- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Meet Louise Brown- The World’s First IVF Baby
Meet Louise Brown- The World’s First IVF Baby And The Innovators Who Changed The Face Of Infertility Treatment Forever
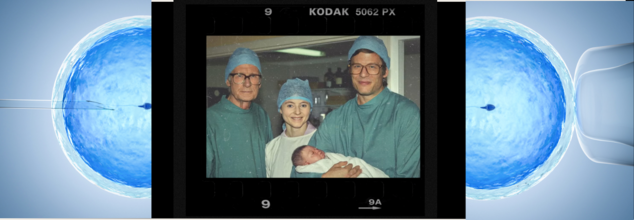
Almost half a century ago, a maverick event marked the course of medical history into a new and revolutionary phase. The birth of Louise Brown on 25th July 1978 marked the world's first baby born through a process of In-Vitro Fertilization or IVF. With Louise Brown, hope for millions of infertile couples dawned across the globe and massive debates followed regarding the ethics of assisted reproduction.
The new drama for Netflix is titled Joy after Louise's middle name, takes viewers back to the great journey of pioneers for this groundbreaking achievement. Louise, 46 now and working at a bakery in Bristol, has heard more than her share of thanks from strangers. She's quick to say, however, that it is her parents and the triumvirate of British visionaries-physician Robert Edwards, embryology nurse Jean Purdy, and gynecologic surgeon Patrick Steptoe-who faced incredible obstacles to make her existence possible.
“I still get people come up to me saying, ‘Oh, you’re amazing.’ And I’m like, ‘I didn’t do anything, it was Mum and Dad and the three doctors.’ It’s lovely people who want to thank them,” told The US Sun.
Netflix drama Joy looks at the sacrifices made by the team to create IVF. Dr. Robert Edwards started his research into fertilization in 1955, but in 1968, he was the first to fertilize a human egg. However, the success did not attract encouraging support from the medical fraternity, and Edwards did not get any funds for continued research. He, along with nurse Jean Purdy and surgeon Patrick Steptoe, planned a clinic in an abandoned ward of Royal Oldham Hospital.
The couple had personal and professional challenges. Edwards was away from his family and children for 170 miles, Purdy had conflict with her religious mother, and Steptoe was putting off his retirement dreams. Public opposition further tested their strength, and opponents referred to their work as unnatural and even vandalized their clinic with the word "Frankenbabies."
Their diligence paid off after years of trial and error. A breakthrough came when Edwards decided to use a naturally produced egg instead of stimulating the ovaries through hormones. This new approach proved successful with Louise's mother, Lesley, who had been trying to conceive for a decade.
A Miracle Amidst Controversy
Lesley Brown and her husband, John, decided they would like a child even though the odds were completely stacked against them. Diagnosed with blocked fallopian tubes, Lesley was told that her chances of conceiving were one in a million. Lesley approached Steptoe for assistance after a gynecological operation she was obliged to pay for herself, thanks to a win on her football pools. The Browns were entered in the experimental IVF procedure.
Lesley’s faith in the team was unwavering. Louise recounted, “If they had said, ‘Go into Trafalgar Square and stand on your head naked and you’ll get pregnant,’ she would have”, as reported in The US Sun.
The process worked on the 101st attempt. A single egg fertilized in a petri dish with John's sperm was successfully implanted in Lesley's womb. Nine months later, Louise was delivered via Caesarean section, with the world's media waiting outside the hospital.
Although successful, the aftermath of birth for Louise was far from smooth. Her family received death threats and vile messages - once even a smashed test tube through the post with a foetus-like object inside - and Louise herself was subjected to over 100 tests as a newborn to dispel doubts about her health.
While her birth was a scientific success, it was also an intensely personal one. "When I had my sons, I realized how good those people were,"* Louise said, speaking of the sacrifices of her parents and the scientists."
The film Joy honors the work of the trio, especially Jean Purdy, who died at 39 years of age in 1985. Although she played a critical role, the historical accounts of her work were often overlooked. Her name wasn't put on the plaque celebrating the team's triumph until 2022.
It was Dr Robert Edwards, who continued to keep in touch with Louise even up to his death in 2013, who was rewarded with the Nobel Prize in 2010 for his work on IVF. Jean and Patrick were both deceased by then.
Louise summarizes, "They have done it for 12 million of us. I owe them my life. I'd do anything for any of them, my parents, and the three scientists.
Today, over 12 million babies worldwide have been born through IVF-a testament to the vision and perseverance of Edwards, Purdy, and Steptoe. Louise Brown's story, now immortalized in Joy, is as much a story of medical innovation as it is about human resilience and the power of hope.
The Long-Term Effects of IVF on Modern Health Care
Birth of Louise Brown was more than a medical milestone; it led to revolution in reproductive healthcare. Successive decades have changed millions of lives through IVF technology with hope for individuals and couples wanting a child. Beyond the origins, the field of ART has evolved into a wide research sector that pushes beyond the frontiers of science and redefines possible interventions in human reproduction.
Success in IVF has led to research on related techniques, such as intracytoplasmic sperm injection (ICSI), vitrified eggs, and preimplantation genetic testing. These all granted the power of reproductive control, allowing even in defiance of age, genetic conditions, or cancer treatments, to plan a family.
The principles developed by the original IVF team have paved the way for better understanding of reproductive biology, innovation in treating problems like polycystic ovary syndrome (PCOS), and endometriosis. The existence of IVF has raised awareness about infertility and helped reduce the stigma around seeking medical help.
Still, with every medical discovery, IVF has its unique share of hurdles. Many issues concerned with accessibility and affordability ensue and take center stage in the ART discourse, and along with the potential to transform lives, IVF is still expensive for many people, a challenge for global health organizations to equitably access.
Health care providers emphasize the value of education and support provided to patients at every step of the IVF process. IVF often requires multiple attempts and is often physically, emotionally, and financially stressful. Support for psychological well-being has increasingly been an essential element of treatment through counseling and stress management in IVF clinics.
Claire Danes Revealed She Was Shocked At Being Pregnant After 40, Does Age Really Play A Role?

(Credit-Claire Dane/Instagram, Canva)
Claire Danes recently revealed that she was shocked to learn that she was pregnant with her third child at 44. In an interview with Amy Poehler in an episode of Good Hang with Amy Poehler, the Beast In Me actress revealed that she burst into tears at her OB/GYN’s office, explaining that she didn’t know it was possible to be pregnant after 40.
Danes shared that she initially felt a strange sense of embarrassment about the pregnancy. Because she and her husband, Hugh Dancy, weren’t planning for a third, Danes felt like she had stepped outside of normal "parameters."
The debate surrounding pregnancies after 40 has always persisted. Many people like Claire believe that it is impossible to get pregnant after your biological clock runs out. However, in reality, things do not work like that. Dr Rohan Palshetkar, Consultant IVF specialist, at Bloom IVF explains a few factors one should know about.
Can You Get Pregnant After 40?
Yes, Dr Rohan explains that it is completely possible and safe with the current technological advancements. “Earlier we did have fetal medicine specialists, high resolution ultrasounds, better monitoring techniques and safter IVF options”
Screening tests are much more detailed, IVF options are more robust and egg freezing is also an empowering tool for women who wish to have pregnancies later in life, Dr Rohan explained.
However, he also pointed out that post 35 risks of having diabetes and hypertension increases, so consistent monitoring helps a lot.
What Are Some Risks Of Pregnancies After 40?
The chance of having a high-risk pregnancy increases for women above 40, according to the American College of Obstetricians & Gynecologists (ACOG). They explain that since women are born with all the eggs they will ever have, those eggs age right along with the body. As time goes on, the number of eggs decreases, and their quality can change.
While many women have healthy pregnancies in their 40s, here are some specific risks you should know about.
Chromosome Issues
Older eggs are more likely to have certain genetic changes. This means there is a higher chance for the baby to be born with a health condition like Down syndrome instead.
Miscarriage or Stillbirth
Women in their forties face a much higher statistical chance of losing a pregnancy. It is very important to stay in close contact with your doctor to monitor your baby's health.
Low Birth Weight
There is a greater risk that the baby will be born weighing less than what is considered healthy. Small babies often need extra medical care and stay in the hospital longer.
Blood Clots
Being pregnant naturally increases your risk of developing dangerous blood clots. However, this specific medical danger becomes even more likely for mothers who are over the age of thirty-five or forty.
Gestational Diabetes
This is a specific type of high blood sugar that some women develop only while they are pregnant. It requires careful diet management or medication to keep you and baby safe.
Preeclampsia
This is a very serious condition involving high blood pressure that can happen during pregnancy. It can be dangerous for the mother and the baby if it is not treated quickly.
Labor Challenges
Delivery can be more difficult for older mothers, often leading to longer labor times. Because of these complications, doctors are much more likely to recommend a surgical C-section birth instead.
How Doctors Support Pregnancies After 40
Being "high-risk" doesn’t mean something will go wrong; it just means your medical team will watch you more closely. Modern medicine has great tools to keep you and your baby safe, such as,
- Prenatal Screening
- Extra Ultrasounds
- Frequent Check-ups
11 Signs From Your Nervous System You Should Never Ignore, According to Neurologists

Credits: iStock
Neurology can sometimes be overwhelming because the nervous system touches almost every part of the body. This means, from memory to speech, to sleep and every sensation, all of them are part of neurology. So, naturally, neurologists deal with a vast range of conditions, including carotid artery disease, seizure disorders, Alzheimer’s and frontotemporal dementia, migraines and facial pain, Parkinson’s disease, muscle disorders, narcolepsy, and many others.
“If there’s a nerve somewhere, a neurologist could get involved,” says Dr. Andrew Dorsch, division chief for general neurology at Rush University System for Health and a specialist in neurologic rehabilitation, as reported by Times. “And there’s nerves everywhere in the body. There’s a lot that can go wrong, and figuring it out often takes real detective work.”
The problem is that many people ignore early neurological symptoms, because it looks like any other normal thing that could happen to anyone under immense stress. Here are 11 symptoms doctors say you should never ignore.
Double vision that comes on suddenly
One overlooked symptom is a specific type of double vision that happens when both eyes are open and improves when either eye is closed. This is known as neurological diplopia and is different from eye-related vision problems.
Dr. Luis Cruz-Saavedra, a neurologist with Memorial Hermann Health System, told Times, this type of double vision can be linked to serious conditions such as multiple sclerosis, stroke, aneurysm, myasthenia gravis, brain tumors, or brain infections.
If double vision starts suddenly, it is an emergency. “Immediately,” he says. Doctors may check for stroke warning signs and order imaging such as a CT scan or MRI to identify the cause.
Weakness in one arm or leg
Subtle weakness is another symptom people tend to ignore. Dragging one foot, limping, dropping objects, or struggling to write with a dominant hand are all red flags.
“I see people come in months after symptoms begin,” Cruz-Saavedra says. Many assume it is a pinched nerve, but weakness can signal stroke, brain tumors, multiple sclerosis, or brain inflammation. Neurologists usually test strength, reflexes, balance, and coordination to narrow down the cause.
Brief episodes of unresponsiveness
Some people suddenly stare blankly for a few seconds and then return to normal with no memory of the episode. These moments are often noticed by family members rather than the patient.
Cruz-Saavedra explains that this can be a sign of temporal lobe seizures, which affect areas of the brain involved in memory and emotion. People may describe it as losing a small chunk of time, which should always be medically evaluated.
Trouble speaking or understanding words
Speech problems are among the most common warning signs of stroke, yet many people delay seeking care.
Dr. Enrique Leira, director of the division of cerebrovascular diseases at the University of Iowa, toles Times, stroke symptoms often appear suddenly. Speech may become slurred, slow, or difficult to understand. Some people struggle to find words or comprehend language altogether. In these cases, urgent medical attention is critical.
Sudden, severe headache during exertion
Most headaches are harmless, but some require immediate attention. A headache that strikes suddenly, feels unusually intense, and occurs during physical effort can indicate something serious, including stroke.
Leira says headaches that do not gradually build up and instead arrive abruptly should always be checked right away.
Persistent numbness in feet or fingers
Dr. Dorsch says numbness commonly affects the feet or fingers and suggests that nerves are failing to send signals properly. This is different from tingling, which usually means nerve irritation.
Numbness may result from diabetes, autoimmune conditions, genetic disorders, or nerve damage. A full neurological workup helps determine which nerves are affected and why.
Frequent déjà vu
Occasional déjà vu is normal. Experiencing it repeatedly is not.
“If it’s happening regularly, that’s not typical,” Dorsch says. Frequent déjà vu episodes can be an early sign of temporal lobe seizures and should be evaluated.
Difficulty standing up from a chair
Struggling to rise from a chair on a regular basis is not just about aging or stiff joints. Dorsch says neurologists want to rule out problems involving muscles, nerves, or the spinal cord, including Parkinson’s disease or amyotrophic lateral sclerosis.
Changes in voice
Neurologists pay close attention to voice changes. Dr. Alexandru Olaru of University of Maryland St. Joseph Medical Center notes that an unusually soft or breathy voice may indicate Parkinson’s disease. Slurred speech can point to stroke.
Another concerning sign is a wet or gurgly voice caused by saliva pooling in the throat. This can occur in conditions like Parkinson’s disease, ALS, and multiple sclerosis.
Muscle twitches that do not stop
Muscle twitches are common and often harmless. But when they occur repeatedly in the same location, they should be discussed with a doctor.
Olaru explains that these fasciculations may be benign or linked to conditions such as spinal stenosis, ALS, or autoimmune nerve disorders. Tests like electromyography can help identify the cause.
Sudden personality or behavior changes
Abrupt shifts in behavior, including paranoia, withdrawal, impulsivity, or inappropriate behavior, can signal neurological disease.
Cruz-Saavedra says conditions like autoimmune encephalitis or frontotemporal dementia may show up as personality changes long before memory problems appear. New obsessive behaviors or hoarding can also be warning signs.
Drinking Alcohol Could Damage Your DNA, Not Just Your Liver Or Heart
Credits: AI Generated
Alcohol is often seen as harmful mainly for the liver or heart, but its impact goes much deeper—reaching down to our DNA. Even moderate drinking can silently cause changes at a cellular level, raising long-term health risks that may not be immediately visible. According to Dr. Amit Miglani, Director & HOD – Gastroenterology, Asian Hospital, the breakdown of alcohol in the body produces a toxic chemical called acetaldehyde, which can directly damage DNA inside our cells.
Alcohol Can Damage Your DNA, Not Just Your Liver And Heart
This damage disrupts the body’s natural repair mechanisms, allowing mutations to accumulate over time. Such mutations are linked to several cancers, including cancers of the mouth, throat, liver, breast, and colon. The insidious nature of this damage means that even when you feel healthy, harmful changes may be occurring beneath the surface.
How Alcohol Interferes With DNA Repair
DNA damage can be complex to understand, but its consequences are serious, explains Dr. Arun Kumar Giri, Director – Surgical Oncology, Aakash Healthcare. Normally, the body constantly repairs minor DNA errors. However, alcohol disrupts this repair process, leaving cells vulnerable to mutation and abnormal growth.
Dr. Giri adds that some people have genetic variations that make them break down alcohol more slowly. For these individuals, alcohol stays in the body longer, increasing the likelihood of DNA damage. Over years of repeated exposure, this can lead to uncontrolled cell growth and eventually cancer.
No Completely Safe Level of Alcohol For DNA Health
One of the most important points, Dr. Giri emphasizes, is that there is no entirely safe level of alcohol when it comes to DNA. The risk increases with both the frequency and quantity of drinking. Even occasional binge drinking can be harmful, meaning that how often you drink can be as important—or even more so—than how much you drink at one time.
This perspective shifts the discussion from asking “How much alcohol is too much?” to “How often am I exposing my cells to alcohol-induced damage?” Protecting DNA health requires regular monitoring and mindful drinking habits, even for those who feel healthy today.
Alcohol: Long-Term Health Implications
Alcohol-induced DNA damage is not just a short-term concern. Over time, the accumulation of mutations can significantly increase cancer risk and other serious diseases. Regular health check-ups, a balanced lifestyle, and moderation, or complete avoidance of alcohol are crucial steps for safeguarding your genetic health and overall well-being.
Dr. Amit Miglani highlights that “It’s not just about the organs you can feel being affected today; it’s about protecting your long-term health, especially your DNA, for the future.”
Dr. Arun Kumar Giri advises, “Understanding the cellular impact of alcohol helps people make informed choices about their drinking habits. Even small changes can significantly reduce the risk of long-term damage.”
© 2024 Bennett, Coleman & Company Limited

