- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Those Aren't Mosquito Bites - How To Identify Bed Bug Bites?

(Credit-Canva)
Beds are usually considered a safe place for people; it is a place that you can always count on to help you rest and recuperate no matter how tough things get. However, sometimes this safe place can become home to some unwanted guests. While our parents would often urge us to make sure our beds remained clean and no food articles remained on it, sometimes leaving things here and there does not seem like a big concern for us. However, this could also be an invitation for bed bugs to enter the equation.
According to the U.S. Environmental Protection Agency (EPA) bed bugs are public health pests. While they do not transmit any diseases, they can cause our physical, mental as well as economical health to suffer. Severe health consequences to them can include allergic reactions which could be on the spectrum of small rashes to anaphylaxis, which is a full body reaction. It can also cause anxiety, insomnia and impact people’s mental health. However, how does one distinguish bed bug bites to normal insect bites?
NHS Guidance on Bed Bugs and Their Bites
The National Health Service (NHS) highlights that bed bugs can hide in various locations, including bed frames, mattresses, clothing, furniture, behind pictures, and under loose wallpaper. They identify three key signs of a bed bug infestation:
Bites: Often appearing on exposed skin areas during sleep, such as the face, neck, and arms.
Blood Spots: Small spots of blood on bedding, resulting from bites or crushed bed bugs.
Brown Spots: Tiny brown spots (bed bug excrement) found on bedding or furniture.
On fair skin, bed bug bites typically appear red, while on darker skin, they may look purplish and can be less noticeable. Reactions to bites vary; some people experience intense itching and painful swelling. Generally, bed bug bites resolve on their own within a week or two.
How Can You Treat Bed Bug Bites?
To manage bed bug bites, the NHS recommends several self-care measures. Applying a cool, damp cloth to the affected area can help alleviate itching and swelling. It's also important to keep the bite area clean to prevent any potential infections. Finally, resisting the urge to scratch the bites is crucial in minimizing the risk of further irritation or infection. Some over the counter products that you may get for relief may include mild steroid creams like Hydrocortisone cream can help ease the itching associated with bed bug bites. NHS notes that children under 10 and pregnant women should consult a doctor before using hydrocortisone cream. You may also be given Antihistamines, which provide relief if the bites are severely itchy and interfere with sleep.
How Can You Get Rid Of Them?
The NHS suggests that if you have bed bugs, it's best to get in touch with your local council or a pest control company. Getting rid of bed bugs on your own can be really tough because they can hide well and some bug sprays don't work on them. While there are a few things you can try yourself, they probably won't completely solve the problem.
COVID And Flu Could Increase Your Risk Of Heart Attacks Or Stroke: American Heart Association Study

(Credit-Canva)
As COVID and viral infections cases rise in numbers, researchers are finding out how, following the bout of cases, the risk of heart diseases has also increased in people. To explore this connection, new research published today in the Journal of the American Heart Association reveals a strong link between both acute and chronic viral infections and an increased risk of serious cardiovascular events, such as heart attacks and strokes.
The lead author, Dr. Kosuke Kawai, noted that while we know viruses can cause cancer, their link to non-infectious diseases like heart disease hasn't been clear. This study confirms that acute (short-term) and chronic (long-term) viral infections are connected to both immediate and lasting risks for heart and brain events.
How Do Short Infections Cause Harm To Heart?
When your body fights off a virus, your immune system releases chemicals that cause inflammation (swelling) and make your blood more likely to clot. Both of these problems can linger even after the virus is gone.
This ongoing inflammation and tendency to clot can damage the heart and blood vessels, which is likely why the risk of a heart attack or stroke spikes so dramatically right after an illness.
The research details what happens to your heart risk right after you get a respiratory infection. The study combined data from many high-quality reports and found a major, temporary jump in risk:
Influenza (Flu)
In the month immediately following a confirmed flu infection, people were 4 times more likely to have a heart attack and 5 times more likely to have a stroke compared to when they weren't sick.
COVID-19
After a COVID infection, the risk was also high. People were 3 times more likely to have a heart attack and 3 times more likely to have a stroke in the first 14 weeks. Worryingly, this risk stayed higher than normal for an entire year.
What Infections Cause Long-Term Heart Risk?
This part of the study focused on people who have had certain chronic (long-lasting) viral infections, tracking their health for an average of over five years to see if their risk remained high:
HIV Infection
People with HIV had a 60% higher risk of heart attack and a 45% higher risk of stroke.
Hepatitis C
This infection was linked to a 27% higher risk of heart attack and a 23% higher risk of stroke.
Shingles (Herpes Zoster)
Even this common virus was associated with a 12% higher risk of heart attack and an 18% higher risk of stroke.
Even though these percentage increases are smaller than the immediate post-flu/COVID jump, they are still very important because the risk lasts for years. Shingles, for example, affects about one in three people in their lifetime, meaning that this seemingly small increase in risk will lead to a large number of extra heart problems across the general population over time.
How Can We Prevent Risk Of Heart Attacks After Infections?
The study suggests a powerful way to fight these risks is by getting vaccinated. The findings strongly support the idea that increasing the number of people who get flu, COVID, and shingles shots could lower the overall rate of heart attacks and strokes in the community. As an example, previous research has shown that getting a flu shot can be linked to a 34% lower risk of major heart problems.
The American Heart Association recommends that everyone, especially those with existing heart conditions or heart risk factors, talk to their doctor about getting the right vaccines. Vaccination is a simple step that offers crucial protection to people whose hearts are already vulnerable.
It’s important to remember that this study was based on looking at people's health records (observational studies), not on controlled experiments. The main focus was on single viruses. Researchers noted that we still need more studies to fully understand how some other viruses, like dengue and HPV, might be linked to heart disease.
Is India Drinking More Than The Rest Of The World? Recent Report Reveals
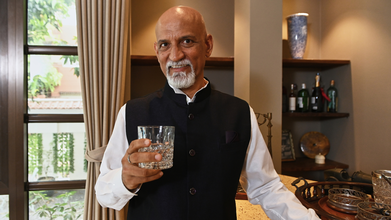
Credits: Canva
Is India getting drunk? While rest of the world is cutting its alcohol consumption, India's shows some contradicting results. As per a London-based market analytics firm Euromonitor International, the country is projected to consume an additional 357 million litres between 2024 and 2029. This is the biggest increase anywhere in the world.
the report titled World Market for Alcoholic Drinks 2025 notes that the there is a stagnating overall in alcohol consumption, and the only high points are countries like India, Brazil, Mexico, and South Africa.
Why Are Indians Drinking So Much?
The reason is Zebra Stripping. What exactly is that? Zebra Stripping is the act of switching between alcoholic and non-alcoholic drinks in the same social setting. The Print reported that people in India are moderating their alcohol consumption, rather than completely dismissing it. People, however, are avoiding binge drinking, and switching to zebra stripping.
Health is the main driving factor of this change. There is a generational divide among the Gen Z adults of legal drinking age. As 36% of them have never consumed alcohol. This is the case globally too. For instance, in the US, the National Institute of Drug Abuse shows that lifetime drinking, past month drinking, and past year drinking among young people have declined from year 2000. This means that the decline is most severely seen among the Gen Z, those who are born between 1997 to 2012.
Despite this drop in Gen Z drinkers, the report, aforementioned, shows the number of alcohol consumers will only increase.
How Can Alcohol Affect Your Body?
The National Institute on Alcohol Abuse and Alcoholism notes that alcohol could lead to organ damage and immune dysregulation. Alcohol could cause cardiac arrhythmias, cardiomyopathy, ischemic heart disease, hypertension, ischemic stroke or hemorrhagic stroke, acute respiratory disease, distress syndrome, pneumonia, oesophageal cancer, and oral cavity cancer.
Other impact that alcohol could cause on one's body are:
- Steatosis or fatty liver
- Steatohepatitis
- Fibrosis
- Cirrhosis
- Alcohol-associated hepatitis
- Liver Cancer
- Myopathy
- Muscle wastage
- Acute pancreatitis
- Chronic pancreatitis
- Gut leakiness
- Microbial dysbiosis
- Colorectal cancer
- Impaired fracture repair
- Reduce bone density
It can also increase the risk of liver, colon, breast, oral cavity and rectum cancer.
The Centers for Disease Control and Prevention (CDC), USA, notes that around 178,000 deaths have happened in the US, annually, just by excessive alcohol use. CDC notes that while drinking levels at any point is not safe, moderate alcohol use is only up to two drinks or less in a day for men, and one drink or less in a day for women.
Apart from the diseases and chronic conditions, CDC notes that alcohol use could also lead to injuries through motor vehicle crashes, falls, drownings, and burns. It could also lead to violence, overdose, alcohol poisoning, sexual transmitted infections, miscarriage, stillbirth, or fetal alcohol spectrum disorder (FASD).
Study Reveals How Manipulative People Use THIS As A Weapon: Psychology Of Narcissists

(Credit-Canva)
Manipulation, according to the American Psychological Association, is behavior designed to exploit, control or otherwise influence others to one’s advantage. Some people Some people do this with words; others through actions. In a new study, researchers found that there is another act that manipulators often use to their advantage.
We think of a hug or a hand on the arm as comforting and connecting. But a new study suggests that these simple actions can hide a darker intention. Research in the journal Current Psychology reveals that people who are manipulative and self-centered (narcissistic) often use touch to calculate how to influence or control their romantic partners.
Senior researcher Richard Mattson points out that in these relationships, you not only miss out on the good feelings that touch usually brings like lower stress and a boost of the "love hormone" oxytocin, but the touch is actively used to benefit the manipulative person, often hurting their partner in the process. This work connects how someone touches with who they are.
How Do Narcissists Manipulate With Touch?
Most studies look at the positive effects of touch, but this research focused on the opposite: when touch is used to harm or trick someone. The study centered on people who showed traits belonging to the "Dark Triad," which is a group of three linked, negative personality traits:
Narcissism: Being extremely self-focused, needing admiration, and lacking empathy for others.
Psychopathy: Having very little empathy (inability to understand others' feelings) and acting impulsively.
Machiavellianism: Being cunning and manipulative to reach personal goals, often deceiving others.
The researchers surveyed over 500 college students about their comfort with touch and how they used it in relationships. They found that people with high levels of these dark traits were significantly more likely to use touch as a tool to control, influence, or manipulate their romantic partner, proving it wasn't about affection but about power.
Does Gender Affect How Manipulators Act?
The study revealed some interesting gender-based difference in how these manipulative traits showed up:
Men with these darker traits tended to use touch in an effort to feel more connected to their partner. This was especially true if they already felt insecure or unstable in the relationship, using touch as a way to reinforce their bond or ease their own anxiety.
Women with "Dark Triad" traits often reported feeling uncomfortable when they were touched by others. However, they were still more likely than others to use touch themselves as a means of controlling or influencing their partner.
Experts summarized the core attitude of these personality types as "me first, you second." This self-serving belief is so strong that it affects even how they handle affection and physical closeness—an important part of any relationship.
Can Recognizing Signs Help Build Better Relations?
People with high "Dark Triad" traits often have romantic relationships that are short-lived, troubled, and complex.
The study's findings offer a path toward solutions. Since touch is a powerful, low-cost tool for providing support and promoting better health, Mattson suggests this information can help create new interventions. The goal is to "leverage touch" to teach people, especially those who avoid touch or use it to manipulate, how to use it in healthy, caring, and mutual ways. Instead of using touch for control or self-protection, they could learn to use it to truly connect and support someone else.
© 2024 Bennett, Coleman & Company Limited

