- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Colon Cancer Could Kill 53,000 Americans In 2025, Experts Say The American Diet Is To Blame

Credits: Health and me
Colon cancer is no longer an old person's disease. In a recent turn of events, incidence rates for colorectal and other GI cancers are increasing steadily in Americans under the age of 50, which is concerning scientists, physicians, and public health experts worldwide.
Based on the American Cancer Society, in 2025 about 52,900 Americans are predicted to be killed by colorectal cancer, with a disproportionate number of deaths falling among young adults—some in their 20s and 30s. The question that experts are desperately seeking to answer is: Why now?
At the center of the crisis is a hypothesis that's gaining momentum: the American diet and increasing levels of obesity are fueling early-onset colon cancer.
Colorectal cancer is the second leading cause of cancer death in the U.S., and a study published in the journal BJS by Oxford University Press indicates this increase is strongly associated with obesity-related circumstances like chronic inflammation, raised insulin, and non-alcoholic fatty liver disease.
A 2019 study identified that women who were defined as obese had almost twice the risk of early-onset colorectal cancer compared to their non-obese peers. With a projection showing that about half of all U.S. adults will be obese by 2030, the association is increasingly difficult to dismiss.
Obesity is not the sole offender. The Western diet, high in ultra-processed foods, red meat, added sugars, and low in fiber, is being put under extreme scrutiny. Conjugated with alcohol intake, smoking, and a lack of physical activity, this diet could be fueling an insidious epidemic.
Another new piece of the puzzle is a toxin named colibactin, which is made by a strain of E. coli living in the colon. It has been discovered to cause damage to colon cells' DNA, forming a biological pathway that may lead to cancer formation.
Although still an emerging field of study, the presence of colibactin-producing bacteria may partly account for why some individuals with no such family history or apparent lifestyle risk develop colorectal cancer in their 30s or 40s. Researchers are increasingly looking to the gut microbiome, an intricate system heavily controlled by diet, antibiotics, and environment.
Why the American Diet Is Being Blamed for Rising Colon Cancer Rates?
The standard American diet—widely known as a Western-style diet—is rich in ultra-processed foods, red and processed meats, added sugars, and refined carbohydrates but poor in fiber, whole grain, and fresh vegetables and fruits. This dietary pattern has for a long time been linked to chronic diseases such as obesity, type 2 diabetes, and heart disease, but increasing evidence now establishes a clear connection with early-onset colorectal cancer as well.
One of the most important factors is obesity, which is growing very fast in America and is now thought to be a major driving force in the incidence of colon cancer in younger adults. Obesity causes chronic inflammation and high levels of insulin in the body—both of which are known to stimulate cancer cell growth, including within the gastrointestinal system.
In a 2019 report, obese women were found to have almost twice the risk of developing early-onset colorectal cancer. Considering that nearly half of all American adults are projected to be obese by 2030, this is an extremely troubling trend.
Furthermore, low-fiber diets prevalent in fast food-dominated and processed food-based diets prolong digestion and inhibit healthy cell turnover in the colon. Fiber is essential for a healthy gut microbiome, the disruption of which can lead to the proliferation of harmful bacteria such as E. coli. Certain strains of E. coli synthesize colibactin, a toxin that has been proven to induce DNA damage in colon cells, causing it to initiate cancer development.
The issue is not limited to a single food category, but instead a combination of unhealthy dietary habits, sedentary lifestyle, and higher intake of pro-inflammatory and metabolic-disturbance-promoting food items.
Simply put, the American diet fosters a setting where cancer is more likely to develop—making it one of the most modifiable risk factors in the fight against early-onset colorectal cancer.
Why Are Young Adults Facing the Brunt of Colon Cancer?
What's of particular concern is how quickly things are shifting. Adults born in 1990 are twice as likely to get colon cancer and four times as likely to get rectal cancer as adults born in 1950. And this increase isn't limited to America—these same trends are being seen across the world.
In American men below 50, colorectal cancer is currently the number one cause of cancer death. In women aged between 50 and younger, it comes second.
These are figures calling for action—but action is slow, in part because colorectal cancer has traditionally been viewed as an old-age disease. That presumption is causing warning signs to go missed, particularly in younger patients who are not considered at risk.
Is Being Diagnosed Too Late Making Treatment Harder?
For younger patients, the path to a diagnosis is typically riddled with obstacles. Symptoms such as abdominal pain, fatigue, rectal bleeding, or unexplained weight loss are commonly dismissed or mislabeled as less severe conditions like hemorrhoids or irritable bowel syndrome.
By the time they are diagnosed with cancer, it's usually at a late stage—decreasing treatment choices and chances of survival. Even when the treatment is given early in life, younger patients tend to receive harsh therapies, which don't always benefit them but usually compromise quality of life, including fertility, body image, and mental well-being.
As lead author Dr. Char notes, “We’re seeing patients not only battling the disease but also facing financial stress, work disruptions, and emotional trauma at a point in life where they’re just beginning careers or raising young families.”
Colorectal cancer is not affecting all communities equally. Data shows that Black, Hispanic, Indigenous, and Asian Americans are disproportionately impacted—both in incidence and mortality.
This mirrors historical inequities in access to healthcare, preventive tests, and diet, only intensified by economic inequality. In several of these populations, obstacles such as lack of trust in the medical system, lower rates of insurance, and fewer sources of healthy food create prevention and early detection much more difficult.
Public health leaders contend that to stem colorectal cancer is to address not only healthcare systems, but also the wider social determinants of health.
Screening and Awareness Need to Shift Towards Improved Prevention
The increasing burden of early-onset colorectal cancer is forcing health systems to reconsider screening recommendations and public awareness programs. The U.S. Preventive Services Task Force already reduced the recommended screening age from 50 to 45, but most experts indicate that may not be soon enough—particularly for individuals at high risk.
Vigilance raising population awareness regarding symptoms, family history risk, and changes in lifestyle is of utmost importance. Early application of screening tests such as colonoscopy and stool DNA tests is effective. However, for younger patients, particularly those who are not insured, access continues to be an issue.
Increased research on early detection, non-invasive diagnostic modalities, and individualized screening intervals is needed urgently.
The rise in early-onset colorectal cancer is not a mystery without leads. Obesity, poor diet, microbial changes, and delayed diagnoses are all contributing factors that can be addressed with policy, education, and targeted intervention but it requires collective will. That means:
- Health systems taking young patients’ symptoms seriously
- Researchers accelerating efforts into microbiome and genetic testing
- Communities pushing for better food access, active lifestyles, and equitable care
- People getting educated on their risk—and fighting for screening
This isn't simply about cancer numbers. It's about the actual lives—lives of young people—lost to a preventable, curable disease. If we persist in viewing colon cancer as something that happens to older people, we'll be losing a generation that's already up against its toughest battle yet.
Can AI Predict Your Risk Of Cancer? FDA Approved A New Tool That Spots Disease 5-Year Before It Appears
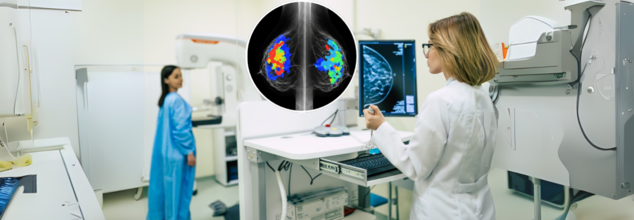
The U.S. Food and Drug Administration (FDA) has authorized the first-ever artificial intelligence (AI) tool designed to predict a woman’s five-year risk of breast cancer using a routine screening mammogram. The announcement, made on May 30, 2025by the tool’s developer, Clairity, marks a pivotal step in how breast cancer is detected and prevented—and it may just redefine the standard of care in women’s health.
This isn’t just another AI detection tool. Clairity’s platform, known as CLAIRITY BREAST, is not focused on spotting existing tumors, but rather on forecasting who may develop breast cancer years in advance. It shifts the paradigm from early detection to early risk prediction, potentially giving clinicians a critical head start in identifying high-risk individuals—before cancer ever forms.
This innovation comes from the vision of Dr. Connie Lehman, a radiologist and professor at Harvard Medical School, and the former chief of breast imaging at Massachusetts General Hospital. With decades of experience detecting cancers on mammograms, Lehman realized a key gap in screening: the lack of modern, image-based risk assessment tools.
“Our imaging technology was advancing fast, but our methods to identify women at high risk weren’t keeping up,” said Lehman at the 2025 American Society of Clinical Oncology (ASCO) Meeting, where the FDA authorization was announced.
While most existing risk models consider age, genetics, and family history, they often miss women who don’t fit those boxes. In fact, 85% of women diagnosed with breast cancer have no family history, and 50% have no identifiable risk factors at all. This makes Clairity’s approach uniquely valuable.
How The Breast Cancer Detection AI Tool Works?
CLAIRITY BREAST leverages deep learning and computer vision algorithms trained on millions of mammogram images, each linked to five-year follow-up data. By analyzing the subtle imaging features in breast tissue—often imperceptible to the human eye—the system generates a validated five-year risk score for each patient.
That score is integrated seamlessly into existing clinical workflows, providing radiologists and oncologists with a powerful new layer of information for decision-making.
“Now we can move even further upstream,” said Lehman. “Not just detecting cancer early—but predicting it, personalizing care, and even preventing it.”
Traditional screening strategies are reactive, catching cancer once it’s already present. But with Clairity, the approach becomes proactive, especially for women who may otherwise fall through the cracks of conventional risk models.
“This FDA authorization is a turning point,” said Dr. Larry Norton, founding scientific director at the Breast Cancer Research Foundation. “Most existing risk models miss the very women who go on to develop breast cancer. Clairity changes that.”
Younger women in particular stand to benefit. While breast cancer incidence is still highest in women over 50, cases among younger women are rising, yet they’re often not recommended for routine screening unless they have known risk factors. Clairity’s AI-powered insights can help clinicians tailor screening plans and intervene earlier for women who previously would have gone unflagged.
Dr. Lehman describes breast cancer not as a binary—either present or not—but as a continuum, with progression that begins long before a tumor is visible.
“There’s a point even before ductal carcinoma in situ (DCIS), when cancer hasn’t developed, but the risk is there,” she explained. “That’s where CLAIRITY can intervene—well before invasive cancer begins.”
The goal, according to Lehman, isn’t just to detect breast cancer earlier, but to predict and prevent it, in the same way that doctors routinely assess cardiovascular risk based on blood pressure, cholesterol, or BMI.
Until now, breast cancer lacked such a dynamic, image-based risk tool. That’s what makes Clairity’s authorization so significant.
AI’s Expanding Role in Radiology
AI has been used in radiology for decades, first to flag microcalcifications in mammograms in the early '90s. But back then, AI systems were limited to rule-based logic and needed exhaustive human guidance.
Today’s AI, especially in platforms like Clairity, goes far beyond what human vision can perceive. It identifies patterns in breast tissue texture and density at the pixel level, learning from vast image sets without needing explicit human-labeled inputs.
Lehman compared it to how machines learn to distinguish cats from dogs—by exposure to thousands of examples rather than being told what features to look for. In the case of breast cancer, the stakes are obviously much higher.
“This technology allows us to see what we couldn’t see before, and that opens doors to dynamic risk assessment,” Lehman said. “Eventually, we may even use these tools to monitor how interventions like medication, weight loss, or hormone therapy change a woman’s risk over time.”
Backed by Santé Ventures and ACE Global Venture, Clairity was founded in 2020 with a clear goal: to bring sophisticated AI tools to routine mammography. Now, with FDA de novo authorization, it’s set to hit the market by late 2025.
The company estimates the global market for breast cancer prediction tools at $63 billion, suggesting broad clinical interest and commercial potential.
As imaging centers, hospitals, and oncologists look to integrate risk prediction into daily care, Clairity's success will depend on adoption, clinician trust, and real-world outcomes. But with this regulatory milestone, a major hurdle has been cleared.
The FDA’s green light for CLAIRITY BREAST doesn’t just add a new tool to the cancer detection toolbox—it fundamentally changes the playing field. By enabling risk prediction from a single mammogram, it turns routine screening into a forward-looking, personalized roadmap for prevention.
Canine Parvovirus Outbreak Among Pet Dogs In Ontario, Can Humans Also Get Infected?

Credits: Canva
Ontario is currently facing an outbreak of canine parvovirus (CPV), which has led to spikes in online searches on more information on the dog disease.
Expert Tracy Fisher, a veterinarian from Regina and the president-elect of the Canadian Veterinary Medical Association, told CTVNews.ca that the frequency of cases varies every year. The expert has also commented that the prominence of CPV in Canada is common and persistent. The outbreak had made headlines earlier this summer in London too.
What is Canine Parvovirus?
PetMD notes that CPV is the most serious virus that dogs and puppies can get. However, the silver lining here is that it is preventable with proper vaccination, though it is still widely prevalent, especially in puppies and poorly vaccinated adolescent dogs.
DVM Ellen Malmanger writes that CPV is an infectious DNA virus that commonly causes severe illness in young and unvaccinated dogs. It also affects the body's rapidly dividing cells. This means the intestinal tract and bone marrow are usually the most affected.
As per the Veterinary Centers of America (VCA)'s Canadian division, CPV first appeared in dogs in 1978. “The virus that causes this disease is similar to feline panleukopenia (feline distemper); the two diseases are almost identical,” the website for VCA Canada, a network of animal hospitals, says. “However, that has never been scientifically proven.”
VCA Canada notes that primary source of infection is through the ingestion of the feces of already-infected dogs. It can be easily transmitted through contact with the hair or feet of infected dogs or with objects contaminated by the infected feces.
According to VCA Canada, the virus initially targets the animal's tonsils or lymph nodes, where it infects lymphocytes—a type of white blood cell. These infected cells then spread the virus throughout the body, reaching areas such as the bone marrow and the intestinal lining.
Can You Touch A Dog With Parvo?
Humans cannot get parvo from dogs. Parvovirus is species-specific and so the strain that affects dogs, known as CPV cannot infect humans. However, humans can contact similar virus from contaminated surfaces, such as Norovirus, but there is no risk of acquiring parvo from dogs.
What Is Human Parvovirus?
The human parvovirus is different, and is caused by the B19 strain. It was first discovered in 1974 during evaluation and testing for hepatitis B, and was later named by the International Committee on Taxonomy of Viruses in 1985.
Parvovirus B19 is a common and often overlooked infection that spreads from person to person. While it’s not widely talked about, it’s more widespread than most people think — in fact, nearly half of all adults in the U.S. have had it at some point in their lives.
What makes it tricky to spot is that most people don’t even realize they’ve been infected. The virus rarely causes symptoms, and when it does, they tend to be mild. It’s usually only people with weakened immune systems — where the body’s natural defense isn’t working as it should — who may experience more noticeable effects. That’s because parvovirus B19 can temporarily interfere with the body’s ability to make red blood cells.
Anyone can catch the virus, regardless of age or ethnicity. But those most at risk include individuals with immune system issues or conditions that affect red blood cell production. Children are also more likely to get infected, but in most cases, they don’t show any symptoms. If symptoms do appear, they’re generally mild and manageable.
1 Dead And 40 Sick With Legionnaires Outbreak In London– What You Need To Know
(Credit-Canva)
London is currently dealing with a serious lung sickness called Legionnaires' disease. So far, one person has died, and more than 40 people have gotten sick in just the past week. The Middlesex-London Health Unit has announced this as an outbreak.
The Health Unit UK is working closely with provincial health groups to find out where this sickness started. This involves taking samples from different cooling systems, which can take some time. Officials know people are eager to find the source, and they are too, but they don't have an exact location yet. Teams are busy collecting water samples and swabs from cooling systems. They'll then compare these to samples from the sick people, hoping to find a common source.
Normally, only a few cases of Legionella, the bacteria that causes the disease, are reported each month. However, the number suddenly jumped to 43 new cases, which is why the outbreak was declared. Health officials think the recent warm weather probably played a role in this increase, as the number of cases was much higher than what they usually see at this time of year.
What is Legionnaires' Disease?
The National Health Services UK explains that Legionnaires' disease is caused by tiny bugs called Legionella bacteria. These bugs are naturally found in water sources like hot tubs, cooling towers, hot water tanks, large pipes, and parts of air conditioning systems.
It's important to understand that this sickness does not spread from person to person. People get sick when they breathe in tiny drops of water or mist that contain these bacteria. Most people who are exposed to the bacteria don't get sick, but some might get a milder, flu-like illness called Pontiac fever.
Legionnaires Outbreak: Where Is This Bacteria Found?
Legionella bacteria are naturally found in water sources like hot tubs, cooling towers, hot water tanks, large plumbing systems, and parts of air-conditioning systems. People get sick if these bacteria become airborne as mist (from wind or fans) and are then inhaled.
Most people exposed to Legionella don't get sick, though some might get a milder, flu-like illness called Pontiac Fever, which usually goes away on its own. People who are older, have lung problems, or have weaker immune systems are at a higher risk of getting a serious infection. It's important to remember that Legionella does not spread from person to person.
Also Read: Canine Parvovirus Outbreak Among Pet Dogs In Ontario, Can Humans Also Get Infected?
Legionnaires Outbreak: Important Health Guidelines to Follow
If you develop symptoms like fever, cough, or shortness of breath, you should seek medical attention right away.
The Health Unit asks all business owners and property managers to make sure their cooling equipment is regularly maintained and cleaned according to the manufacturer's instructions. This is the best way to prevent future outbreaks. The Middlesex-London Health Unit also listed some commonly asked questions regarding the disease,
Legionnaires Outbreak: Will Masks Help?
While face masks can reduce your risk of getting respiratory illnesses, including Legionella, the general public's risk for Legionnaires' disease is currently low. Because of this, the Health Unit is not recommending widespread community masks to use specifically to prevent this disease.
Legionella bacteria can spread over a large area through the air. The exact source of this current outbreak hasn't been found yet. At this time, it's not known if this outbreak is from the same location as last year's Legionella outbreak. However, this possibility is being considered as part of the ongoing investigation.
© 2024 Bennett, Coleman & Company Limited

