- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
FDA Clears Prefilled Syringe for Shingles Vaccine, Aim Is for Smoother Administration

Credits: Canva
In a move that could make the shingles vaccination process smoother for both patients and healthcare providers, the U.S. Food and Drug Administration (FDA) has approved a new prefilled syringe version of Shingrix—the widely used vaccine for shingles, or herpes zoster.
The vaccine, developed by global biopharma company GSK, has already been a go-to option for adults aged 50 and older and certain immunocompromised individuals. With this newly approved version, the process of getting vaccinated becomes significantly simpler, without compromising efficacy or safety.
From Two Vials to One Prefilled Syringe
Until now, Shingrix has been administered in a two-step process. It involved combining two separate vials—a freeze-dried (lyophilized) powder containing the antigen, and a liquid adjuvant, by trained healthcare workers just before the vaccine was given.
This mixing step, while manageable, added a layer of complexity that could sometimes slow down the vaccination process, particularly in busy clinics or pharmacies.
With the FDA’s approval of the prefilled syringe, that extra step is eliminated. The vaccine is now available in a ready-to-use format, making the administration process quicker and reducing the chances of handling errors.
For healthcare professionals, this means less prep time and more streamlined delivery. For patients, it could mean shorter waiting times and potentially increased access.
Who Can Get the New Shingrix Syringe?
The approved prefilled syringe format maintains the same usage guidelines as the original formulation. It is licensed for use in:
- Adults aged 50 years and older
- Adults aged 18 years and older who are or will be at increased risk of shingles due to immunodeficiency or immunosuppressive conditions (from either illness or medical treatments)
This broadened scope ensures that vulnerable individuals, like those undergoing chemotherapy, transplant patients, or people living with HIV, can continue receiving this critical protection against shingles, now in a more efficient form.
Why This Matters
Shingles isn’t rare—in fact, according to the Centers for Disease Control and Prevention (CDC), about 1 in 3 Americans will develop shingles in their lifetime.
It is caused by the reactivation of the varicella-zoster virus, the same virus responsible for chickenpox. When it comes back, often years later, it manifests as a painful rash, often accompanied by burning or shooting pain.
In some cases, it can lead to long-term complications like postherpetic neuralgia, where pain lingers for months or even years after the rash clears.
“This new presentation of Shingrix was developed to streamline the vaccination process, supporting health care professionals to provide protection against shingles,” said Tony Wood, Chief Scientific Officer at GSK, in a statement. “Shingles is a disease that one in three U.S. adults will develop in their lifetime.”
The FDA’s decision was based on data that demonstrated technical comparability between the new prefilled syringe format and the original two-vial version. That means the vaccine’s safety, quality, and effectiveness remain unchanged in the updated version.
New Parkinson's Treatment Is Like A Pacemaker To The Brain

Credits: Canva
In a major leap for Parkinson’s disease treatment, a new form of brain implant is transforming the way patients experience relief from symptoms like tremors, stiffness, and slowness of movement. Often likened to a “pacemaker for the brain,” this breakthrough, known as adaptive deep brain stimulation (aDBS), is being hailed as a personalized, real-time therapy that adjusts to the brain's needs moment by moment.
From Reluctance to Relief: One Patient’s Journey
As the Scientific American reports, Keith Krehbiel had lived with Parkinson’s disease for nearly 25 years before agreeing to undergo a surgery he had long avoided. In 2020, as his symptoms worsened, he reluctantly said yes to a deep brain stimulation (DBS) implant, unaware he’d soon be part of a historic medical trial.
Just as he was preparing for surgery, neurologist Helen Bronte-Stewart of Stanford University received approval to launch a new trial testing an upgraded form of DBS. She offered Krehbiel the chance to be the first participant. His response: “Boy, do I!”
Five years on, the clinical trial, known as ADAPT-PD, involving 68 participants is now under review for publication. But the initial results have already been powerful enough to earn regulatory approval in both the U.S. and Europe.
What Makes Adaptive DBS Different?
As per the American Parkinson Disease Association (APDA), traditional DBS works by sending electrical impulses to parts of the brain that control movement, helping correct abnormal brain activity. But until now, it operated on fixed settings, adjusted manually by doctors based on patient feedback during clinic visits. That’s where adaptive DBS is changing the game.
This next-generation implant not only stimulates the brain but also listens to it. Using Medtronic’s BrainSense™ technology, the system continuously reads brain signals called local field potentials (LFPs), particularly in the beta-band frequency range, which has been linked to motor symptoms in Parkinson’s patients.
When the system detects brainwave patterns that suggest tremor, stiffness, or slowness, it automatically tweaks the stimulation levels in real-time.
“It’s like a smart pacemaker for the brain,” Bronte-Stewart explained. The goal is simple but revolutionary: deliver just the right amount of stimulation when it’s needed most, and ease off when it’s not.
A New Era for Parkinson’s Care
The implications of this adaptive technology are wide-reaching. APDA notes, over one million people in the U.S. and 1.2 million in Europe live with Parkinson’s, a progressive neurological disorder that often grows resistant to medications over time. While traditional DBS has helped around 200,000 patients worldwide, only 40,000 devices implanted since 2020 are equipped with the adaptive capability, and many of them haven’t even activated the feature yet.
With the ADAPT-PD trial results clearing regulatory hurdles, that’s poised to change. Krehbiel’s own experience is one reason why: after his surgery, his symptoms significantly improved, and his quality of life followed suit.
The benefits of adaptive DBS extend beyond Parkinson’s. Neurologists believe this “closed-loop” approach could also be effective for other movement disorders like Tourette’s syndrome, and even psychiatric conditions such as obsessive-compulsive disorder (OCD) and depression — though more trials are needed.
Experts believe the evolution of adaptive DBS is just beginning. Next on the horizon is the integration of artificial intelligence. By learning individual brain patterns, AI could help predict when symptoms are about to worsen, and adjust stimulation preemptively.
Rakesh Roshan Undergoes Angioplasty, Shares Health Update And Asks People Over 40 To Get Regular CT Scan
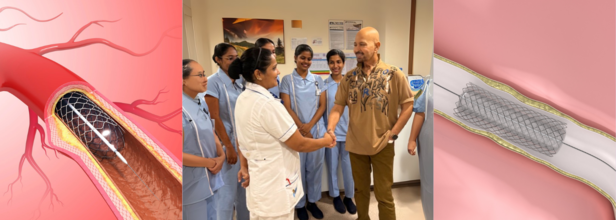
Credits: Canva and Instagram
Veteran filmmaker Rakesh Roshan, known for hits like Kaho Naa... Pyaar Hai and Krrish, opened up on Tuesday about his recent health scare that led to an urgent angioplasty procedure.
In a heartfelt Instagram post, the 74-year-old shared a photo from his hospital room, shaking hands with a nurse and thanking the medical team who cared for him.
While the photo appeared reassuring, his caption revealed a critical diagnosis that had, until recently, gone unnoticed.
Why Routine Checkups Are Important
Roshan wrote that during a routine full-body check-up, a cardiologist recommended a sonography of the neck. This suggestion proved to be a turning point. “By chance, we found out that although asymptomatic, both my carotid arteries to the brain were above 75% blocked,” he shared. “Which, if ignored, could be potentially dangerous.”
Without any outward symptoms, the condition could have led to a stroke or other serious complications. He immediately checked into the hospital to undergo “preventative procedures,” including angioplasty.
Now safely back home, Roshan says he feels well and is eager to resume his workouts. “I hope this inspires others to stay on top of their health, especially where the heart and brain is concerned,” he wrote.
A Reminder for Preventive Care Over Cure
The filmmaker urged everyone over the age of 45–50 to consider a CT scan for the heart and a carotid artery sonography as part of their annual health screenings. These tests, often overlooked, can detect hidden arterial blockages that may not present symptoms until it’s too late.
“I think it’s important to remember that prevention is always better than cure. I wish a healthy and aware year to you all,” he added.
His message was met with an outpouring of support from friends and well-wishers across the industry. Actors, including Anil Kapoor, Suniel Shetty, Tiger Shroff, and others left supportive comments and emojis. Roshan’s daughter Sunaina had also earlier confirmed to the media that her father had undergone an angioplasty “in his neck” and assured fans that he was “perfectly fine.”
What Is Angioplasty?
According to Johns Hopkins Medicine, angioplasty is a medical procedure used to restore blood flow through narrowed or blocked arteries. It is most commonly done to treat coronary artery disease but can also be used in other parts of the body, such as the carotid arteries leading to the brain.
The procedure involves inserting a thin, flexible tube called a catheter into a blood vessel. The catheter is guided to the blocked area, where a small balloon is inflated to compress plaque against the artery wall, thus opening the vessel and improving blood flow. In some cases, an atherectomy may also be performed to shave or remove the plaque.
The Role of Stents in Preventing Re-Narrowing
In nearly all modern angioplasty procedures, a stent is inserted to help keep the artery open. A stent is a tiny, mesh-like metal coil that is expanded at the site of blockage. Once placed, it prevents the artery from narrowing again.
There are two types of stents:
- Drug-eluting stents, which release medication to prevent scar tissue buildup
- Bare metal stents, which don’t have a drug coating but are used in patients who may be at higher risk of bleeding
Post-procedure, patients are typically prescribed antiplatelet medications to reduce the risk of blood clots and to ensure the stent remains open.
Risks and Follow-Up Care
While angioplasty is a relatively safe procedure, there can be complications if the stent becomes blocked or scar tissue develops. Some patients may require a repeat procedure or even radiation therapy (brachytherapy) to clear the narrowing.
That’s why ongoing medical supervision and lifestyle changes—such as regular exercise, a balanced diet, and avoiding tobacco—are key to long-term heart and brain health.
Federal Investigation Uncovers Failures in Organ Donation Protocols, Triggers National Reforms

Credits: Canva
The U.S. Department of Health and Human Services (HHS) has announced a major overhaul of the nation’s organ transplant system, following a disturbing federal investigation that revealed serious ethical and safety concerns. At the heart of the issue is a Kentucky-based organ procurement organization (OPO), which allegedly continued preparations for organ donation in patients who showed signs of life.
The revelations have triggered swift action from federal agencies, as lawmakers call for transparency, stronger safeguards, and a renewed effort to rebuild public trust in the transplant process.
Uncovering a Troubling Pattern
The Health Resources and Services Administration (HRSA), under HHS, reviewed 351 authorized but incomplete organ donation cases linked to the Kentucky OPO that also serves Southwest Ohio and parts of West Virginia. Investigators found troubling practices in at least 103 of those cases, including patients displaying neurological signs incompatible with organ donation and concerns that some may not have been fully deceased at the time organ procurement was initiated.
Additional issues uncovered included poor neurological assessments, lack of coordination with medical teams, questionable consent processes, and misclassification of causes of death, especially in drug overdose cases. Smaller and rural hospitals were found to be especially vulnerable due to inconsistent oversight and limited resources.
Reopening a Closed Case and Demanding Accountability
The HRSA has now directed the Organ Procurement and Transplantation Network (OPTN) to reopen a previously closed case that had been dismissed by the OPTN Board of Directors. The earlier review had claimed "no major concerns" in the case of a neurologically injured patient. However, the new independent investigation contradicted that conclusion and cited potential negligence.
The Kentucky OPO is now required to conduct a thorough root cause analysis, especially focusing on failures like not observing the required five-minute wait after cardiac death before beginning organ recovery. The organization must also implement stricter donor eligibility rules and establish a clear, formal procedure that allows any hospital or OPO staff member to halt the donation process if patient safety is at risk.
HRSA warned that the OPO will face decertification if it fails to comply with these corrective measures.
A Call for Reform and Reassurance
During a congressional hearing this week, Rep. Brett Guthrie of Kentucky, whose own mother died while awaiting a liver transplant, stressed the importance of restoring public confidence in the system.
“We have to get this right,” Guthrie said. “Hopefully people will walk away today knowing we need to address issues but still confident that they can give life.” He reaffirmed his commitment to remain a registered organ donor.
Lawmakers emphasized that while most organ donations are conducted safely and ethically, the near-misses uncovered by the investigation are deeply concerning and could deter future donors. Some families have already chosen to opt out of organ donor registries after these incidents were made public.
How Organ Donation Works in the U.S.
Organ donation in the U.S. is a complex process involving multiple entities. Hospitals are responsible for caring for critically ill or brain-dead patients. Once death is declared or life support is withdrawn, hospitals notify local OPOs, which coordinate the recovery and placement of organs with transplant centers.
While most donations occur after brain death, a growing number take place after circulatory death, when the heart stops following withdrawal of life support. In these cases, organs are only viable if death occurs quickly and is confirmed with a mandatory five-minute waiting period.
OPOs are not allowed to be involved in declaring death or the decision to end life support. However, recent reports suggest a blurred line in practice, with concerns that OPOs have pressured hospitals during end-of-life decisions.
Stronger Safeguards, Greater Transparency
As part of its response, HRSA has ordered the OPTN to strengthen national safeguards and mandate reporting of any instance where donation is paused due to concerns from families, hospital staff, or OPO teams. The aim is to create a culture where patient eligibility is continually reassessed and where concerns can be raised without fear.
In Kentucky, the OPO says it has already begun implementing changes. Staff at every partnering hospital are now given checklists outlining protocols for identifying and handling potential donors. A new system has also been set up to allow anonymous reporting of any concerns.
Barry Massa, head of Kentucky’s Network for Hope, emphasized that OPOs do not participate in life support decisions and are “not even in the room” when such determinations are made. Still, HRSA insists that the transplant network needs more proactive collaboration and clearly defined boundaries to protect vulnerable patients.
With over 100,000 people waiting for life-saving organ transplants in the U.S., federal officials say that reforming the system is not just necessary, it’s urgent.
© 2024 Bennett, Coleman & Company Limited

