- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
You Have Heard Of Blood Thinning, But Do You Know Blood Thickening Can Also Make You Sick?
Recently, a friend's relative was admitted to the hospital after experiencing recurring discomfort and unstable blood sugar levels. Initially, it appeared to be a routine diabetes complication, but it turned out she had something unexpected—her blood was thickening to such an extent that it was making her sick.While blood thinning is often discussed in the context of diabetes and cardiovascular conditions, the dangers of blood thickening, or hypercoagulability, remain largely overlooked.
This woman in her late 60s living with diabetes, was in danger of suffering a life-threatening complications from abnormally clotting blood. Her story highlights an often overlooked medical issue: thick blood can prevent proper circulation, increase the risk of thrombosis, and contribute to all sorts of health complications, including some that prove fatal if ignored.
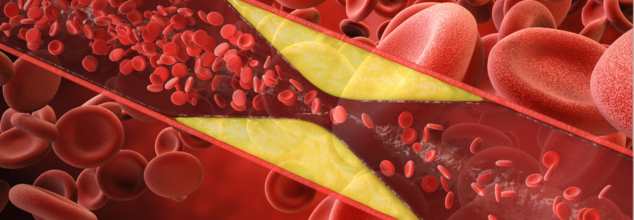
Blood must be in a fine balance to be able to circulate properly and clot when needed. But when there is an imbalance of blood proteins and cells, it becomes too thick. This is called hypercoagulability, and it makes the blood more prone to clotting, which can clog the blood vessels and cause serious health issues like strokes, heart attacks, and deep vein thrombosis.
While blood is homogeneous in appearance, it contains a mix of different components, such as red and white blood cells, platelets, proteins, and clotting factors. When these components exist in a greater quantity than normal, the blood becomes thicker, thus harder for the heart to pump it effectively through the body.
What Causes Blood to Thicken?
There are a number of reasons why blood may become thick, and although some are inherited, others are acquired later in life. Some of the most important causes include:
Overproduction of Blood Cells: Too many red blood cells (polycythemia vera) or platelets can cause thick blood.
Underlying Illnesses: Diseases such as cancer, lupus, and diabetes can interfere with blood clotting mechanisms.
Too Much Clotting Protein: Some people overproduce clotting proteins, which puts them at risk of thrombosis.
Smoking: Smoking harms blood vessels and lowers the body's capacity to form anticoagulant factors.
Inflammation: Elevated inflammatory markers, frequently found in chronic conditions such as diabetes, contribute to clot formation.
Because there is no one definition of "thick blood," physicians diagnose it according to the underlying condition causing abnormal clotting.
Link Between Diabetes and Thick Blood
Diabetes patients are especially vulnerable to thickening of the blood because of elevated glucose, lipid, and inflammatory cytokine levels in the blood. Diabetes encourages the development of plaque in arteries, thus enhancing the likelihood of lethal clots. The condition, which is referred to as thrombosis, may clog arteries and veins and result in fatal complications.
When an individual has diabetes, their platelets (small blood cells responsible for clotting) become hyperactive, and the risk of clot formation becomes higher. Poor circulation and long-term inflammation are also contributing factors. Scarily, research indicates that almost 80% of individuals with diabetes will eventually perish from clot-related complications.
Symptoms of Thick Blood
Most individuals are unaware of their thick blood until a blood clot develops. In others, a family history of clotting disorders will lead to testing before symptoms arise. Warning signs can include:
- Blurred vision
- Dizziness
- Frequent headaches
- Easy bruising
- High blood pressure
- Shortness of breath
- Fatigue and lack of energy
- Excessive menstrual bleeding (in women)
- Itching skin
- Gout (a type of arthritis brought on by an excess of uric acid in the blood)
If you have unexplained clotting, multiple pregnancy loss (greater than three first-trimester miscarriages), or a family history of clotting diseases, see a physician for screening.
What Tests Can Detect Hypercoagulability?
In diagnosing thick blood, physicians review the complete medical history and perform blood tests in phases. Some of the most frequently performed tests are:
Complete Blood Count (CBC): Tests for elevated red blood cell or platelet counts.
Activated Protein C Resistance Test: Finds the presence of Factor V Leiden, which is a genetic mutation linked with blood clotting disorders.
Prothrombin G20210A Mutation Test: Finds abnormality in the blood clotting factors.
Antithrombin, Protein C, and Protein S Levels: Assists in finding conditions like lupus anticoagulants.
These tests being expensive and highly specific, physicians would typically start with more general screening tests and proceed to more specialist diagnostics.
How Can You Reduce the Risk of Thick Blood?
Although some reasons for thick blood are genetic and cannot be avoided, life-style changes and medical treatment may decrease risks in people with diabetes or other predisposing factors. Preventive strategies include:
- Circulation is improved and blood kept from becoming sluggish through exercise.
- Thickening of the blood can result from dehydration, so proper hydration with water is crucial.
- Keeping glucose and lipid levels in check can minimize risks of clot formation.
- Smoking harms blood vessels and facilitates clot formation.
- Eating foods with omega-3 fatty acids (fish, flaxseeds, and walnuts) helps in minimizing inflammation and enhancing circulation.
- In certain individuals, physicians might recommend blood thinners such as aspirin or anticoagulants.
Ignoring to symptoms of thick blood may result in more dangerous complications. It is critical to detect them early with routine check-ups and blood work, especially for patients with diabetes, cardiovascular disease, or a family history of blood clotting diseases.
If you suspect that you have thick blood or have clotting-related symptoms, see your doctor right away. Early detection and treatment will avert fatal disorders like stroke, heart attack, and deep vein thrombosis.
What Is The Difference Between Life Expectancy And Healthy Life Expectancy?

‘How long do you think you will live?’, ‘Me? I’ll live till I’m 100 years old!’ As kids these answers were acceptable, full of life and energy, we believed that living till we are 100 was something that can be done. But as we age, we realize, not only is it a pipedream, but life stressors like food, cost of living and how healthy we actually are, can make 100 years sound like hell. Living a long life, like 80 or 70 years old is seen as a reasonable, achievable dream in comparison.
However, the reality of it is much more different than that. You are not being given a choice for a long life, you are paying for a long life with your health. So, if you were to be given a choice, it would be more like, live a perfectly healthy life till 50 or live a long life at the cost of it.
So, when we focus on our health, what should we aim for, long-term healthy years or longer years lived?
What is The Difference Between Life Expectancy And Healthy Life Expectancy?
According to the Royal Borough of Greenwich UK, Life Expectancy (at birth) is the average number of years a person is expected to live in a specific area, based on current death rates. It's a key statistic used to understand the overall health and well-being of a population.
The Life Expectancy gap measures the difference in this number. It can compare life expectancy between men and women or between different geographical areas, like towns or neighborhoods.
On the other hand, Healthy Life Expectancy (at birth) is a more specific measurement. It's the average number of years a person is expected to live in good health, without illness or disability, based on current health and death rates in a particular area.
Have We Been Living Healthier Or Longer?
According to Gov UK, Since the early 2000s, life expectancy has increased more than healthy life expectancy. This means the number of years people spend in poor health has also slightly increased. For example, men now live about 16.1 years in poor health, and women live about 19 years in poor health.
While women still live longer than men, the gap is getting smaller. The difference is now only 3.6 years. However, most of those extra years for women are spent in poor health. Women live 3.6 years longer than men, but they only have 0.7 years more in good health.
Do Older Adults Have Less Healthy Life Expectancy?
The same trend applies to people over 65. They are living longer, but they are also spending more of their later years in poor health. For instance, a 65-year-old man can expect to live an additional 18.8 years, but 8.2 of those years may be in poor health. For a 65-year-old woman, the numbers are 21.2 and 9.9 years, respectively.
This shows that while we're beating old age, we're not always beating the illnesses that come with it. The data suggests we are spending a smaller percentage of our early lives in poor health, but a larger percentage of our later years.
Can We Increase Our Healthy Life Expectancy?
According to the National Institute of Health, genes account for less than a third of your chance of living to age 85. The biggest factor is your behavior and lifestyle. By making healthy choices, most people have the potential to live to a very old age.
Living a healthy lifestyle has a huge impact on your well-being, especially as you get older. A long-term study of a religious group known for healthy living found that they live nearly 10 years longer on average than most Americans. Their secrets? Regular exercise, a vegetarian diet, avoiding tobacco and alcohol, and maintaining a healthy weight.
Experts agree that if you could only do one thing to live longer and healthier, it would be to exercise. Physical activity is crucial for staying active and avoiding disease and disability. Even small amounts of physical activity can help older adults. A study of adults aged 70 to 89 found that those who followed a moderate exercise program had fewer disabilities and recovered faster. A mix of walking, strength training, and balance exercises is especially effective.
Be skeptical of "anti-aging" products or quick fixes. The best and most proven path to a long and healthy life is through common sense habits and an active, engaged lifestyle.
Why Do I Keep Having Stressful Dreams About School? What Do These Recurring Dreams Mean?

It's a simple Monday morning, the sun’s up bright and early, the weather is pleasant, but the anxiety strikes me as soon as I open my eyes. It's the dreaded 10th grade Math exam, the one subject I never excelled at. As if it wasn’t enough that the exam could make or break whether I get enough overall grade to get into my dream schools, if I were to get a bad score on this, it would be a permanent mark on my record.
“I had studied enough, I can do this” I told myself, but what was the point my admit card was nowhere to be found. I searched high and low, my anxiety peaking with every passing minute. “I thought I got up in time? Why am I late, they’ll never let me into the exam hall” I could hear my heartbeat in my ears and it’s getting louder, louder and louder, until it's just a loud long noise. Next thing I know, I’m on my bed, I graduated 10th grade years ago and this was a dream.
What Do Stressful Dreams About School Say About You?
If it isn’t your school exam, then maybe your college entrance exam or perhaps a qualifying exam that could determine whether you get your dream job or not. Recurring dreams about school happen to a lot of us.
These dreams are very common. Experts suggest that they often appear when a person is feeling anxious in their waking life, especially about being evaluated or judged by a boss or another authority figure. These dreams can take many forms: a person might oversleep for an exam, be unable to find their classroom, study the wrong subject, or even show up to school without clothes. The dreams revisit a place where we first experienced success or failure based on our performance.
To understand this, one must know that dreams are a way for the mind to process memories and experiences, both conscious and unconscious. The school setting in these dreams is a stand-in for a feeling of being tested in life and worrying about not meeting other people’s expectations.
Why School is the Go-To Setting
The reason school so often appears as the setting for these anxiety dreams is because it’s where we first learn how to deal with life. Feelings of stress, inadequacy, and embarrassment often happen first in a school environment. These early experiences create foundational beliefs in our unconscious mind about how we handle pressure. For some people, these beliefs can be very hard to change, causing feelings of stress and worry to resurface years later in dreams, even if the beliefs aren't relevant to their adult life.
What Do Recurring Dreams Reveal About Us?
According to the Sleep Foundation, having a recurring dream—the same dream happening again and again—is a sign of an unresolved problem or a difficult emotion in a person’s life. These dreams may be a way for the mind to make sense of past experiences, or they might be a sort of practice run to help a person prepare for a threat or challenge they're facing in real life. The dreams are often a way for the mind to push a person to finally face and deal with a problem.
Another reason for a recurring dream is that it represents a basic psychological need that isn't being met. Experts say everyone needs to feel independent, feel capable, and feel connected to others. Some research has found that people who lack these feelings are more likely to have recurring nightmares with negative themes, such as failing, falling, or being attacked.
Can You Stop Recurring Dreams?
If you're bothered by having the same dream over and over, you can take some steps to try and make them stop. Experts recommend a few different approaches
- Address the root problem. If you can figure out what emotional problems or difficult feelings are causing your dreams, working through them may help the dreams stop.
- Consider therapy. A specific type of therapy called imagery rehearsal therapy is often recommended. With a therapist's guidance, you can practice reimagining the dream with a more positive ending.
- Reduce stress. Since negative recurring dreams are often linked to stress, finding ways to lower your stress levels may also help reduce the dreams.
- Prioritize mental health. People with mental health conditions like depression often have more negative recurring dreams. Treating these conditions can help reduce the frequency of bad dreams.
- Adopt healthy sleep habits. To get a better night's sleep, try to go to bed and wake up at the same time every day. It’s also a good idea to avoid caffeine, alcohol, nicotine, and fatty foods close to bedtime.
- Talk to your doctor about your medications. Some medications, including melatonin, can cause nightmares. Your doctor can advise you on whether changing the dose or stopping the medication might help.
- Treat sleep disorders. If you have a condition like insomnia or sleep apnea, getting treatment for it could help reduce how often you have negative recurring dreams.
Diagnostic Anomaly: Rare Condition Makes This Teen Remembers Everything: She Has Access To Memories That Many Others Don't

At least once in our lives, most of us have dreamed of having a perfect memory. A brain that would remember crucial details at the nick of time, whether it is during your exam or an interview. But this is not just a dream, it is just another day for this young girl, who has a ‘Super Brain’.
Scientifically speaking, she has a very rare condition that makes her remember every detail of her life, like a record. In a 2024 interview by Official W5, Emily Nash, who was 18-year-old at the time of filming, from Ottawa, described her incredible ability to remember everything.
A Person Who Remembers Everything
The video explained how she is one of the few people in the world confirmed to have Highly Superior Autobiographical Memory (HSAM) She can remember the exact date and details of public events, from the death of Queen Elizabeth to celebrity news and movie release dates. Her memory is so precise that she can tell you what she was doing on a specific date, down to what she had for lunch and what was playing on the radio.
Her family even gave her the nickname "Wikipedia" because she was their go-to source for random facts and dates. Emily describes her memory as a "calendar" where each day is like a little movie she can rewind and fast-forward through.
How Is HSAM Different From Having Good Memory?
According to a 2024 study by Neuropsychology Review, HSAM is a very rare and special ability where a person can remember almost every single day of their life in incredible detail. If you give them a specific date, like "January 15, 2003," they can instantly recall what they were doing, what the weather was like, and even what they were wearing. Unlike memory athletes who use tricks to memorize things, people with HSAM do this automatically and without any effort. It feels like a movie playing in their mind. The review confirmed that HSAM is a truly unique type of memory.
It's Fast and Accurate
People with HSAM can recall memories quickly, with amazing detail, and the memories are almost always perfectly accurate.
It Doesn't Fade with Age
A person with HSAM who was studied at ages 75 and 80 still had an incredible memory, showing that this ability seems to resist the normal memory loss that comes with getting older.
It's Only for Personal Memories
The study found that people with HSAM are not better at remembering just anything. They are not smarter, and their memory for general facts, names, or things they learned in a textbook is normal—only their memory for their own life is special.
How Do People With HSAM Remember Everything?
The study explained what goes on inside the brains of people with HSAM.
Brain Activity
When people with HSAM recall a memory, their brain activity goes into overdrive. Areas that are normally used for memory light up much more intensely. This suggests that their memories are more vivid and that the brain's "memory network" is working at a much higher level.
Brain Structure
Interestingly, the physical structure of their brains doesn't appear to be bigger or different in size. Instead, the main difference is in the way certain brain regions are connected, particularly the hippocampus, which is a key part of the brain for memory. This suggests that the special memory isn't because of a bigger brain but because the brain's connections are wired differently.
How Does Researching HSAM Help Brain Health?
Understanding HSAM could be incredibly important for the future. By figuring out how these rare individuals remember so well, scientists might be able to develop new strategies to help people with memory problems, such as those caused by diseases like Alzheimer's. It could also help improve the accuracy of eyewitness testimony in legal cases. Ultimately, this research gives us a unique window into how memory works and how it might be strengthened.
© 2024 Bennett, Coleman & Company Limited

