- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
6 Tourists, Including US Citizen, Die from Suspected Methanol Poisoning in Laos, Southeast Asia

After a disturbing event, Southeast Asia, a popular holiday destination for Americans and Canadians, has recently come under scrutiny. Six tourists, including a U.S. national, tragically died from methanol poisoning connected to tainted alcohol, according to recent reports from Laos. This serves as a stark reminder to tourists to use caution when drinking in places with limited regulations.
What is Methanol Poisoning?
Before we move on to the symptoms and prevention, let us first understand what is Methanol. It is a toxic form of alcohol found in industrial products such as paint thinners and antifreeze. It is also sometimes used illegally to produce illegal alcoholic drinks because it’s cheaper than ethanol - the alcohol used in beverages. Methanol is colorless, odorless, and tasteless, which makes it almost impossible to detect its presence in drinks.
Consuming even small amounts of it can be fatal, even half a shot glass can lead to dangerous outcomes. The symptoms may not appear immediately but can include nausea, vomiting, abdominal pain, and breathing difficulties. Left untreated, methanol poisoning can lead to blindness, organ failure, or death.
Why is this a Concern in South East Asia?
South East Asia, particularly countries like Laos, Indonesia, Cambodia, and Vietnam, has long struggled with methanol contamination in illegally sold alcohol. In popular tourist towns such as Vang Vieng in Laos, which is a big on party scene, alcohol served in bars or purchased from street vendors may be mixed with methanol. These drinks can appear to be legitimate branded products, making the risk harder to spot.
How to Protect Yourself
- Avoid unknown or unbranded alcohol and stick to sealed, internationally recognized brands purchased from reputable stores.
- Be cautious of cocktails as mixed drinks may use locally sourced or unregulated spirits.
- Watch for cheap alcohol. If a drink’s price seems too good to be true, better to avoid it.
- Bring your own alcohol if the regulations permit.
- Know the early symptoms - nausea, abdominal pain, and confusion - and seek medical help immediately if you suspect contamination.
What to Do if You Suspect Poisoning
Methanol poisoning requires urgent medical attention. So go to the nearest hospital or clinic immediately. Let the staff know of the possibility of methanol poisoning and contact your country's consulate for assistance in finding appropriate care.
Despite efforts by foreign governments to warn travelers, the issue persists in many South East Asian countries due to limited oversight and widespread use of methanol in counterfeit alcohol production. Awareness is your best defense against this hidden danger.
Go and enjoy the rich culture and beauty of South East Asia, but prioritize your safety by making informed choices about what you drink, you can ensure your travels are memorable for the right reasons.
Salad Dressing Recall: FDA Issues Class II Recall For Salad Dressings And Sauces Over Plastic Contamination

Credits: Canva
Salad Dressing Recall: If you recently bought salad dressing or sauces, it may be time to double-check what’s sitting in your fridge following an important recall. On November 6, the U.S. Food and Drug Administration announced a recall covering thousands of gallons of dressings and condiments made by Ventura Foods LLC. The notice was later upgraded on December 4 to a Class II recall, highlighting the need to remove these products from stores and homes. Here is what consumers should know.
Also Read: The “Triangle of Death” on Your Face: Why You Should Never Pop a Pimple There
Salad Dressing Recall: What Products Are Being Recalled?
The expanded recall affects multiple Ventura Foods LLC products, including the following dressings and sauces:
- Caesar Dressing (Costco Food Court)—32 LB (14.51 kg); SKU: 0 26700 19376 7
- Caesar Dressing (Costco Service Deli)—23.62 LB (10.71 kg); SKU: 0 26700 19376 7
- Creamy Poblano Avocado Ranch Dressing and Dip—1 GAL (3.78L); SKU: 7 34730 53243 1
- Hidden Valley, Buttermilk Ranch—1 GAL (3.79L); SKU: 0 26700 19192 3
- Italian Salad Dressing—1 GAL (3.78L); SKU: 7 67367 00518 4
- Pepper Mill Creamy Caesar Dressing—1 GAL (128 FL OZ) 3.79 L; SKU: 0 93901 78134 5
- Pepper Mill Regal Caesar Dressing—1 GAL (128 FL OZ) 3.79 L; SKU: 0 93901 72607 0
- Publix Deli Carolina-Style Mustard BBQ Sauce—12 LB; SKU: 10 026700 16964 6
- Ventura Caesar Dressing—2000LB (907.1kg); SKU: 00 026700 17360 8
Costco also recalled two ready-to-eat items that used the affected dressing: the Caesar Salad (item number 19927) and the Chicken Sandwich with Caesar Salad (item number 11444). Both products are now past their sell-by dates, which ranged from October 17 to November 9, as per Health.
Salad Dressing Recall: Why Are Salad Dressings Being Recalled?
According to the FDA and Costco, the recalled dressings and sauces may contain pieces of plastic, described as “plastic foreign material,” leading to a voluntary recall. The FDA noted that because many of these products were manufactured in large quantities for food service use, they were likely supplied to delis, cafeterias, and similar facilities. Distribution covered 27 states, including Arkansas, Colorado, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Nebraska, New Hampshire, New Jersey, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, South Carolina, Texas, Virginia, Washington, and Wisconsin.
Salad Dressing Recall: What Does A Class II Recall Mean?
On its website, the FDA explains that a Class II recall is its second most serious category. It refers to situations where using or being exposed to the product could cause temporary or medically reversible health effects, while the chance of severe health consequences is considered low.
Salad Dressing Recall: What Should I Do If I Purchased These Products?
The FDA has not issued detailed guidance for consumers who may have bought the recalled items. As with any recall, the safest step is to avoid consuming the products and contact the retailer for information about returns or refunds. Costco stated in its advisory that customers should stop using the affected items and bring them back to their local Costco location for a full refund.
Billy Connolly Has Been “Incredibly Brave” in His Battle With Parkinson’s Disease, Says Actor Martin Compston
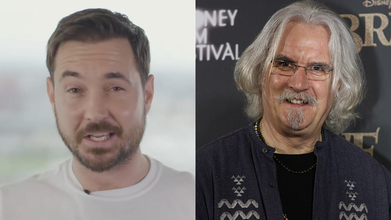
(L) Martin Compston (R) Billy Connolly
Billy Connolly Parkinson's Disease: Martin Compston, Sottish actor and former footballer praised Sir Billy Connolly, actor, comedian and musician, for handling his Parkinson's disease in an "incredibly brave" way.
The 83-year-old comedian was diagnosed in 2013, and five years post that, in 2018, he announced his retirement. Compston who is also co-host of Hoolie In The Hydro, said that the Scottish comedian battled the disease "with a smile on his face and cracking jokes that only Billy can."
Also Read: 8 Red Flags That May Suggest Cancer Growth In Your Body
He said, "Obviously, Billy’s been battling Parkinson’s but he’s been battling incredibly bravely and again he’s done it with a smile on his face and cracking jokes that only Billy can. I’m hoping he’s with us for a long time to come.”
Billy Connolly Health Update
In 2024, Billy made an admission about death amid his ongoing health struggles. In his 2023 autobiography, he mocked the "exaggerated" reports of his "demise". However, the actor-comedian said that he has maintained a positive outlook about his health and that he does not feel "close to death".
In an interview with The Mirror, he said that he remembers the day when he was told he had Parkinson's was the same day he was diagnosed with prostate cancer. "Yes, it was a funny week I had. On the Monday, I had hearing aids. On the Tuesday I got pills for heartburn, which I have to take all the time, and on the Wednesday, I got news that I had prostate cancer and Parkinson’s."
He shared that the best way to deal with such a news is to start thinking about the next step, which is the treatment. "You just have to think. Don't think you are being badly treated [by life] or you have the bad pick of the straws. You are one of millions. Just behave yourself and relax."
Connolly got the all-clear from prostate cancer after receiving treatment, reported the Independent.
Read: Can You Detect Dementia With An Eye Test?
As far as Parkinson's is concerned, his wife, Pamela Stephenson had said that her husband had the "most significant" symptom of the disease, which was a "couple of serious falls" that happened after his balance deteriorated due to Parkinson's.
Talking to Guardian, Billy said, "Recently I've noticed a deterioration in my balance. That was never such a problem before, but in the last year that has come and it has stayed. For some reason, I thought it would go away because a lot of the symptoms have come and gone away."
Prostate Cancer And Parkinson's Disease In Men Aged 40-50
The John Hopkins Medicine recommends screening for prostate cancer at age 55, and start their PSA screening between ages 40 to 54.
What Is Prostate Cancer? Prostate cancer is the most commonly diagnosed cancer in men and the second leading cause of cancer-related deaths in the United States. In many cases, it grows slowly, and detecting or treating it before symptoms appear may not always improve health outcomes or extend life. Learn more about prostate cancer, including screening, prevention, treatment options, research, and key statistics.
The National Institute of Neurological Disorders and Stroke says that while an average age of onset of Parkinson's disease in a person is in early to mid 60s, there could be some people who may have the disease before the age of 50.
Also Read: The “Triangle of Death” on Your Face: Why You Should Never Pop a Pimple There
In fact, a 2019 study in the Journal of Parkinson's Disease notes that while the mortality rate of Parkinson's disease is higher in women, risk of developing it is twice as high in men than women.
What Is Parkinson's Disease? Parkinson’s disease is a slowly progressing disorder that affects movement and the nervous system. It develops when certain nerve cells in the brain weaken, become damaged, or die. As a result, people may experience tremors, stiffness, slowed movement, and balance problems. Over time, these symptoms can make everyday activities like walking, talking, and simple tasks more difficult.
Influenza A: After Three Child Deaths, Health Officials Urge Flu Vaccination in Canada

Credits: Canva
Three children from Ottawa and Eastern Ontario have died due to flu-related complications over the past two weeks, as an unusually early and aggressive flu season grips the region. Health officials have confirmed that the cases are linked to Influenza A, a strain currently circulating widely and affecting children more severely than usual, as per CTV news.
The children were between five and nine years old. Authorities have not released further personal details about the two Ottawa cases and one case from Eastern Ontario.
What Is Influenza A?
Influenza A is a fast-spreading respiratory virus responsible for seasonal flu outbreaks and, at times, global pandemics. It changes quickly through genetic shifts, which makes new strains harder to predict and control. The virus is grouped based on surface proteins called hemagglutinin and neuraminidase, with H1N1 and H3N2 among the most common strains in circulation. It spreads mainly through coughs, sneezes, or close contact and often comes on suddenly, causing fever, cough, body pain, and extreme tiredness. In some cases, it can lead to serious complications, especially in vulnerable groups.
Influenza A: Health Officials Call Deaths a Serious Warning
Public health leaders from Ottawa and Eastern Ontario described the deaths as a troubling reminder of how dangerous the flu can be, especially for children.
“This highlights that influenza is not always a mild illness. It can lead to serious complications that require hospitalization,” medical officers of health from both regions said in a joint statement issued on Monday, as per CTV News.
Influenza A: Child Flu Deaths Rare but Not Unprecedented in Canada
While flu-related deaths among children are uncommon in Canada, they are not unheard of. During the last severe flu season in 2022, two children in Ottawa died due to influenza.
Most flu-related deaths in Canada occur among older adults. Of the estimated 3,500 flu deaths reported nationwide each year, roughly 90 percent involve people over the age of 65. However, experts say the current Influenza A strain is behaving differently.
Influenza A Hitting Children Hard This Season
The strain of Influenza A currently circulating has been linked to a sharp rise in severe pediatric flu cases globally. Health officials say the cluster of three child deaths within such a short period, and within a relatively small geographic area, is highly unusual.
This unusual pattern prompted the regional coroner to alert public health authorities after three sudden, unexpected child deaths tested positive for Influenza A.
“It’s rare for the coroner to reach out like this,” said Dr. Trevor Arnason, Ottawa’s medical officer of health. “But this season has been particularly severe.”
Influenza A: Hospitals Strained as Pediatric Cases Rise
CHEO, Ottawa’s children’s hospital, has reported high numbers of children falling seriously ill with the flu since November. Hospitalizations have continued to rise through early December.
Last week, CHEO issued an urgent request asking family doctors to extend clinic hours and assist at the hospital’s Kids Come First clinic to help manage patient volumes.
Hospital officials have also noted that many children arriving at the emergency department with severe flu symptoms had not been vaccinated.
Influenza A: Strong Push for Flu Vaccination as Cases Surge
Public health officials, including Ontario’s Chief Medical Officer of Health Dr. Kieran Moore, are urging everyone aged six months and older to get vaccinated as soon as possible.
Dr. Arnason and Dr. Paul Roumeliotis, medical officer of health and CEO of the Eastern Ontario Health Unit, stressed that vaccination is especially important for children this season.
Influenza A: Vaccine Still Effective Despite Strain Mutation
Some people have expressed concern after reports suggested this year’s flu vaccine is not a perfect match for the circulating Influenza A strain. Health officials clarified that while the virus has mutated slightly since circulating in the southern hemisphere, the vaccine still offers meaningful protection.
“The flu vaccine may not always prevent infection, but it significantly reduces the risk of severe illness, hospitalization, and complications,” officials said. They added that the vaccine takes about two weeks to become fully effective, making early vaccination crucial ahead of the holiday season, when virus spread typically increases.
© 2024 Bennett, Coleman & Company Limited

