- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Your Cholesterol Levels Could Predict Alzheimer’s Risk And Why the Wrong Meds Could Make It Worse

Researchers might have discovered a unexpected ally in the battle against Alzheimer's disease—spearheading cholesterol-reducing medications. Recent studies indicate that medications such as statins, which have been prescribed over many years to forestall heart attacks and strokes, might also confer significant protection against mental decline.
A paper in the Journal of Neurology, Neurosurgery and Psychiatry has found that those with low levels of "bad" cholesterol (LDL-C) not only have fewer cardiac risks but also have a significantly lower risk of dementia, including Alzheimer's disease. The presence of statins in those with low LDL-C levels further increased this benefit.
These results, coupled with corroborating evidence from U.S.-based scientists, pave the way to rethink how we keep cardiovascular health in line—now with consideration of the brain.
How Cholesterol Affects Brain Health?
Statins are among the most prescribed medications worldwide, with 7–8 million individuals in the UK alone taking them to avoid cardiovascular events. The drugs act by lowering low-density lipoprotein (LDL) cholesterol, the so-called "bad cholesterol," which can block arteries and lead to heart attacks and strokes.
A more in-depth look at population-level health information from South Korea, on over 570,000 people, added a fascinating new twist: the lowest LDL-C group—below 1.8 mmol/L—were 26% less likely to have dementia and 28% less likely to have Alzheimer's than the group with LDL-C of more than 3.4 mmol/L.
Additionally, statin users with low levels of LDL-C had a further 13% lower risk of dementia and 12% lower risk of Alzheimer's than non-users.
"These results highlight the significance of LDL-C management not only in preventing heart disease but as a key component of an anticipatory approach to neurodegenerative disease prevention," researchers stated in their study. "Targeted statin prescriptions that aim at optimal levels of LDL-C could maximize cardiovascular as well as cognitive benefit."
Relationship Between Brain Function and Blood Lipids
Yet another study, this one from the Glenn Biggs Institute for Alzheimer's and Neurodegenerative Diseases at UT Health San Antonio, supports the notion that the relationship between brain and cholesterol is real—but not necessarily simple.
Dr. Sokratis Charisis, a neurologist and senior researcher, examined data from the landmark Framingham Heart Study and reaffirmed that high levels of LDL are causally linked with cardiovascular disease and dementia.
Though, the information pulled a surprise in regard to HDL—often called "good cholesterol." Long hailed for its cardio-protective qualities, low levels of HDL were found to be associated with a decreased risk of Alzheimer's disease, indicating a more nuanced biological interaction between cholesterol subtypes and cognitive impairment.
"It speaks to the fact that this relationship may not be as straightforward as we believe," said Dr. Charisis. "There may be completely different mechanisms linking blood lipids to brain health as opposed to cardiovascular health."
What Really Affects Alzheimer's Risk?
Charisis also pointed out a third lipid marker—ApoB48, a lipoprotein that carries dietary fats in the blood. Though not usually tested as part of regular cholesterol checks, higher levels of ApoB48 were associated with a reduced risk of Alzheimer's, suggesting unforeseen levels of biological interplay between the diet, lipid metabolism, and brain deterioration.
"This finding is especially noteworthy," said Charisis, "because it potentially could be used to help identify a new biomarker that can ultimately inform predictive diagnostics and personalized treatment strategies."
The significance of this developing research is immense. As of 2019, an estimated 57.4 million individuals globally were affected by dementia, a figure that is predicted to increase more than twice over—that is, 152 million by the year 2050, according to international health organizations.
As Alzheimer's disease is responsible for most cases of dementia and there is no cure yet, prevention and early treatment are more essential than ever. Changes in lifestyle, reduction of cardiovascular risk, and now control of lipids could be the cornerstones of a multi-faceted approach to neurodegeneration.
While statins have traditionally been seen from the perspective of heart health, this new evidence indicates they might also be repurposed or more targeted in their prescribing for brain health, particularly among aging adults.
Yet the results also highlight the importance of individualization. What is good for one brain may not be equally useful for another, especially when age and cholesterol levels are considered. "Perhaps it will be crucial to have dynamic cholesterol targets depending on the patient's age, health status, and genetic profile," Charisis said.
This opens up the possibility of more individualized treatment regimens—not only prescribing statins by cardiac risk, but also including cognitive health evaluations in the decision-making process.
For the time being, specialists continue to recommend regular monitoring of cholesterol levels and early treatment of cardiovascular risk factors. Although you shouldn't start statin therapy just to minimize dementia risk without a doctor's advice, having a healthy LDL-C value is a definite boon to both heart and brain.
Individuals worried about cognitive impairment—particularly those with a family history of Alzheimer's—are advised to:
- Monitor their lipid profiles on a regular basis
- Consult with a healthcare provider regarding cholesterol-lowering therapies
Adopt habits of lifestyle that foster both cardiovascular and cognitive health: exercise, a Mediterranean diet, managing stress, and sleep
The Hidden Glaucoma Warning Signs Every Middle-Aged Adult Should Know
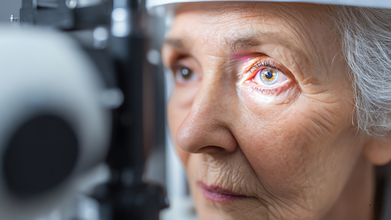
Credit: Canva
Glaucoma is an umbrella term for a group of eye diseases that create pressure inside your eyeball, which can damage delicate, critical parts at the back of your eye, including the optic nerve.
While most of the diseases are progressive, meaning they gradually get worse and eventually cause permanent vision loss and blindness. In fact, glaucoma is the second-leading cause of blindness worldwide and is the leading cause of blindness for people over 60 years old.
Dr Niteen Dedhia, Medical Director, Ojas Maxivision Eye Hospital tells Business Standard: "Glaucoma slowly and quietly causes damage to the optic nerve. Changes in eye pressure, blood flow and nerve fibres occur over time, while the brain often compensates for the loss.
"As a result, symptoms go unnoticed, and by the time vision loss becomes apparent, the damage is usually permanent."
Many forms of glaucoma have no warning signs and the effect is extremely gradual, to the point that you may not notice a change in vision until the condition is in its late stages.
Here are some symptoms that mid-age people need to keep an eye out for:
1. Gradual loss of circumferential vision
One of the earliest symptoms of glaucoma is damage and subsequent loss of peripheral vision. Dr Dedhia noted: “Glaucoma starts by damaging the peripheral vision but doesn’t affect the centre (front) vision."
If you seem to struggle with spotting objects approaching from the side or bump into things more often, you may be experiencing early stages of the disease and not merely experiencing normal ageing.
2. Difficulty seeing or reading in the dark or low light settings
Difficulty adjusting to darkness, discomfort in dimly lit spaces or having trouble navigating at night can be early warning signs may point to reduced contrast sensitivity linked to glaucoma rather than simple eye strain.3. Frequent changes in eye power
Dr Neeraj Sanduja, Ophthalmologist, Eye Surgeon at Viaan Eye Centre, Gurgaon told the publication: "Needing frequent prescription changes or feeling that glasses 'never feel quite right' may reflect subtle visual field changes caused by glaucoma rather than simple refractive error progression."
4. Eye pressure or unusual discomfort
Open-angle glaucoma, the most common form of the condition that causes patchy blind spots in your side vision, is often painless or limited to a mild sense of pressure or heaviness in the eyes.
Those suffering from open-angle glaucoma may notice a dull ache after prolonged screen time or reading that improves with rest. Frequently mistaken as regular eye strain, it is often ignored, however, may indicate subtle increases in eye pressure that require professional evaluation.
5. Frequent headaches with eye strain
Frequent headaches, especially when accompanied by eye strain or blurred vision, should not be ignored as migraine pain as it may signal rising eye pressure or early glaucoma changes, Dr Dedhia warns.
Who Is at Risk for Glaucoma?
Certain groups of people have a higher than normal risk of getting glaucoma which includes those who:
- have high eye pressure
- are farsighted or nearsighted
- have had an eye injury
- use long-term steroid medications
- have corneas that are thin in the center
- have thinning of the optic nerve
- have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body
- are over age 40
- have family members with glaucoma
- are of African, Hispanic, or Asian heritage
Sleeping Too Much or Too Little Raises Liver Disease Risk, Study Finds

Credit: Canva
Abnormal sleeping patterns, whether excessive or brief, can significantly increase your risk of developing chronic liver disease, an EMJ study suggests.
Sleep duration has previously been linked to worsening your chances of Type 2 diabetes; obesity; cardiovascular diseases including hypertension, stroke, heart attack; mental disorders such as depression, anxiety; weakened immune system and potentially contributing to neurological conditions such as dementia.
However, researchers have now also found that sleep disruption may intensify existing stress on the liver which can worsen metabolism and pave the way for disease progression.
The authors noted that poor sleeping habits may influence liver health for multiple reasons including by altering glucose metabolism, increasing inflammation and disrupt circadian rhythms that regulate liver function.
"Participants who reported consistently short sleep duration were more likely to have elevated liver enzymes and higher fibrosis risk scores compared with those reporting moderate sleep duration. Long sleep duration was also associated with adverse liver markers, though the relationship was weaker than that observed for short sleep," the study noted.
Despite discovering links, the involved researchers noted that the study only highlighted sleep as a potential factor that could worsen liver function along with other lifestyle reasons and did not act as a clear cause.
Why Is Chronic Liver Disease A Concern?
Once a rare condition, non-alcoholic fatty liver disease (NAFLD) now affects one in three Indians. A JAMA study has now found that about 40 percent of the global population is now suffering from NAFLD, with abdominal obesity identified as its single biggest risk factor.
Researchers found that nearly 70 percent of people with Type 2 diabetes and about 80 percent of those with obesity are affected by NAFLD. They also discovered that NAFLD prevalence is higher in men than in women, with rates of 15,731 per 100,000 population in men compared with 14,310 in women.
READ MORE: This Deadly Liver Disease Is Affecting People In Their 20s And This One Symptom Is The Red Flag
Between 2010 and 2021, India recorded a 13.2 percent increase in age-standardized prevalence, ranking just behind China at 16.9 percent and Sudan at 13.3 percent. Additionally, the disease peaks earlier in men, between 45 and 49 years of age, while women show the highest prevalence between 50 and 54 years.
NAFLD, now called as metabolic dysfunction-associated steatotic liver disease (MASLD), is when excess fat builds up in the liver, unrelated to heavy alcohol use, due to obesity, Type 2 diabetes, high blood pressure and cholesterol.
It ranges from simple fat accumulation to inflammation and damage, which can progress to fibrosis, cirrhosis or liver cancer, The disease often has no symptoms and is managed with lifestyle changes such as diet and weight loss.
Why Is NAFLD on the rise?
Poor diets (high carbs/sugar), sedentary habits and rising obesity are some of the key reasons why an uptick in NAFLD cases has been seen pan-India. Increased intake of refined carbs, sugary drinks, processed foods and unhealthy fats can increase the risk of obesity, diabetes, hypertension and high cholesterol which can pave the way for this liver disease.
Experts also note that working long hours at desks without any proper physical activity can lead to weight gain and fat accumulation in the liver.
According to the Union Health Ministry, the prevalence of the condition could be in the range of 9-53 percent. Multiple other health studies also suggest nearly 40 percent of urban Indians may have some form of fatty liver disease
Hepatologist Dr Cyriac Abby Philips, popularly known as LiverDoc on social media, noted on X that many patients do not realize that timely lifestyle changes can completely reverse the condition. “All it takes is being in charge of your body and health. No shortcuts—go slow and steady,” he wrote.
If left untreated, NAFLD can progress to Non-Alcoholic Steatohepatitis (NASH), where liver inflammation begins. Over time, this inflammation can lead to scarring of the liver, known as fibrosis. Advanced fibrosis results in cirrhosis, which severely affects liver function.
NAFLD can also increase the risk of chronic liver disease, liver failure and hepatocellular carcinoma. Many patients diagnosed with liver cancer have a history of untreated fatty liver.
Unique Symptoms Of Alzheimer's Disease And How It Can Be Managed
Credits: iStock
Over 2 million Americans have Alzheimer's. It is the most common cause of dementia and is a progressive disease. This means the disease will get worse, however, it could be managed, though cure is not available. It is the biological process that begins with the appearance of a buildup protein in the form of amyloid plaques and neurofibrillary tangles in the brain. This causes brain cells to die over time and the brain to shrink.
What Makes Alzheimer's So Unique?
The fact that there is no cure for Alzheimer's disease is one of the most unique part of the condition. In advanced stages, loss of brain function can cause dehydration, poor nutrition or infection.
The symptoms of Alzheimer's are unique because the signs are easily miss-able. These signs could seem like a day to day problem and not anything serious. At first, it starts with trouble in remembering recent events or conversations. Over time, memory gets worse and other symptoms occur.
While everyone could have trouble with memory at times, the memory loss that happens with Alzheimer's is lasting. The signs could be:
- Repeat statements
- Repeating questions over and over
- Forgetting conversations, appointments and events
- Misplacing items, and putting the in odd places
- Getting lost in places you know very well
- Forgetting names of family members
- Forgetting names of everyday objects
- Have trouble finding the right words, expressing thoughts or having conversations
Unique Symptoms Of Alzheimer's: Cannot Recognize Numbers
Alzheimer's could also lead to trouble in concentrating, thinking, especially about abstract concepts like number. Your thinking and reasoning abilities take a hit. In fact, in many cases, people with Alzheimer's are not able to recognize numbers.
Unique Symptoms Of Alzheimer's: Cannot Perform Everyday Tasks
There are many tasks that you do in your day to day life, which come easy to you, could become difficult over time. As Alzheimer's advances, people forget how to do basic tasks such as dressing or bathing.
Read: What A Finger-Prick Blood Test Could Mean for Alzheimer’s Diagnosis
Your Personality Changes
With Alzheimer's, your personality too can change, as the disease could affect moods and behaviors. Symptoms include:
- Depression.
- Loss of interest in activities.
- Social withdrawal.
- Mood swings.
- Not trusting others.
- Anger or aggression.
- Changes in sleeping habits.
- Wandering.
- Loss of inhibitions.
- Delusions, such as believing something has been stolen when it hasn't.
Are There Any Treatments Or Cures?
UK researchers say fruit flies could help unlock why devastating brain and nerve conditions such as Alzheimer’s, Parkinson’s and motor neurone disease develop, despite decades of medical research. Scientists have known for years that many neurodegenerative disorders are linked to genetic mutations. What has remained unclear is how those mutations actually trigger disease inside the nervous system.
According to the Mirror, new findings published in the journal Current Biology suggest a breakthrough may lie in studying fruit flies, insects whose genes behave in strikingly similar ways to those in humans.
© 2024 Bennett, Coleman & Company Limited

