- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Is The Hottest Temperature A Human Body Can Handle?

Credits: Canva
As temperatures around the world rise because of climate change, the human body is increasingly confronting a little-understood and increasing hazard: excessive heat. From enduring heatwaves to sweltering heat waves with high humidity, what used to be a seasonal annoyance is now a worldwide health risk. But how hot is too hot for the human body? At what point does heat become deadly—and why?
In 2020, an article published in Science Advances identified a precise threshold by which the human body cannot survive: 95°F (35°C) wet-bulb temperature. Unlike regular temperature readings, wet-bulb temperature takes into consideration both heat and humidity. It is measured with a thermometer covered in a cloth soaked in water, replicating the way the human body dissipates heat—by evaporating sweat.
If the air surrounding the body is too moist, sweat does not evaporate. When this system breaks down, so does the body's control over internal temperature. The result? A speedy and potentially dangerous increase in core temperature.
In perspective, 115°F (46.1°C) air temperature with 30% humidity yields a wet-bulb temperature of approximately 87°F (30.5°C)—still survivable. However, a seemingly "cooler" 102°F (38.9°C) day with 77% humidity brings the wet-bulb temperature to the lethal 95°F (35°C) mark.
Once wet-bulb temperatures reach this tipping point, sweat can no longer evaporate fast enough to cool the body. Even if the skin is wet, the internal temperature continues to climb. At this stage, hyperthermia sets in—defined by a body temperature above 104°F (40°C)—leading to symptoms like confusion, rapid heart rate, organ failure, and even death.
Who’s Most at Risk?
Although no human can live above a wet-bulb temperature of 95°F, not all people are equally at risk in lower heat exposures.
- Older people, because of impaired thermoregulation.
- Obese or chronically ill people, such as those with cardiovascular disease.
- Those on certain medications, e.g., antipsychotics or beta-blockers.
- Workers outdoors and athletes, whose exertion increases body heat.
Even healthy individuals can succumb to lower wet-bulb temperatures if they are exerting themselves in direct sun or in poorly ventilated environments.
What Happens Inside the Body During Heat Exposure?
The human body contains approximately 60% water, and fluid balance is inextricably linked with temperature regulation. In hot temperatures, the body loses water quickly through sweat and respiration. If it is not replaced, dehydration occurs, causing blood volume to decrease. This affects anything from organ function to delivery of oxygen at the cellular level.
Meanwhile, the thermoregulatory system, which depends on blood flow to shuttle heat from internal organs out to the skin, starts to fail. If this cooling circuit fails, internal organs become overheated, cells start dying, and a chain of failure results in heat stroke or cardiovascular collapse.
How Hot Is Too Hot, Really?
Whereas wet-bulb temperature gives us one measurement, research indicates the ambient air temperature limit of human survival is probably between 104°F and 122°F (40°C–50°C). 122°F is at the limits of what the body can withstand while keeping its core temperature stable, says a 2021 Physiology Report.
A different approach to research implies that the temperature at which the body begins to sweat is 89.6°F (32°C)—the beginning of heat strain. Thus, danger doesn't begin at extreme temperatures only; it accumulates with time, particularly due to long exposure and high humidity.
The U.S. Environmental Protection Agency (EPA) has documented that heat directly caused 11,000 fatalities in the United States between 1979 and 2018, although the actual number is probably much greater because underreporting is likely to have occurred. While hurricanes or flooding may be dramatic, they kill openly, but heat waves are deadly killers that silently take victims in poor communities, older people, and those not having air conditioning.
Moreover, heat exacerbates existing conditions, increasing the possibility of strokes, heart attacks, and breathing difficulties during heat waves.
How to Survive Extreme Heat?
We may not be able to manipulate the weather, but we can manage our environment and lifestyle. Experts advise:
- Rehydrate with electrolytes, not plain water. Sweating excessively loses salt and minerals necessary for cellular processes.
- Lower internal body temperature by bathing or showering with cool water.
- Avoid sun exposure, particularly between 10 AM and 4 PM.
- Dress in light, loose clothing and have lighter, more frequent meals.
Use extra caution with electric fans during high heat; they can accelerate evaporation and boost dehydration.
In addition, the Centers for Disease Control and Prevention (CDC) recommends visiting during heatwaves susceptible populations—i.e., people who are frail or have disability and ensuring air conditioning, shades, or available cooling resources like fans or air conditioning are at their disposal.
The highest temperature that a human can tolerate is not one number—it's a function of heat, humidity, and time. Wet-bulb temperatures over 95°F are universally lethal within a few hours, but even lower temperatures can be severely dangerous under the right conditions. As climate change accelerates, our knowledge of and readiness for extreme heat must keep pace. This isn't merely a meteorological issue—it's a public health emergency in the making.
The Hidden Glaucoma Warning Signs Every Middle-Aged Adult Should Know
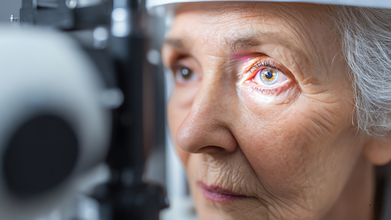
Credit: Canva
Glaucoma is an umbrella term for a group of eye diseases that create pressure inside your eyeball, which can damage delicate, critical parts at the back of your eye, including the optic nerve.
While most of the diseases are progressive, meaning they gradually get worse and eventually cause permanent vision loss and blindness. In fact, glaucoma is the second-leading cause of blindness worldwide and is the leading cause of blindness for people over 60 years old.
Dr Niteen Dedhia, Medical Director, Ojas Maxivision Eye Hospital tells Business Standard: "Glaucoma slowly and quietly causes damage to the optic nerve. Changes in eye pressure, blood flow and nerve fibres occur over time, while the brain often compensates for the loss.
"As a result, symptoms go unnoticed, and by the time vision loss becomes apparent, the damage is usually permanent."
Many forms of glaucoma have no warning signs and the effect is extremely gradual, to the point that you may not notice a change in vision until the condition is in its late stages.
Here are some symptoms that mid-age people need to keep an eye out for:
1. Gradual loss of circumferential vision
One of the earliest symptoms of glaucoma is damage and subsequent loss of peripheral vision. Dr Dedhia noted: “Glaucoma starts by damaging the peripheral vision but doesn’t affect the centre (front) vision."
If you seem to struggle with spotting objects approaching from the side or bump into things more often, you may be experiencing early stages of the disease and not merely experiencing normal ageing.
2. Difficulty seeing or reading in the dark or low light settings
Difficulty adjusting to darkness, discomfort in dimly lit spaces or having trouble navigating at night can be early warning signs may point to reduced contrast sensitivity linked to glaucoma rather than simple eye strain.3. Frequent changes in eye power
Dr Neeraj Sanduja, Ophthalmologist, Eye Surgeon at Viaan Eye Centre, Gurgaon told the publication: "Needing frequent prescription changes or feeling that glasses 'never feel quite right' may reflect subtle visual field changes caused by glaucoma rather than simple refractive error progression."
4. Eye pressure or unusual discomfort
Open-angle glaucoma, the most common form of the condition that causes patchy blind spots in your side vision, is often painless or limited to a mild sense of pressure or heaviness in the eyes.
Those suffering from open-angle glaucoma may notice a dull ache after prolonged screen time or reading that improves with rest. Frequently mistaken as regular eye strain, it is often ignored, however, may indicate subtle increases in eye pressure that require professional evaluation.
5. Frequent headaches with eye strain
Frequent headaches, especially when accompanied by eye strain or blurred vision, should not be ignored as migraine pain as it may signal rising eye pressure or early glaucoma changes, Dr Dedhia warns.
Who Is at Risk for Glaucoma?
Certain groups of people have a higher than normal risk of getting glaucoma which includes those who:
- have high eye pressure
- are farsighted or nearsighted
- have had an eye injury
- use long-term steroid medications
- have corneas that are thin in the center
- have thinning of the optic nerve
- have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body
- are over age 40
- have family members with glaucoma
- are of African, Hispanic, or Asian heritage
Sleeping Too Much or Too Little Raises Liver Disease Risk, Study Finds

Credit: Canva
Abnormal sleeping patterns, whether excessive or brief, can significantly increase your risk of developing chronic liver disease, an EMJ study suggests.
Sleep duration has previously been linked to worsening your chances of Type 2 diabetes; obesity; cardiovascular diseases including hypertension, stroke, heart attack; mental disorders such as depression, anxiety; weakened immune system and potentially contributing to neurological conditions such as dementia.
However, researchers have now also found that sleep disruption may intensify existing stress on the liver which can worsen metabolism and pave the way for disease progression.
The authors noted that poor sleeping habits may influence liver health for multiple reasons including by altering glucose metabolism, increasing inflammation and disrupt circadian rhythms that regulate liver function.
"Participants who reported consistently short sleep duration were more likely to have elevated liver enzymes and higher fibrosis risk scores compared with those reporting moderate sleep duration. Long sleep duration was also associated with adverse liver markers, though the relationship was weaker than that observed for short sleep," the study noted.
Despite discovering links, the involved researchers noted that the study only highlighted sleep as a potential factor that could worsen liver function along with other lifestyle reasons and did not act as a clear cause.
Why Is Chronic Liver Disease A Concern?
Once a rare condition, non-alcoholic fatty liver disease (NAFLD) now affects one in three Indians. A JAMA study has now found that about 40 percent of the global population is now suffering from NAFLD, with abdominal obesity identified as its single biggest risk factor.
Researchers found that nearly 70 percent of people with Type 2 diabetes and about 80 percent of those with obesity are affected by NAFLD. They also discovered that NAFLD prevalence is higher in men than in women, with rates of 15,731 per 100,000 population in men compared with 14,310 in women.
READ MORE: This Deadly Liver Disease Is Affecting People In Their 20s And This One Symptom Is The Red Flag
Between 2010 and 2021, India recorded a 13.2 percent increase in age-standardized prevalence, ranking just behind China at 16.9 percent and Sudan at 13.3 percent. Additionally, the disease peaks earlier in men, between 45 and 49 years of age, while women show the highest prevalence between 50 and 54 years.
NAFLD, now called as metabolic dysfunction-associated steatotic liver disease (MASLD), is when excess fat builds up in the liver, unrelated to heavy alcohol use, due to obesity, Type 2 diabetes, high blood pressure and cholesterol.
It ranges from simple fat accumulation to inflammation and damage, which can progress to fibrosis, cirrhosis or liver cancer, The disease often has no symptoms and is managed with lifestyle changes such as diet and weight loss.
Why Is NAFLD on the rise?
Poor diets (high carbs/sugar), sedentary habits and rising obesity are some of the key reasons why an uptick in NAFLD cases has been seen pan-India. Increased intake of refined carbs, sugary drinks, processed foods and unhealthy fats can increase the risk of obesity, diabetes, hypertension and high cholesterol which can pave the way for this liver disease.
Experts also note that working long hours at desks without any proper physical activity can lead to weight gain and fat accumulation in the liver.
According to the Union Health Ministry, the prevalence of the condition could be in the range of 9-53 percent. Multiple other health studies also suggest nearly 40 percent of urban Indians may have some form of fatty liver disease
Hepatologist Dr Cyriac Abby Philips, popularly known as LiverDoc on social media, noted on X that many patients do not realize that timely lifestyle changes can completely reverse the condition. “All it takes is being in charge of your body and health. No shortcuts—go slow and steady,” he wrote.
If left untreated, NAFLD can progress to Non-Alcoholic Steatohepatitis (NASH), where liver inflammation begins. Over time, this inflammation can lead to scarring of the liver, known as fibrosis. Advanced fibrosis results in cirrhosis, which severely affects liver function.
NAFLD can also increase the risk of chronic liver disease, liver failure and hepatocellular carcinoma. Many patients diagnosed with liver cancer have a history of untreated fatty liver.
Unique Symptoms Of Alzheimer's Disease And How It Can Be Managed
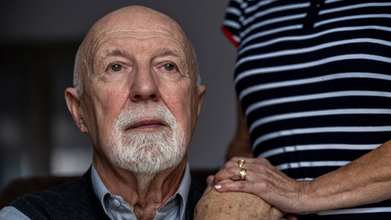
Credits: iStock
Over 2 million Americans have Alzheimer's. It is the most common cause of dementia and is a progressive disease. This means the disease will get worse, however, it could be managed, though cure is not available. It is the biological process that begins with the appearance of a buildup protein in the form of amyloid plaques and neurofibrillary tangles in the brain. This causes brain cells to die over time and the brain to shrink.
What Makes Alzheimer's So Unique?
The fact that there is no cure for Alzheimer's disease is one of the most unique part of the condition. In advanced stages, loss of brain function can cause dehydration, poor nutrition or infection.
The symptoms of Alzheimer's are unique because the signs are easily miss-able. These signs could seem like a day to day problem and not anything serious. At first, it starts with trouble in remembering recent events or conversations. Over time, memory gets worse and other symptoms occur.
While everyone could have trouble with memory at times, the memory loss that happens with Alzheimer's is lasting. The signs could be:
- Repeat statements
- Repeating questions over and over
- Forgetting conversations, appointments and events
- Misplacing items, and putting the in odd places
- Getting lost in places you know very well
- Forgetting names of family members
- Forgetting names of everyday objects
- Have trouble finding the right words, expressing thoughts or having conversations
Unique Symptoms Of Alzheimer's: Cannot Recognize Numbers
Alzheimer's could also lead to trouble in concentrating, thinking, especially about abstract concepts like number. Your thinking and reasoning abilities take a hit. In fact, in many cases, people with Alzheimer's are not able to recognize numbers.
Unique Symptoms Of Alzheimer's: Cannot Perform Everyday Tasks
There are many tasks that you do in your day to day life, which come easy to you, could become difficult over time. As Alzheimer's advances, people forget how to do basic tasks such as dressing or bathing.
Read: What A Finger-Prick Blood Test Could Mean for Alzheimer’s Diagnosis
Your Personality Changes
With Alzheimer's, your personality too can change, as the disease could affect moods and behaviors. Symptoms include:
- Depression.
- Loss of interest in activities.
- Social withdrawal.
- Mood swings.
- Not trusting others.
- Anger or aggression.
- Changes in sleeping habits.
- Wandering.
- Loss of inhibitions.
- Delusions, such as believing something has been stolen when it hasn't.
Are There Any Treatments Or Cures?
UK researchers say fruit flies could help unlock why devastating brain and nerve conditions such as Alzheimer’s, Parkinson’s and motor neurone disease develop, despite decades of medical research. Scientists have known for years that many neurodegenerative disorders are linked to genetic mutations. What has remained unclear is how those mutations actually trigger disease inside the nervous system.
According to the Mirror, new findings published in the journal Current Biology suggest a breakthrough may lie in studying fruit flies, insects whose genes behave in strikingly similar ways to those in humans.
© 2024 Bennett, Coleman & Company Limited

