- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Your Chronic Health Struggles Could Be Doubling Your Risk Of Depression- Here’s What To Know

Credits: Canva
Living with a chronic illness can be like fighting an uphill battle—physically, mentally, and emotionally. But new research indicates the cost may be even deeper than most people know: long-term physical illness may dramatically raise your risk of developing depression.
As a revolutionary study in Nature Communications Medicine explains, individuals with many chronic conditions are much more likely to experience a mental health breakdown. This finding explains the essential, but frequently overlooked, connection between body and mind.
Traditionally, healthcare systems everywhere have addressed physical and mental illness as separate silos. But new science is presenting a different picture—one where body and mind are highly intertwined.
In the recent U.K. Biobank study, researchers followed over 142,000 adults aged between 37 and 73, all of whom had at least one chronic illness but no prior diagnosis of depression. The findings were eye-opening: individuals with multiple physical conditions were up to 2.4 times more likely to be diagnosed with depression over the next decade compared to those without chronic illnesses.
The report's co-author, Professor Bruce Guthrie from the University of Edinburgh, underscored the significance: "Healthcare tends to think of physical and mental ill health as two totally separate things, but this research indicates that we must do better at predicting and treating depression in individuals who have physical illness."
Which Conditions Have the Highest Risk?
While any long-term illness will erode mental toughness, some combinations greatly increase depression risk. Among the study's most surprising findings:
Individuals with migraine illness or chronic respiratory disease had twice the risk of depression.
A combination of heart disease and diabetes raised depression risk by almost 78%.
Gastrointestinal illnesses such as IBS, celiac disease, and liver disease were associated with an 83% increased risk of depression in women and a twofold increase in risk in men.
These figures are more than just statistics—they represent real individuals facing a double burden of illness and emotional distress. And with 1 in 12 people in high-risk groups developing depression over a decade (compared to 1 in 25 among those without chronic conditions), the data calls for urgent attention.
Why Is Depression Always More Than Just Feeling Sad?
In order to comprehend why this is important, it's necessary to know what depression actually is. Clinical depression, also known as major depressive disorder, is a mood disorder that extends far beyond fleeting sadness. It's a complex illness that influences the way individuals think, feel, and behave. Symptoms can involve:
- Constantly feeling sad or hopeless
- Loss of interest in activities once enjoyed
- Fatigue or loss of energy
- Trouble concentrating or making decisions
- Changes in appetite or sleep habits
- Physical symptoms like sudden pain
- Integers of suicide or harming oneself
Depression is not a personal failing or something you can simply "snap out of." It is a genuine medical illness that more often than not needs to be treated by professionals—such as therapy, medication, or both.
Biological and Emotional Roots of Depression in Chronic Illness
Why chronic illness would so greatly increase the risk of depression? Experts consider the causes to be multifactorial.
Physiologically, certain chronic diseases interfere with brain chemistry or hormonal equilibrium, both of which play a critical role in regulating mood. Such conditions as thyroid disease or diabetes, for example, can have a direct effect on neurotransmitters associated with depression.
Emotionally, the ongoing juggling act of pain, tiredness, and doctor visits can be draining. Throw in social isolation, financial burden, or loss of autonomy, and it is not hard to understand how emotional well-being can start to fray.
When to Seek Help?
If you or someone close to you is living with a chronic illness, it is important to remain aware of depression symptoms. Early treatment makes a real difference in the outcome of care and the quality of life.
Do not wait until things get worse. If you see signs such as lingering unhappiness, loss of initiative, or constant exhaustion, seek professional attention. A visit to a primary care doctor or mental health expert can be an important first step.
This new research supports what many patients have long intuited—real wellness can't be realized without attending to body and mind. It's high time for medical providers, policymakers, and insurers to adopt a more integrated strategy for the management of chronic disease that encompasses preventive screening and treatment for mental illness.
Lead researcher Lauren DeLong said it best: "We noticed obvious links between physical health conditions and the occurrence of depression, but this research is just the start. We hope our research will encourage other scientists to explore and disentangle the connections between physical and mental health conditions."
Gamer’s Neck Develops 'Dropped Head Syndrome' After Years Of Looking At His Phone, Doctors Warn Of Debilitating Condition
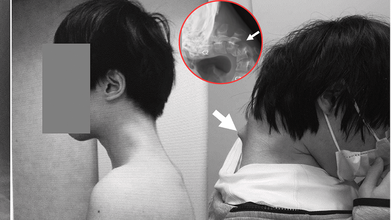
Credits: JOS Case Reports
When was the last time you caught yourself hunched over your phone, neck bent at an unnatural angle? A few minutes scrolling might feel harmless, but for one 25-year-old gamer in Japan, years of that posture ended with a shocking diagnosis, “dropped head syndrome.” His story has left doctors urging young people worldwide to rethink how long they spend staring down at their screens.
In a striking case that has unsettled health experts, Japanese doctors documented how a 25-year-old man grew a serious case of "dropped head syndrome" after years of crouching over his smartphone playing video games. The debilitating but unusual condition left him unable to lift his head, properly swallow food, or sustain a healthy weight.
In the case report released in JOS Case Reports in 2023, the patient's battle started following years of isolation from society in his teenage years. Having endured constant bullying at school, he isolated himself in his bedroom and spent many hours glued to his phone playing games, with his head leaning forward at steep angles for hours on end.
How Smartphone Overuse Weakened His Neck?
The injury was chronic. For six months, the man suffered from excruciating neck pain before he lost all ability to lift his head. His vertebrae deformed and dislocated over time, scar tissue in his spine formed, and he had trouble swallowing, leading to spectacular weight loss.
Scans established that his cervical spine had been subjected to extreme stress through unnatural posture over many years. The muscles and ligaments that were meant to keep the head upright no longer worked, and his chin would sag onto his chest.
The doctors first tried to treat it conservatively using neck collars, but the patient complained of numbness and pain, compelling the team to embark on surgery.
How Did The Doctors Treat 'Dropped Head Syndrome'?
Surgeons carried out an intricate procedure that entailed removing bruised bits of vertebrae and scar tissue, followed by the implantation of metal rods and screws to stabilize and realign the spinal posture. Six months passed before the patient regained the ability to keep his head level.
At one-year follow-up, swallowing problems had cleared up, posture was stable, and quality of life had dramatically improved.
The group concluded that the condition was caused by an "underlying developmental disorder" but that the long-term consequences of prolonged smartphone use with this posture were the biggest contributor to his illness.
What Is Dropped Head Syndrome?
Dropped head syndrome (DHS), also referred to as "floppy head syndrome," is an uncommon disorder that involves, at times severe, weakness of the neck muscles, resulting in a "chin-on-chest" posture.
It is most commonly linked to neuromuscular disorders like amyotrophic lateral sclerosis (ALS), Parkinson's disease, or specific muscular dystrophies. The patients tend to use their hands to support their heads and can have difficulties with eating, talking, and walking.
In ALS, DHS happens in approximately 1–3% of the patients and is typically progressive with a grim prognosis. But as this Japanese case suggests, DHS may also arise due to non-neurological etiologies such as trauma, drug abuse, or—as in this instance—chronic mechanical stress of posture.
Can Screen Time Be Associated With Dangerous Conditions?
Although this instance is unusual, physicians caution it shows an expanding medical danger associated with mobile phone addiction. Over 6.8 billion individuals across the globe currently have access to smartphones, with four to seven hours of average screen time per day. Among game players and youth, use can be much higher.
Protracted downward neck posture—a sometimes termed "tech neck"—is already associated with headache, eye strain, and degeneration of the cervical spine. This is the extreme example of DHS and serves to illustrate how serious the effects can be when posture is neglected.
How Does Dropped Head Syndrome Affect Everyday Life?
DHS is more than just an inconvenient posture. The deformity affects simple functions such as swallowing, speaking, and breathing. It inhibits mobility, renders everyday activities challenging, and results in social withdrawal and isolation. In younger individuals, it even generates a chain of physical disability that multiplies mental health issues.
In this patient's life, bullying during childhood and later ostracism provided fertile ground for technological dependence. His case is particular about pointing to the juncture of mental well-being, online tendencies, and bodily well-being—a synergistic combination that is all the more pertinent in contemporary societies.
Organizations like the American Academy of Orthopaedic Surgeons have already warned of increasing incidence of posture-related spinal disorders in young people. The majority will never suffer from DHS, yet milder but chronic neck and back ailments are sweeping up teenagers and young adults.
Elizabeth Jarman from Médecins Sans Frontières, citing parallel access problems with diabetes care, emphasized that the first step to prevention is awareness. In the case of digital health, professionals are calling for schools, workplaces, and families to include posture education and frequent movement as part of daily practice.
Can Dropped Head Syndrome Be Prevented?
Prevention of dropped head syndrome due to posture is easy in principle:
- Avoid repetitive forward flexion of the neck.
- Take frequent breaks from screen time.
- Do neck-strengthening and posture-improving exercises.
- Employ ergonomically arranged seating and screen configurations.
But putting these measures into practice takes awareness and discipline—two qualities usually lacking in the fast-engagement era of mobile gaming and social media.
Is Surgery the Only Option for DHS Treatment?
For cases as bad as the Japanese gamer's, surgery is still the only real option. Surgical procedures are not without hazard, though, from infection to nerve damage. Even if successful, recovery is long and needs rigorous rehabilitation.
Due to the relative infrequency of DHS, there is no gold standard for surgical treatment. Each case has to be assessed on its merits, weighing risks against benefits.
This is an extreme case, but it is one that should serve as a warning to young people everywhere. The frequency of "tech neck" complaints in clinics, alongside rising screen time, indicates there could be more cases of spinal deformities emerging if awareness is not given high priority.
As the Japanese physicians who attended to the gamer stressed, the illness might have been precipitated by the integration of physical posture and pre-existing susceptibilities, but excessive use of smartphones in uncomfortable positions may produce unimaginably tragic results.
Brain’s ‘Clean Sweep’ Could Help You Lower Your Risk Of Dementia

(Credit-Canva)
Our body is like a self-maintaining machine, it is equipped to help us heal ourselves, recharge after a long day’s work as well as having its own warning system to ensure places that need help come to notice, i.e., pain. However, did you know your brain could also actively be stopping you from developing mental health conditions? Yes, your brain and body are not as defenseless as you may think it to be, with the help of sleep, your brain is actively keeping you from developing certain issues.
The brain has a unique way of getting rid of waste, almost like a personal cleanup crew. This process, called the glymphatic system, is thought to work best while we're sleeping. But what happens if our sleep is disrupted?
Researchers believe that a lack of good sleep might stop this system from working correctly, leading to a build-up of waste or toxins in the brain. Some are suggesting this buildup could increase a person's risk of developing dementia.
How the Brain Clears Out Waste
Every cell in your body creates waste, and outside the brain, a system called the lymphatic system takes care of it. But the brain doesn't have these vessels, so how does it stay clean?
About 12 years ago, scientists discovered the glymphatic system. It uses a fluid that surrounds your brain and spinal cord, called cerebrospinal fluid, to "flush out" toxins. This fluid flows through the brain, collects waste, and then drains it away.
Waste products
According to the National Institute of Health one key waste product is a protein called amyloid beta (Aβ). When Aβ builds up, it can form plaques in the brain. These plaques, along with other protein tangles, are a clear sign of Alzheimer's disease, the most common type of dementia.
Sleep and waste
Studies in both humans and mice have shown that Aβ levels increase when you're awake and then drop quickly while you sleep, like the 2018 study published in the Annals of neurology.. This supports the idea that the brain is more actively "cleaning" during sleep.
How Is Sleep Connected To Dementia?
If sleep helps clear toxins, what does long-term disrupted sleep, like that from a sleep disorder, mean for your brain's health?
Sleep Apnea
This common condition causes a person's breathing to stop and start repeatedly during the night. This can lead to a long-term lack of sleep and reduced oxygen, both of which may cause toxins to build up in the brain. Studies have linked sleep apnea to a higher risk of dementia, and some research shows that treating sleep apnea helps clear more Aβ from the brain.
Insomnia
Having trouble falling or staying asleep over a long period has also been linked to an increased risk of dementia. While these links are promising, scientists are not yet sure if treating these sleep problems directly lowers the risk of dementia by removing toxins from the brain.
Does Sleep Aid Brain Health?
Another study, published in the Nature publication 2024, showed that neurons act like miniature pumps. During sleep, these neurons produce rhythmic bursts of electrical energy that create waves. These waves are not just a sign of a sleeping brain; they actually push fluid through brain tissue, effectively washing away waste.
This discovery helps explain why a good night's sleep is so important for brain health. As Dr. Jonathan Kipnis, the senior author, said, "We knew that sleep is a time when the brain initiates a cleaning process to flush out waste and toxins it accumulates during wakefulness. But we didn’t know how that happens."
The researchers believe the brain might adjust its cleaning method based on the type and amount of waste, similar to how we adjust our hand motions when washing dishes—using big, slow movements for large messes and faster, smaller ones for sticky spots.
Propranolol For Anxiety: Why Are Women Taking Popular Heart Medicine For Panic Attacks

(Credit-Canva)
Panic attacks, anxiety, tremors are common for people to experience, and until recently there was not a sustainable solution for it. However, some women revealed how they use this popular heart medicine, propranolol, to not only reduce these symptoms, but to also ensure that they perform better in different situations like dates and presentations.
Described by many influencers to be a ‘magic pill’ that helps us calm down their jitters, new data shows a rise in the number of prescriptions for propranolol. However, is it safe? And what are the health implications of using the same?
How Beta-Blockers Like Propranolol Work
According to Cedar Sinai experts, when you face a stressful situation, your body goes into "fight-or-flight" mode. This response is triggered by stress hormones like adrenaline and noradrenaline, which make your heart beat faster and your blood pressure rise. Doctors explain that beta-blockers interrupt this process. They prevent those stress hormones from causing those physical reactions.
- Selective beta-blockers mainly affect your heart.
- Nonselective beta-blockers, on the other hand, have a broader effect, including on the brain.
Experts note that for anxiety-related issues like panic attacks or performance anxiety, nonselective beta-blockers can "turn down the volume" on your body's stress response. This allows you to think more clearly and cope better.
Propranolol For Anxiety: Does It Help?
Doctors often prescribe a nonselective beta-blocker called propranolol to help with anxiety, panic attacks, and PTSD. It's usually taken as needed for specific stressful situations, not for daily use.
One of its benefits is that it works quickly—in about 20 to 30 minutes—without causing sleepiness or brain fog, which is a common side effect of other fast-acting anxiety medications.
Doctors explained that many patients are more open to trying propranolol because it's typically known as a heart medication, which helps remove the stigma some people feel about taking "psych meds."
Propranolol for Migraines: Does It Help?
According to the National Library of Medicine, Beta-blockers are a common and effective type of medicine used to prevent migraines. The most frequently used one is propranolol.
Treatment with propranolol typically starts at a low dose of 40 mg per day. This can be gradually increased up to 320 mg daily, if needed. It's important to be patient, as it can take up to 12 weeks at the right dose before you notice the full benefits of the medication.
Is Propranolol Safe for Pregnant Women?
The role of propranolol in pregnancy has been an important conversation. Some important notes about propranolol and pregnancy that were addressed in the MothertoBaby medical journal are
Getting Pregnant
It is not known if propranolol makes it harder to get pregnant. It can, however, cause erectile dysfunction in men, which could make conception difficult.
Miscarriage
There have been no studies to see if propranolol increases the risk of miscarriage.
Birth Defects
Every pregnancy has a 3-5% chance of birth defects. It is not known if propranolol increases this risk. However, studies on beta-blockers in general have not shown a higher chance of birth defects.
Other Pregnancy Issues
Some studies have linked propranolol to slower baby growth, but it’s not clear if this is caused by the medicine itself or the health condition being treated. The medication does not appear to increase the risk of other problems like premature birth.
Baby's Health After Birth
If you take propranolol in late pregnancy, your baby might have temporary symptoms like a slow heart rate or low blood sugar. Not all babies will have these symptoms, but it’s crucial to tell your healthcare providers so they can monitor your baby and provide the best care.
Long-Term Effects
No studies have been done to see if propranolol affects a child's learning or behavior later in life.
If you are pregnant or planning to be, it’s important to talk to your doctor before stopping or changing how you take your medication. They can help you weigh the benefits of treating your condition against any potential risks.
© 2024 Bennett, Coleman & Company Limited

