- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
That Thumping Pulsing In Your Ear Isn’t Just Annoying – Here’s What It Means

Image Credits: Canva
You also have certainly experienced what ear disturbances feel like when you leave a really loud concert: temporary and seemingly meaningless. But what if the noise isn't a maddening ringing, and more like steady thumping in synchronization with your heartbeat? This condition is called Pulsatile Tinnitus and is characterized by a rhythmic whooshing, thudding, or pulsing in one or both ears. Though at times frustrating, and even sometimes worrisome, it most often has a known cause, and is in fact, an early indicator of a significant disease process.
Depending on the presence of a vascular abnormality - such as an aneurysm or arteriovenous malformation-surgery or endovascular treatments may be necessary.
Pulsatile tinnitus can be temporary and harmless, but in some cases, it may be a warning sign of a serious condition. If the rhythmic pulsing in your ear persists, seek medical evaluation to rule out any underlying health issues. Identifying the root cause is the first step toward finding relief and protecting your long-term health.
What Is Pulsatile Tinnitus?
Pulsatile tinnitus is a rare form of tinnitus that occurs due to blood flow irregularities in the vessels near the ears. Unlike traditional tinnitus, which is often described as a constant ringing, buzzing, or hissing, pulsatile tinnitus is rhythmic and synchronized with your heartbeat.
Most people experience it in just one ear, but it can occur in both. While it's usually harmless, persistent pulsatile tinnitus should not be ignored as it may signal an underlying cardiovascular or neurological issue that requires medical attention.
Why Do You Hear Your Heartbeat in Your Ear?
Hearing your heartbeat in your ear can be unsettling. While occasional pulsatile tinnitus is generally harmless, frequent or persistent cases warrant a closer look. The sound results from turbulent blood flow in the vessels around the ear, which can be caused by various conditions, including high blood pressure, anemia, or even pregnancy. Some individuals may experience it only when lying down or in specific positions.
Common Symptoms of Pulsatile Tinnitus
While symptoms differ from individual to individual, the most common symptom of pulsatile tinnitus is the presence of a rhythmic sound in one or both ears that occurs in synchronization with the heartbeat. These sounds can be described as follows:
- Whooshing
- Grinding
- Hissing
- Thudding
- Whistling
The intensity of the sound may vary with physical activity, stress, or change in body position.
What Triggers Pulsatile Tinnitus?
1. An Intense Workout
Vigorous exercise increases blood flow and cardiac output, causing temporary pulsatile tinnitus. The extra blood circulating through your arteries near the ears can create a pounding sensation, which usually subsides after you cool down.
2. Anemia
When you have low red blood cell levels, your heart must pump harder to supply oxygen to your body, creating turbulent blood flow near the ear. This increased circulation can lead to pulsatile tinnitus.
3. Thyroid Disorders
Thyroid conditions, particularly hyperthyroidism, can alter blood composition and pressure, leading to fluctuations in venous return to the heart and causing pulsatile tinnitus.
4. Fluid in the Ear or an Ear Infection
When fluid builds up in the middle ear, either due to an infection or other causes, blood vessels around the ear may pulsate the trapped fluid. This can result in hearing a heartbeat-like thumping sound.
5. High Blood Pressure
High blood pressure (hypertension) forces blood to flow more aggressively through your arteries, increasing turbulence and leading to pulsatile tinnitus. If your systolic pressure is 120 or higher and/or your diastolic is above 80, your risk increases.
6. Atherosclerosis
A buildup of plaque in the arteries (atherosclerosis) can narrow blood vessels, reducing blood flow and causing pulsations that may be heard in the ear. This is more common in older adults.
7. Pregnancy
Pregnant individuals experience increased blood volume and pressure, which can affect major blood vessels near the inner ear, causing pulsatile tinnitus. Fluid retention during pregnancy may also amplify pulsations.
8. Other Underlying Conditions
While vascular issues are common causes, other conditions can also trigger pulsatile tinnitus, including:
- Head trauma
- Paget’s disease (a chronic bone disorder)
- Hyperthyroidism (overactive thyroid)
When Should You See a Doctor?
While occasional pulsatile tinnitus isn’t necessarily a cause for alarm, persistent or worsening symptoms should be evaluated by a healthcare professional. It may indicate a serious vascular, neurological, or cardiovascular issue that requires treatment.
Signs You Need Immediate Medical Attention:
- Prolonged tinnitus that lasts for more than a few weeks
- Sudden increase in loudness or pitch
- Associated symptoms such as headache, dizziness, or blurred vision
- Pulsatile tinnitus after head trauma
How Is Pulsatile Tinnitus Diagnosed?
A medical professional—preferably a neurotologist or otolaryngologist (ENT specialist)—can assess pulsatile tinnitus through:
- A physical exam to check for vascular abnormalities
- Hearing tests (audiometry) to evaluate sound perception
- Imaging scans (MRI, CT, or ultrasound) to detect blockages, tumors, or aneurysms
- Blood tests to detect anemia, thyroid disease, or cholesterol level
Treatment of Pulsatile Tinnitus
Treatment depends on the underlying cause. Some of the common methods include:
- Treatment of Hypertension
- Lifestyle modifications like reducing salt intake, managing stress, and exercising regularly can be helpful if hypertension is the causative agent.
- Medications are also given in some cases.
Treatment of Anemia or Thyroid Conditions
- Iron supplements are prescribed for anemia, while thyroid conditions require medication or hormone therapy.
- Treating Ear Infections or Fluid Buildup
- Doctors may prescribe antibiotics, antihistamines, or decongestants to clear fluid accumulation.
- Surgical or Interventional Procedures
One Blood Type Linked To Higher Rates Of Fatal Liver Illness, Study Finds
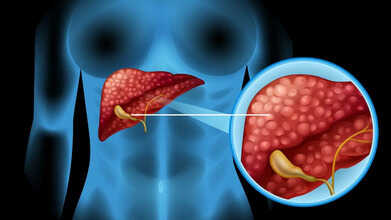
Credits: Canva
A recent study suggests that a person’s blood group could play a role in whether they are more likely to develop severe liver conditions. Although most of us link blood type only with transfusions or donor matching, scientists now believe it may also offer clues about long-term liver health.
Higher Liver Disease Risk Linked to This Blood Group
A new study published in the journal Frontiers reports that individuals with blood group A have an increased chance of autoimmune liver disorders. In these conditions, the body’s own immune system mistakenly harms liver tissue, which can lead to ongoing damage and, in some cases, life-threatening liver failure.
The researchers also found that people with blood group B may have a slightly lower likelihood of certain liver-related concerns compared with those who have type A.
Why Your Blood Group Could Influence Liver Health?
Scientists have long examined how inherited blood groups relate to different illnesses. Some earlier findings noted that individuals with non-O blood types (A, B, or AB) tend to show higher activity of certain clotting factors and other changes in the body.
These differences may affect blood flow in the liver. For example, past studies found slightly increased levels of a clotting protein called von Willebrand factor in people with advanced liver disease who had non-O blood types, although it does not appear to be a major driver of risk.
Liver Conditions Connected to Certain Blood Groups
The latest research focused on autoimmune liver diseases such as:
- Autoimmune hepatitis, in which the immune system attacks liver cells.
- Primary biliary cholangitis (PBC), where the bile ducts inside the liver slowly break down.
Among these, autoimmune hepatitis showed a stronger link with blood group A. Blood group B appeared to carry a somewhat lower chance of PBC when compared with type A.
What Past Research Shows About Liver Cancer
Several earlier studies explored the relationship between blood group and liver cancer (hepatocellular carcinoma or HCC). Older data and a large meta-analysis found that people with type O blood were under-represented among those with liver cancer, suggesting that type O may be tied to a lower risk overall.
Why Knowing Your Blood Type Helps
Understanding your blood group can offer insight into potential health risks, though it does not mean you will certainly develop liver disease if you are type A or B. It remains only one part of a larger picture.
This may be especially important if you have blood type A or B and a family history of liver conditions. Routine health checks, liver screenings, and discussions with your doctor can help you watch for any early signs.
For now, it is clear that blood type is more than a simple classification, as it may hold useful information about future liver health.
Autoimmune liver disorders are uncommon, yet they can become serious when they are not spotted in time. A better grasp of the genetic and immune-related factors behind them can guide stronger prevention and treatment efforts. The authors of the study note that more research involving larger and more varied groups of people is needed to confirm these findings and to explain how different ABO blood types may influence the development of autoimmune liver problems.
Metformin, A Common Diabetes Medicine, Shows Surprising Brain Effects

Credits: Canva
According to the International Diabetes Federation, roughly one in nine adults worldwide lives with diabetes, and around 90% of these cases are type 2 diabetes. There is currently no cure for type 2 diabetes. Still, the condition can be managed through healthy lifestyle habits, such as staying active, as well as medication. One widely used medication is metformin, considered a first-line therapy for type 2 diabetes, and it has been prescribed for decades since the Food and Drug Administration (FDA) approved it in 1994. Recent research, however, suggests it may also act directly on the brain, opening the door to new approaches to treatment.
Metformin Found to Unexpectedly Affect The Brain
Scientists at Baylor College of Medicine in the US have discovered a brain pathway that metformin appears to influence, alongside its known effects on other parts of the body. "It has been widely believed that metformin lowers blood sugar mainly by reducing glucose production in the liver. Other studies have also highlighted its action in the gut," says Makoto Fukuda, a pathophysiologist at Baylor.
As reported by Science Alert, the researchers explained, "We turned our attention to the brain, given its central role in regulating overall glucose metabolism. Our goal was to understand whether and how the brain contributes to metformin’s anti-diabetic effects."
How Is Metformin Affecting Your Brain?
Earlier research by some of the same scientists had pinpointed a protein in the brain called Rap1, which influences glucose metabolism, especially in a region called the ventromedial hypothalamus (VMH).
In their 2025 study, experiments on mice showed that metformin reaches the VMH, where it helps combat type 2 diabetes by essentially shutting down Rap1. When mice were genetically modified to lack Rap1, metformin no longer affected a diabetes-like condition—even though other medications still worked. This provides strong evidence that metformin acts in the brain through a mechanism distinct from other drugs.
The researchers also examined which specific neurons metformin interacts with. This could eventually pave the way for treatments that target these neurons directly. "We found that SF1 neurons are activated when metformin enters the brain, indicating they are directly involved in the drug’s effect," they said.
Metformin Side Effects
While generally safer than many other type 2 diabetes medications, metformin does have side effects. Gastrointestinal issues such as nausea, diarrhea, and stomach discomfort affect up to 75% of users. Other risks can arise when there are underlying conditions like kidney problems, which may compound health concerns.
Metformin is also recognized as a gerotherapeutic—a medication that may slow aging processes in the body. For instance, it has been shown to reduce DNA damage and support gene activity linked to longer life.
Previous studies indicate that metformin can also protect the brain from wear and tear and may even lower the risk of long COVID, according to Science Direct.
Can Ethiopia’s Volcanic Ash Make Delhi’s Toxic Air Worse For People With Respiratory Issues?
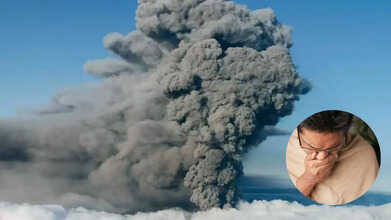
Credits: ANI
Delhi NCR is already facing one of its toughest air-quality crises, and now another worry has emerged. Volcanic ash from Ethiopia’s Hayli Gubbi volcano has started drifting toward Indian skies. BBC reports that ash clouds from this rare eruption have reached Delhi, raising concerns about health risks in a city where clean air is already hard to come by due to rising pollution. As this volcanic ash moves closer, people fear it could worsen existing respiratory problems.
In Delhi, where the Air Quality Index (AQI) often falls in the “very poor” or “severe” range, even small increases in particulate matter can have serious health effects. Understanding what volcanic ash can do and taking the right precautions can help reduce its impact.
Ethiopian Volcanic Ash Reaches Delhi
A volcano in northern Ethiopia erupted on Sunday for the first time in nearly 12,000 years. Winds blowing at 100–120 km/h carried ash plumes to several countries. The Hayli Gubbi volcano in Ethiopia’s Afar region erupted Sunday morning, and by late last night, ash clouds reached Delhi, which is already struggling with toxic air, causing some disruption to flights.
The ash plumes, rising thousands of feet into the atmosphere, first passed over Gujarat and then moved toward Rajasthan, Delhi, Haryana, and Punjab. According to the India Meteorological Department (IMD), the ash clouds are drifting toward China and are expected to clear from Indian skies by 7:30 pm.
The Health Impact Of Volcanic Ash: What Science Says
Volcanic smog, also called “vog,” is generated whenever a volcano erupts. Global health bodies like the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC) have long studied its effects. Here’s what you need to know about how volcanic ash can impact health.
Respiratory Risks: Who’s Most Vulnerable
Volcanic ash is made of fine particles that can reach deep into the lungs. According to the US Geological Survey’s Impacts & Mitigation guidelines, inhaling these particles can lead to:
- Irritation of the nose, throat, and upper airways
- Dry cough, sore throat, or chest discomfort
- Bronchitis-like symptoms or wheezing in people with asthma or chronic bronchitis
Even healthy individuals may experience shortness of breath or discomfort after heavy exposure. For those with pre-existing lung conditions, the effects can be much more serious.
Ethiopia’s Volcanic Ash: What Is Delhi’s Situation?
IMD Director General M. Mohapatra stated that the plume is approaching Delhi NCR, but “any significant impact on ground-level pollution is unlikely” because most of the ash is high in the atmosphere. He added that the ash cloud may appear as a cloudy, hazy sky for a few hours as it moves eastwards.
Meteorologists and weather analysts have noted that the plume contains volcanic ash, sulphur dioxide, and tiny glass or rock particles. It is moving quickly, at around 100–200 km/h, according to reports.
Can Ethiopia’s Volcanic Ash Make Delhi Respiratory Issues More Dangerous?
Dr Aditya Nag, Assistant Professor, Department of Respiratory Medicine, NIIMS Medical College and Hospital, told us that even if most of the ash remains high in the sky, fine particles can settle on the ground and mix with Delhi’s already polluted air. Components like ash and sulphur dioxide can irritate the lungs, throat, and eyes.
Dr. Manav Manchanda, Director & Head – Respiratory, Critical Care & Sleep Medicine, Asian Hospital, told us that people most at risk include children, the elderly, and anyone with asthma or COPD. Volcanic ash can also pose environmental risks, such as reducing visibility or damaging engines.
“Abrasive particles in the volcanic ash can trigger bronchospasm in COPD and asthma patients, making their condition worse,” said Dr Aditya Nag.
Precautions To Stay Safe
Dr. Manav Manchanda, advise the same safety measures that apply during high pollution days:
- Wear N95 or N99 masks outdoors: These filter fine ash particles better than regular masks.
- Limit outdoor activities during peak pollution: Avoid exercising in the morning or late evening.
- Keep doors and windows closed: Use an air purifier to reduce indoor air contamination.
- Stay hydrated: Drink warm water or herbal teas to help clear your lungs.
- Steam inhalation: Regular steam can help remove small particles trapped in the nasal passages and airways.
- Eat health-supportive foods: Include ginger, turmeric, tulsi, citrus fruits, and honey to support respiratory health.
- Keep medicines handy: Asthma patients or those with chronic lung conditions should have doctor-prescribed medications ready.
© 2024 Bennett, Coleman & Company Limited

