- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
THIS Type of Vape Could Secretly Spike Your Blood Pressure and Heart Rate, Scientists Warn

Credits: Canva
E-cigarettes were once marketed as the sleek, “clean” alternative to traditional smoking, a gadget-friendly way to puff without the ash, tar, and lingering stench. But now, researchers are pointing fingers at a specific type of vape that might be giving your heart more trouble than you thought: the so-called “clear” vape.
These transparent-looking devices may seem lighter, fresher, and even harmless. But beneath the smooth packaging lie hidden synthetic cooling compounds that mimic the icy blast of menthol without the signature minty flavour. Unfortunately, this does not just tingle your throat; it quietly ramps up your blood pressure and heart rate.
The experiment that blew the cover
A joint study by Yale University and Boston University put these vapes to the test, with volunteers aged 18 to 45 puffing in carefully controlled conditions. Participants abstained from food, caffeine, tobacco, and exercise for hours before the trial, ensuring their baseline readings were squeaky clean. Then came the real test of steady three-to-four-second drags every 30 seconds over ten minutes.
Blood pressure and heart rate were recorded ten minutes after vaping. At the start, the numbers looked similar whether people used “clear” or non-clear vapes. But the aftermath told a different story. Users of “clear” e-cigarettes experienced a sharper spike in systolic and diastolic blood pressure, mean arterial pressure, and heart rate. In plain terms, their hearts were pumping harder and their blood vessels working overtime.
Why “clear” is not so clear
Unlike flavoured alternatives, “clear” vapes do not smell or taste like candy or fruit. They rely on synthetic chemicals that trick the body into sensing a cooling effect. It feels refreshing, almost like an icy drink on a hot day, but your cardiovascular system sees it differently. Researchers warn that these findings should set off alarms for regulators. With flavour bans becoming more common worldwide, unmonitored products like these might quietly slip through the cracks unless closely watched.
“Surveillance of new products is critically needed,” the team concluded, “to maximise the impact of flavour bans and protect adolescents and young adults.”
Vaping today, smoking tomorrow?
This is not the only piece of bad news about vaping that surfaced recently. A separate study from the University of York and the London School of Hygiene and Tropical Medicine found that young people who vape are three times more likely to take up smoking later in life.
Dr Su Golder, Associate Professor in Health Sciences at the University of York, said that the consistency in the evidence is striking. Across multiple studies, the trend remains the same: vaping acts like a gateway, nudging teenagers towards traditional cigarettes and all the well-documented harms that follow.
Her colleague, Dr Greg Hartwell, echoed the concern, saying that vaping often leads to smoking, which, of course, in turn, opens the door to the multitude of harms that conventional cigarettes bring.
Beyond the heart: other hidden harms
While clear vapes have their own cardiovascular red flags, the wider body of research on e-cigarettes is hardly comforting. Studies have linked vaping to increased risks of asthma, coughing, airway irritation, and possibly even mental health struggles like depression. Other reports point to connections with drug use, raising eyebrows about the broader behavioural consequences.
In short, it is not just your heart under pressure. Your lungs, mental health, and overall wellbeing could be caught in the crossfire too.
The UK crackdown on disposables
Governments are starting to notice. In the UK, as of 1 June, businesses can no longer sell or supply single-use vapes. While the move was partly driven by environmental concerns, discarded vapes are a toxic nightmare for wildlife. It also aims to curb the alarming rise of underage vaping. More than half of children who admitted to using vapes said they preferred disposable versions, making them a prime target for regulation.
“These products are not just an eyesore.” a government statement explained that they pose a huge risk to both the environment and to young people’s health.
In a nutshell, vaping, especially the “clear” kind, is not the harmless hobby it is often marketed to be. From spiking blood pressure to potentially paving the way toward smoking, these sleek devices carry more baggage than their transparent look suggests.
Menopause Clinics Explained: Latest Launch By Maharashtra And Kerala Government

Credits: Canva
The World Health Organization (WHO) noted that menopause often goes unnoticed as a clinical priority, observing these unmet needs, the state governments in Maharashtra and Kerala will soon launch government-run menopause clinics. These clinics will have specialized support systems designed to offer holistic healthcare services for menopausal women within the public system.
These clinics will also have medical consultations, mental health counselling, targeted screening services and lifestyle guidance.
What Are Menopause Clinics?
Menopause clinics are specialized healthcare units, usually housed in government hospitals, urban health centres or district hospitals, that focus on both the medical and emotional needs of women transitioning through menopause. Rather than brushing menopause aside as a “natural” phase that needs little attention, these clinics offer organized, evidence-based care that goes well beyond routine outpatient visits.
At the heart of a menopause clinic is a comprehensive, integrated approach that includes:
- Clinical assessment of menopausal symptoms
- Screening for hormonal and physical health issues, such as bone health and heart disease risk
- Mental health support and psychosocial counselling
- Personalized advice on lifestyle, nutrition and mid-life wellness
- Ongoing patient education and structured follow-up
By bringing these services together under one roof, menopause clinics help women cope with day-to-day symptoms while also addressing long-term risks like osteoporosis, metabolic changes and a higher likelihood of cardiovascular disease.
What Is Menopause?
This is the natural, permanent end of menstruation defined as 12 consecutive months without a period. This typically occurs between ages 45 to 55.
Foods That May Help During Menopause
- Soy: A top source of phytoestrogens, particularly isoflavones, which bind to estrogen receptors in your body. Studies suggest soy may help alleviate hot flashes, improve cholesterol levels, and even reduce the risk of heart disease during menopause.
- Flaxseed: Packed with lignans, a type of phytoestrogen with mild estrogenic effects, flaxseed may also offer some relief.
Including these foods in your diet could help ease symptoms and reduce your risk of certain menopause-related conditions.
Why a Balanced Diet Matters
A nutrient-packed, balanced diet is the foundation of good health at any age. Prioritize:
- Vegetables and fruits: Rich in vitamins and antioxidants.
- Whole grains: Great for maintaining steady blood sugar levels.
- Lean proteins: Support muscle health and repair.
- Low-fat dairy: Provides calcium for bone strength.
- Avoid ultra-processed junk foods, excessive sugar, and unhealthy fats, which contribute little beyond empty calories.
Maharashtra Menopause Clinic
Earlier this January, the Maharashtra government rolled out the country’s first state-run menopause clinics across government hospitals and urban health facilities. The initiative was launched on Makar Sankranti, January 14, under the guidance of Minister of State for Health Meghna Bordikar.
As per official statements, these clinics are designed to offer end-to-end care in one place. Services include expert medical consultations to evaluate and manage menopausal symptoms, mental health support to address emotional and psychological concerns, and screenings for bone health, cardiovascular risk and hormonal balance. Medicines and follow-up advice are also provided during the same visit, cutting down the need for multiple referrals and repeat hospital trips.
A senior health official pointed out that while menopause is a natural life stage and not a disease, many women need consistent physical and emotional support during this transition. The strong response from women across Maharashtra highlights a long-standing gap in healthcare, where menopause-related concerns often went unaddressed due to the absence of dedicated services. With this move, Maharashtra has also set an example for other states looking to introduce gender-specific care within public health systems.
Read: Can Your Diet Affect Menopause?
Kerala follows with dedicated clinics
Taking a cue from Maharashtra, the Kerala government has announced plans to set up specialized menopause clinics in district hospitals. An initial allocation of Rs 3 crore has been earmarked for the project in the 2026 state budget, presented by Finance Minister K N Balagopal.
The proposed clinics in Kerala will follow a similar model, offering medical consultations for menopausal symptoms, mental health counselling, and screenings for heart, bone and hormonal health. Women will also receive medicines along with lifestyle and dietary advice at a single facility.
The initiative acknowledges the wide-ranging impact of menopause, including hormonal changes, sleep disturbances, bone health issues and increased stress, and aims to create a one-stop support system within district hospitals. By bringing menopause care into mainstream public healthcare, Kerala hopes to improve access, reduce stigma and ensure that women receive timely, structured support during this phase of life.
Bruce Willis’ Wife Emma Says He Is Unaware of His Dementia Diagnosis
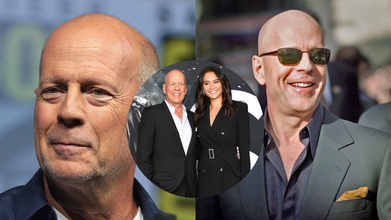
Credits: Wikimedia Commons
Bruce Willis was diagnosed with frontotemporal dementia in 2022. His wife, Emma Heming Willis recalled the day when Bruce was diagnosed with the condition and how it made her feel "lost, isolated and afraid." Talkin to PEOPLE, Emma said, Bruce "never connected the dots" that he has been diagnosed with frontotemporal dementia. “I think that's like the blessing and the curse of this, is that he never connected the dots that he had this disease, and I'm really happy about that. I'm really happy that he doesn't know about it,” she shared about Bruce, 70.
Bruce Willis' Diagnosis
"On the day Bruce got his diagnosis, we walked out of the doctor's office with a pamphlet and an empty goodbye. No plan, no guidance, no hope, just shock," she explained in front of a packed auditorium, People reported.
In one instant, the family's future disappeared. The Oscar-winning actor, famous for his quick wit and performances in Die Hard and The Sixth Sense, would be leaving his career behind. Emma found herself thrust into a whole new role of full-time caregiver at the same time.
She continued to explain, "I found myself having to keep my family intact, raise our two small girls, and tend to the man that I love while dealing with an illness I hardly knew anything about."
Emma's emotional candor resonated with hundreds of families who have received similar diagnoses and encouraged her to author a book, The Unexpected Journey, scheduled for publication in September. In Emma's words, "This is the book I hope will assist the next caregiver. It is packed with encouragement, wisdom, and the encouragement necessary to walk this path.
What Is Frontotemporal Dementia?
Frontotemporal dementia is a less prevalent type of dementia that mainly occurs in the frontal and temporal lobes of the brain. It tends to affect behavior, personality, language, and movement more than memory, particularly in its initial stages.
In contrast to Alzheimer's, which generally strikes older individuals, FTD can hit at an earlier age—sometimes as young as 40. The symptoms can range from changes in personality, emotional flatness, or the inability to show empathy to impulsiveness, so it is especially hard for spouses and children to cope.
Emma's case illustrates how abrupt and disrupting this diagnosis can be—not only for the patient but for caregivers as well.
Whereas Bruce Willis' diagnosis hit global headlines, the mental toll taken by Emma, his caregiver, was largely in the background—until she decided to come forward.
Caregiving is a respectable position, but it's also a challenging and thankless one. For those who are caring for loved ones with dementia or other chronic illnesses, the stress of "keeping it all together" can result in a condition called caregiver burnout.
"Caring for someone is the most intimate and demanding work of love," Emma explained, "but when you're not noticed or supported, it begins to undermine your health—mentally and physically."
‘Work Stress Makes You Gay’: Why Malaysian Minister's Remark Proves The Need To Understand Sex, Gender And Sexuality

Credits: X and Canva
Work stress could make you gay, said a Malaysian minister Zulkifli Hasan, as continued government intervention of what is described as 'sexually deviant behavior' has pressured the country's LGBTQ community. This happened two weeks after religious authorities and police acted on complaints from a sultan and Islamist politicians that a camping retreat was promoting the LGBTQ lifestyle, reported South China Morning Post.
Religious Affairs Minister Hasan on Tuesday said that work stress could be among many other factors that is pushing people into sexual orientations other than heterosexuality. “Societal influence, sexual experiences, work stress and other personal factors come under this category [of possible causes],” Zulkifli said in a written parliamentary reply to a question by Siti Zailah Mohd Yusoff, a lawmaker with the opposition Islamist party PAS.
Also Read: Andy Kershaw Diagnosed With Spinal Cancer That Left Him Unable To Walk
He cited a 2017 study by Sulaiman et.al., that said such elements "can contribute to the increase in LGBT acts".
His comments have attracted a lot of backlash, with many people on social media mocking him. A social media user Muaz Zam said, "By this logic, I am genuinely shocked my entire office isn't gay by now". Another one read: "In other words: they never work hard in the parliament."
However, these claims are not scientifically back. Work related stress can impact a person, but cannot change their sexuality. It can, however, cause health effects. What it does not do is change one's sexuality and this is why one should know the difference about gender, sex and sexual orientation or sexuality.
'Work Stress Makes You Gay': The Difference Between Gender vs Sex

While these both terms are often used interchangeably in official forms, there is a difference between the two.
As per the Council of Europe, gender is an area that cuts across thinking about society, law, politics, and culture.
Read: Trump Administration Deadnames Transgender Former HHS Officer Rachel Levine in Official Portrait
Definition Of Gender vs Sex by WHO
The World Health Organization notes that sex refers to: "the different biological and physiological characteristics of males and females, such as reproductive organs, chromosomes, hormones, etc.”
Whereas, gender refers to: "the socially constructed characteristics of women and men – such as norms, roles and relationships of and between groups of women and men. It varies from society to society and can be changed. The concept of gender includes five important elements: relational, hierarchical, historical, contextual and institutional. While most people are born either male or female, they are taught appropriate norms and behaviours – including how they should interact with others of the same or opposite sex within households, communities and work places. When individuals or groups do not “fit” established gender norms they often face stigma, discriminatory practices or social exclusion – all of which adversely affect health."
Definition Of Gender vs Sex by The European Institute For Gender Equality
“Sex refers to the biological and physiological characteristics that define humans as female or male. These sets of biological characteristics are not mutually exclusive, as there are individuals who possess both, but these characteristics tend to differentiate humans as females or males.”
“Gender refers to the social attributes and opportunities associated with being female and male and to the relationships between women and men and girls and boys, as well as to the relations between women and those between men. These attributes, opportunities and relationships are socially constructed and are learned through socialisation processes. They are context- and time-specific, and changeable. Gender determines what is expected, allowed and valued in a woman or a man in a given context. In most societies, there are differences and inequalities between women and men in responsibilities assigned, activities undertaken, access to and control over resources, as well as decision-making opportunities. Gender is part of the broader sociocultural context. Other important criteria for sociocultural analysis include class, race, poverty level, ethnic group and age.”
The main difference is that gender is a social construct, whereas sex is the biologically labelled term based on organs and hormones.
Read More: Trump's Top Health Nominee Wants ‘Corrective Care’ For Trans People
What Is Sexuality?

As per the American Psychological Association (APA), sexuality is the capacity to derive pleasure from various forms of sexual activity and behavior. The Lanarkshire Sexual Health describes sexual orientation as a way to describe the feelings you have for someone you fancy or are attached to.
While sexuality can change overtime, it is not a choice. There is no evidence that sexual orientation can be forced to change through therapy.
Can Stress Impact Sexuality?
While stress can impact sexual function by reducing libido, causing fatigue, and triggering hormonal changes, it does not change one's sexual orientation. Jason Teoh, who writes on LGBTQ issues, project partner at NSW Department of Planning, Housing and Infrastructure, notes: "Sexual orientation is not caused by stress. It is not caused by trauma, influence or difficult life circumstances."
The WHO notes: sexual orientation is a natural, stable part of human identity shaped by biology, genetics, and early development. The WHO removed homosexuality from its disease classification in 1990. The American Psychiatric Association did the same in 1973.
© 2024 Bennett, Coleman & Company Limited

