round.
Prenatal vitamins are daily supplements for women who are pregnant or trying to get pregnant. These supplements contain the vitamins and minerals you need to support healthy fetal development, according to the Cleveland Clinic.
Dr Rohan Palshetkar, Consultant IVF Specialist, Bloom IVF tells Healthandme: ""Prenatal vitamin should be taken three months at least prior to the pregnancy or basically whenever you begin to start planning the pregnancy, ensure that all your micro nutrients as well as your folic acid levels are up to the normal mark so as to ensure that your baby has a healthy growth"
But when your body doesn't need it, taking supplements could put you at risk over time.
Which Vitamins And Minerals Are Prenatal Vitamins Rich In?
As per the American College of Obstetricians and Gynecologists (ACOG), here are the most important nutrients prenatal vitamins are packed with:
Folic Acid: One of the most important prenatal nutrients, this B vitamin is important as it creates your baby's neural tube. This is the structure that eventually forms brain. As per the US Preventive Services Task Force, folic acid supplements significantly increase the growth of healthy neural tube. The American Academy of Pediatrics also notes that it helps the neural tube to protect from defects by 50 percent.
Iron: It supplies blood and oxygen to the fetus and also helps build the placenta. It also gives the mother extra blood volume that you need throughout pregnancy. Pregnant people are prone to anemia, this is why iron supplementation is a must.
Calcium: The most time spend in uterus for a baby is invested in building their bones and teeth, this is a Herculean task, and requires the mother to have plenty of calcium. If you don't have enough calcium, then your baby will utilise the calcium from your body, which could lead to temporary bone loss.
Certain prenatal supplements also contain other additives such as omega-3 fatty acids.
Why Is It Dangerous To Take Prenatal Vitamins
The main difference between a prenatal vitamin and a multivitamin is the concentration of folic acid and iron.
Ingesting enough folate from food or folic acid from supplements at the start of a pregnancy lowers the risk of certain birth defects. Along with this, iron supplements help the body make the extra blood cells needed during pregnancy.
The amount of folic acid suggested for people who are planning a pregnancy is 400 to 800 micrograms (mcg) a day. The amount of iron needed in pregnancy is 27 milligrams (mg) a day.
The typical amount of folic acid for an non-pregnant adult is 400 mcg a day. For iron, the typical daily amount is 8 mg for males and 18 mg for females.
Taking iron and folic acid at levels higher than the suggested amounts may bump people closer to the upper limit for these nutrients which can raise the risk of health problems.
Taking too much folic acid, especially over 1,000 mcg daily without a doctor's advice, can mask a vitamin B12 deficiency, potentially causing irreversible nerve damage and may lead to side effects such as bitter taste, nausea or sleep problems, with potential links to increased risks in pregnancy like autism or insulin resistance.
Eating too much iron, especially from supplements, can cause acute iron poisoning, leading to severe nausea, vomiting, abdominal pain, diarrhea and bloody stools. Long-term excessive intake causes iron to deposit in tissues, causing iron overload (hemochromatosis) that damages the liver (cirrhosis), heart (failure), and pancreas (diabetes) and may cause a bronze skin color.
© 2024 Bennett, Coleman & Company Limited

