- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Explained: New Autism Research Reveals 4 Distinct Subtypes, Links Genes To Children's Traits

Credits: Health and me
Autism has long been known yet unknown, its defining characteristics understood for decades, but its biological roots unknown. Now, a new research study conducted at Princeton University and the Simons Foundation is changing the narrative by identifying four separate genetic subtypes of autism. This study is a key turning point in understanding that autism is not one disorder, but several variations based on genetic diversity.
Autism is generally thought of as a spectrum, that is, each person exhibits a particular set of characteristics, behaviors, and abilities. To date, efforts to connect particular genes with particular behaviors have been unsuccessful. You might think of it as sitting down to try to assemble several jigsaw puzzles simultaneously, all of which share similar pieces. That is, until scientists started to sort children into categories by behavior before examining their genomes.
Natalie Sauerwald, co-author and associate research scientist at the Flatiron Institute, clarifies, "We couldn't see the whole picture…until we divided people into subtypes."
Her lab, in collaboration with Aviya Litman of Princeton, analyzed data from more than 5,300 kids between 4 and 18 who were in SPARK, a large autism cohort. They measured over 230 characteristics—social communication, repetitive behaviors, developmental milestones, anxiety, ADHD, and others. Employing sophisticated statistical modeling, they discovered four clusters, each associated with distinct genetic patterns.
The Four Autism Subtypes Identified
Social and Behavioral Challenges (37%)
Children achieve typical developmental milestones but have difficulty with social skills, repetitive behaviors, and usually suffer from ADHD, anxiety, or depression.
Mixed ASD with Developmental Delay (19%)
They have a mixture of autism characteristics with delays in early development. Co-occurring conditions are less prevalent compared to the first group.
Moderate Challenges (34%)
Traits are less severe than in other groups, and developmental milestones are on track. There are no major co-occurring conditions.
Broadly Affected (10%)
The most severely affected, this group exhibits pervasive autism characteristics, developmental delay, and intellectual disability.
Notably, the subtypes aligned directly with genetic results. The Broadly Affected subgroup had the greatest percentage of de novo mutations, genetic changes that occur spontaneously and aren't inherited.
Why Recognsing Genetic Traits Matter For Autism Diagnosis And Treatment?
The implications of the study are vast for science, medicine and families. For the first time, genes intersect meaningfully with behavior in a way that shows there isn't one biological pathway to autism. Rather, by correlating certain profiles of traits with different kinds of genetic mutations, the study demonstrates that there are several developmental pathways—representing a profound departure from the old one-size-fits-all paradigm. Clinically, it means potentially improved prognoses and more tailored treatment plans. For example, some subtypes of children may be more helped by speech and social therapy, whereas others will need targeted developmental therapies. From the research standpoint, this makes it possible for researchers to research autism in smaller, more homogeneous populations, which significantly enhances the promise of identifying targeted biological treatments that work.
Dr. Catherine Lord, a leading autism researcher not involved in the study, noted, “These groups make sense…and the connection to genetics is what makes these results most noteworthy.”
As Sauerwald stresses, these four subtypes aren’t definitive but serve as a foundation:
“We’ve discovered a data-driven framework showing there are at least four meaningful subtypes…meaningful both for clinical work and research.”
But this group was largely white and not strictly representative. Further research is required to affirm whether these subtypes hold true across the world. The question then becomes how to translate this model into day-to-day clinics—can pediatricians accurately assign subtypes, and will it lead to better outcomes?
Beyond Behavior Key Traits of Autism
Autism is typically characterized by social and behavioral issues, but there's more than meets the eye. From sensitivity to sound and light, and from stimming to masking and hyperfocus, defining characteristics go beyond behavior. Knowing these trends does a better job of describing in more complete, accurate terms how each person is affected in their own way by autism.
- Sensitivities to sound, light, taste
- Stimming routines employed for concentration or self-calming
- Masking habits, where autistic people change behavior in order to fit in
- Burnout, profound exhaustion after social overstimulation
- Literal thinking, hyperfocus, and deep special interests
Pattern combinations such as these group differently across subtypes and affect each child's developmental trajectory.
Are We Moving Toward Personalized Autism Treatment?
For parents, knowing a child's particular autism subtype may bring them much-needed clarity, direction, and hope. By having a more specific profile of their child's subtype, educational interventions can be more appropriately matched to individual strength and difficulty profiles, supporting more efficient learning assistance. Mental health treatment, as well, can be more specifically tailored to address the specific affective and behavioral tendencies associated with each subtype. Outside of clinical treatment, understanding a child's subtype can assist families in linking with others who are undergoing similar experiences, creating peer networks based on mutual understanding. And most importantly, perhaps, this information is the portal to future therapies—everything from tailored treatment regimes to possible genetic counseling or medication—all with the person's biology in mind.
In a disorder that has long defied tidy labels, this subclassification provides a whole lot more than even labels—provide guidance.
Autism's intricacy had infuriated researchers and families both. But with purposeful subtypes in place, the field now has a plan. Genetics can engage significantly with therapy and support and make a difference in people's lives.
Autism is no longer a monolithic condition—it's a spectrum within a spectrum, identified not just by diagnosis but by the biology that informs every experience.
Influenza Flu Symptoms May Be Changing As A New Variant Spreads: What To Expect

Credits: Canva
A fast-spreading new flu variant driving a sharp rise in infections across the state is bringing with it symptoms that differ from what many people usually associate with influenza.
With flu activity now classified as “very high” in Illinois, health experts say a mutated and highly contagious strain known as subclade K is changing how the illness shows up, particularly when it comes to fever patterns. One of the biggest differences doctors are seeing is how intense and long-lasting fevers have become, especially among children.
“There’s more fever with the flu this year than people are used to,” said Dr. Mark Loafman, chair of Family and Community Medicine at Cook County Health, speaking to NBC Chicago. “The fever can last five to seven days, and that’s concerning. You feel sick, you don’t feel like you’re improving, and that can be worrying.”
Adding to the concern, Dr. Juanita Mora, national spokesperson for the American Lung Association, as per NBC News, said some patients are finding that common fever-reducing medicines such as Tylenol or Motrin are not working as effectively. “This strain is causing very high fevers,” Mora said. “There’s also a severe cough that just doesn’t go away, a lot of phlegm, vomiting, diarrhoea, and significant joint and muscle pain.”
Influenza Flu Symptoms To Watch For
Vomiting has never been among the most typical flu symptoms, though it does occur more often in children. What doctors are now noticing with this strain is an increase in gastrointestinal symptoms among adults as well.
“Kids with the flu often experience nausea or vomiting,” Loafman explained. “Adults usually don’t as much, but we are hearing more reports of GI symptoms in adults who have this subclade K strain.” Because of this, he said flu should not be ruled out just because stomach symptoms are present.
“If you have GI issues along with body aches, fever, and respiratory symptoms, flu is still very much a possibility,” he said, adding that at-home flu tests can be useful if someone suspects they are infected.
Warnings have already been issued by the Illinois Department of Public Health and several county health departments as flu-related hospital admissions and positive test results continue to climb.
According to the latest state update released Monday, flu activity has reached “very high” levels, the most severe category used by the CDC to track respiratory illness trends.
Health officials say most emergency room visits and hospital admissions related to respiratory illness are currently being driven by flu cases.
Common Flu Symptoms To Know
Flu symptoms typically appear one to four days after exposure, according to the Cleveland Clinic.
The CDC lists the following common symptoms:
- Fever or feeling feverish, along with chills
- Cough
- Sore throat
- Runny or blocked nose
- Muscle or body aches
- Headaches
- Fatigue
- Vomiting and diarrhoea, which are more common in children than adults
Not everyone with the flu will develop a fever. However, health officials note that gastrointestinal symptoms are being reported more often in adults with the new strain.
Influenza Flu Warning Signs To Watch For
Because this variant is linked to higher and longer-lasting fevers, Mora said it is crucial to recognise when medical care is needed.
“High fevers that don’t come down are one warning sign,” she said. “Another is trouble breathing, including wheezing, chest muscle use, or a cough that won’t stop. And dehydration is a major concern, especially if someone is barely eating or drinking.”
The CDC outlines different warning signs for children and adults.
In children:
- Rapid or laboured breathing
- Bluish lips or face
- Ribs pulling in with each breath
- Chest pain
- Severe muscle pain or refusal to walk
- Signs of dehydration such as no urine for eight hours, dry mouth, or no tears when crying
- Lack of alertness or interaction
- Seizures
- Fever above 104°F that does not respond to medication
- Any fever in infants under 12 weeks
- Symptoms that improve and then worsen
- Worsening of existing medical conditions
In adults:
- Difficulty breathing or shortness of breath
- Ongoing chest or abdominal pain
- Dizziness, confusion, or difficulty waking
- Seizures
- Little or no urination
- Severe muscle pain
- Extreme weakness or unsteadiness
- Symptoms that return or worsen after improving
- Worsening of chronic illnesses
How Long Is Flu Contagious?
According to the CDC, people can spread the flu starting about one day before symptoms appear and up to seven days afterward. Most people are most contagious around three days into the illness. Young children and those with weakened immune systems may remain contagious longer.
“It’s usually about five to seven days from when symptoms start before people stop shedding high levels of the virus,” Loafman said. “Ten days is very cautious, but not always necessary.”
He advised masking around vulnerable people during the first week, practicing good hand hygiene, and staying home whenever possible. “If you can stay in, stay home,” he said, as per NBC News.
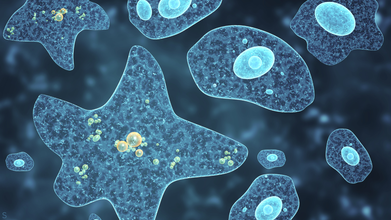
The Invisible “Brain-Eating” Bacteria Lurking in Water Pipes That Can Cause Deadly Infections
Credit: Canva
Environmental and public health scientists have begun warning against the dangers of having free living amoeba in water systems that are capable of triggering severe diseases in humans.
In a recent perspective article published in Biocontaminant, the researchers noted that climate change, deteriorating water infrastructure and limited systems for monitoring and detection are the key factors that have allowed these pathogens to spread and persist.
Corresponding author Longfei Shu of Sun Yat sen University explained: "What makes these organisms particularly dangerous is their ability to survive conditions that kill many other microbes.
"They can tolerate high temperatures, strong disinfectants like chlorine and even live inside water distribution systems that people assume are safe."
The scientists also emphasized that not only can amoebae spread illnesses on its own, it can also act as hidden carriers for other harmful microbes.
By sheltering bacteria and viruses inside their cells, amoeba these unicelled organisms protect these pathogens from disinfection and help them persist and spread in drinking water systems. This so-called Trojan horse effect may also contribute to the spread of antibiotic resistance among humans.
How Dangerous Is Amoeba?
Amoeba are single-celled organisms that naturally live in soil and water. Most species do not cause harm yet some can prove to be fatal.
Some of the diseases caused by this kind of bacteria include Amebiasis (Amoebic Dysentery), an intestinal infection by Entamoeba histolytica, causing diarrhea, cramps and potential liver abscesses as well as Primary Amoebic Meningoencephalitis (PAM) from Naegleria fowleri, a rare but nearly always fatal brain infection from contaminated water entering the nose.
Effects of amoeba-caused infections range from intestinal issues (liver abscesses, anemia, peritonitis) to severe neurological damage (coma, seizures, death) from brain-eating types, with Acanthamoeba causing eye infections (keratitis).
Experts recommend thoroughly washing your hands after toilet use and before handling food, drinking clean water especially in unsanitary conditions and avoiding getting water up your nose in warm freshwater to prevent such infections.
The Indore Crisis
This comes days after the recent Indore sewage water controversy which has claimed the lives 10 people and left over 1,400 people hospitalized, according to Indore Mayor Pushyamitra Bhargava.
However, locals claim that the outbreak has instead caused the death of 17 residents, including a six-month-child. The situation has also left Parvati Bai, 67, with kidney failure, a brain stroke and symptoms of Guillain-Barré Syndrome, or GBS.
GBS is a rare condition where your immune system attacks the nervous system and can cause paralysis as well as death, in certain cases.
The outbreak occurred due to lapses in civic infrastructure. Investigation revealed that a toilet constructed directly above a main drinking pipeline near a police outpost, without a mandatory safety tank resulted in the sewage mixing with drinking water.
New FDA Approved Blood Test Can Predict Alzheimer’s Disease Before Symptoms Appear

Credit: Canva
The US Food and Drug Administration has approved the use of a blood test which can help diagnose Alzheimer’s disease in adults aged 55 and above.
The blood test, known as Lumipulse, can detect amyloid plaques associated with Alzheimer’s disease and has proven to be a “less invasive option” that “reduces reliance on PET scans and increases diagnosis accessibility.”
FDA Commissioner Martin A. Makary said of the landmark decision, "Alzheimer’s disease impacts too many people, more than breast cancer and prostate cancer combined.
"Knowing that 10% of people aged 65 and older have Alzheimer's, and that by 2050 that number is expected to double, I am hopeful that new medical products such as this one will help patients."
It remains unclear when this test will be available for commercial use across the world.
What Is Alzheimer’s Disease?
Alzheimer's disease is one of the most common forms of dementia and mostly affects adults over the age of 65.About 8.8 million Indians aged 60 and above are estimated to being living with Alzheimer's disease. Over seven million people in the US 65 and older live with the condition and over 100,00 die from it annually.
Alzheimer's disease is believed to be caused by the development of toxic amyloid and beta proteins in the brain, which can accumulate in the brain and damage cells responsible for memory.
Amyloid protein molecules stick together in brain cells, forming clumps called plaques. At the same time, tau proteins twist together in fiber-like strands called tangles. The plaques and tangles block the brain's neurons from sending electrical and chemical signals back and forth.
Over time, this disruption causes permanent damage in the brain that leads to Alzheimer's disease and dementia, causing patients to lose their ability to speak, care for themselves or even respond to the world around them.
While there is no clear cause of Alzheimer's disease, experts believe it can develop due to genetic mutations and lifestyle choices, such as physical inactivity, unhealthy diet and social isolation.
Early symptoms of Alzheimer's disease include forgetting recent events or conversations. Over time, Alzheimer's disease leads to serious memory loss and affects a person's ability to do everyday tasks.
There is no cure to this progressive brain disorder and in advanced stages, loss of brain function can cause dehydration, poor nutrition or infection. These complications can result in death.
How Does The Test Work?
Lumipulse detects amyloid plaques and tangles in blood plasma and calculates the numerical ratio of the levels of the two proteins. Based on the ratio, the test shows a positive or negative result for the disease.As explained by Dr Abhay Moghekar, an associate professor of neurology at Johns Hopkins University School of Medicine, who helped study and evaluate the test for FDA approval, "If this test is positive, there’s a greater than 90% chance that you have amyloid plaque in your brain.
"Getting a blood test is gonna be far easier, quicker and cheaper,” he said. “It’s going to allow early access to therapy, so it is going to revolutionize care of patients with dementia."
However, the federal agency also noted certain limitations associated with the test such as it can only be used for patients 55 and older who are already experiencing memory problems.
The FDA also cautions that the test is not intended as a standalone diagnostic tool for Alzheimer’s and results should be interpreted based on the patient’s medical history and other assessments, such as cognitive testing.
© 2024 Bennett, Coleman & Company Limited

