- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Global Warming Is Behind the Rise of Dangerous New Fungal Diseases
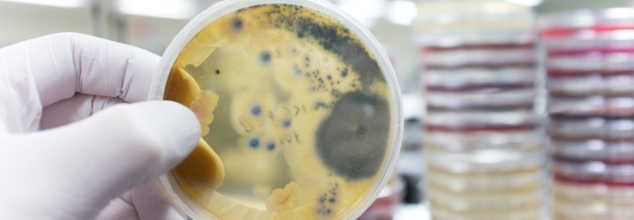
Credits: Canva
Global warming is a rising concern; however, it not just environment, but also affects our health. While we may think that global warming only leads to environmental resources being perished, however, the impact is way more. Whatever happens to the environment is directly related to humans. As per a new research by scientists from Manchester University, due to the rising temperature, a deadly fungus could cause millions of deaths annually and will spread globally. This is the Aspergillus family, which will proliferate in new regions and cause infections.
The report by Manchester University notes that the moulds living among us could further trigger the next disease outbreak.
What Is Mold?
What Is Aspergillus?
It is a group of fungi which is present globally and can cause aspergillosis, a lung disease that could spread to other organs, including your brain.
As per Science Direct, it is also an industrial chemical used for the fermentation of various foods like soy sauce, miso, and sake; however, it can also be dangerous to your health.
It also releases a huge amount of tiny spores into the air, which can cause health issues to those who consume it. It could be even concerning for those with a compromised immune system, especially people with asthma, cystic fibrosis, cancer, or anyone with a severe flu or Covid-19. These conditions may make it impossible for you to clear the spores.
Norman van Rijn, who is one of the study authors, told CNN that if the body fails to get rid of these spores, the fungus “starts to grow and basically kind of eat you from the inside out, saying it really bluntly,”
ALSO READ: Exposure To Mold Can Lead To Neurological Symptoms: Know What They Are
What Does It Do To You?
The author noted that mortality rates of Aspergillosis are actually at 20 to 40%; however, not many people get to know it, as it usually causes common symptoms like fevers and coughs.
The fungi can also alter brain functions. What happens with mold is that it can get inside your home through open doors, windows, and air conditioning systems. Inhaling mold spores or coming into contact with mold can have severe adverse effects on your health. Beyond physical symptoms like headache and allergic symptoms, it can have a significant impact on the brain and nervous system. Symptoms may vary, from mild headaches to more severe issues like memory loss or difficulty walking. While it can affect anybody, certain groups like children, the elderly, pregnant women, and those with weakened immune systems are particularly vulnerable to these effects.
In a video game-turned-TV show, The Last of US, a fictional brain-altering fungus that wipes out humanity has been shown, many draw the fungus's parallel to it. This is also because, while it is not a known fact, however, the reality is fungi fungi-related deaths are at 5% globally.
What Did The Study Find?
Researchers have found that certain species of Aspergillus fungi are likely to expand into new regions of North America, Europe, China, Russia, and Asia as global temperatures rise.
The study—funded by the Wellcome Trust—used computer models and climate projections to map the future spread of Aspergillus strains, including A. flavus, A. fumigatus, and A. niger.
“Fungi are relatively under-studied compared to viruses and parasites, but our maps suggest fungal pathogens are likely to affect most regions of the world in the future,” study author van Rijn told CNN.
One of the key findings, reported by CNN, is that Aspergillus fumigatus could expand its range northward toward the Arctic. By 2100, it could spread 77.5% farther than it currently does, potentially putting around 9 million people in Europe at risk.
Aspergillus fumigatus thrives in warm, organic environments like compost, and it can grow “astonishingly quickly” at high temperatures, said Professor Elaine Bignell, co-director of the MRC Centre for Medical Mycology at the University of Exeter, in a comment to the Financial Times.
“Its natural lifestyle may have given A. fumigatus the resilience it needs to invade human lungs,” Bignell added.
CDC No Longer Recommends COVID Vaccine For Kids And Pregnant Women - What Do Experts Think?

(Credit-Canva)
The U.S. federal government has recently removed COVID-19 vaccines from the recommended list for healthy pregnant women and children. In an X post, the US health Secretary Robert F. Kennedy Jr., said that the Centers of Disease Control and Prevention (CDC) no longer recommends vaccine for “healthy children and healthy pregnant women”. He explains that the official stated that this decision gets the country "one step closer" to ‘Making America Healthy Again’.
To understand the implications of this, we spoke with experts, Dr. Shrey Srivastav, Consultant Physician at Sharda Hospital, and Dr. Arunesh Kumar, Director & HOD, Pulmonology, Paras Health who clarified some common concerns people were experiencing.
What This Means for Access to Vaccines
Dr. Srivastav points out that while the US may not recommend vaccines any longer, the World Health Organization (WHO), still advises vaccination for pregnant women. A few healthcare professionals have brought up their concerns regarding COVID vaccines, stating they do not think it is necessary to get COVID vaccines at the moment.
Dr. Srivastav adds that COVID vaccine is more important for pregnant women with co-morbidities, whether diabetes, hypertension, immuno-compromised or with pre-existing health concerns need the vaccine. Dr. Arunesh also points out the same, encouraging people to get vaccinated for COVID in case they have any such pre-existing conditions. However, Dr Sushila Kataria, Senior Director, Internal Medicine Medanta recommends people should wait for official recommendations from the government before getting vaccinated.
Also Read: Female Cancer Crisis On An Increase, Climate Change Could Be Responsible
RFK Jr. explained that the previous administration had pushed for more COVID shots for healthy children without enough clear data to support repeated booster shots for kids. This decision was made alongside other health officials. Food and Drug Administration Commissioner (FDA) Dr. Martin Makary and National Institutes of Health (NIH) Director Dr. Jay Bhattacharya, who called it "common sense" and "good science," noted that there's no evidence that healthy children currently need the vaccine.
Dr. Srivastav points out that there are many reviews and studies that say otherwise. “In my views many people still have doubts about COVID-19 vaccines for children. However, large studies published in PubMed and other indexed journals have shown that mRNA vaccines are safe and work well for kids aged 5 to 11.”
He continues to explain that for children aged 6 months to 4 years who have weakened immune systems, it's important that all their COVID-19 vaccine shots come from the same company, following the CDC's advice. This particular study was published in 2023 JAMA network, Dr. Srivastav explains the study, “10 million vaccinated children found fewer COVID infections, fewer symptoms, fewer hospital stays, and fewer cases of MIS-C. Mild side effects like sore arms and fever were common, but serious problems like heart inflammation were very rare.”
Is There Enough Evidence Supporting Vaccines?
“Yes, extensive research and monitoring have shown that COVID vaccines are safe for both healthy children and pregnant women.” Dr Arunesh explains that vaccines act as an extra protective shield, “In pregnancy, vaccination helps prevent severe illness and can also pass protective antibodies to the baby. For children, the side effects are typically mild and short-lived, such as arm soreness or fatigue.”
Before this change, the government had been recommending COVID-19 vaccines for almost everyone, including children and pregnant people. According to the Mayo Clinic even though children usually don't get very sick from COVID, some, especially very young ones, can. They also expressed how pregnancy increases the risk of severe COVID-19.
Dr. Srivastav added that research backs the safety and effectiveness of vaccines for pregnant women. “Research shows that COVID-19 vaccines are safe and effective for pregnant women. A large review of over 600,000 pregnant women found that getting vaccinated did not increase the risk of miscarriage, early birth, or stillbirth. In fact, vaccinated pregnant women were less likely to get COVID-19 or need hospital care because of it.”
11-Year-Old Dies From H5N1 Bird Flu In Cambodia, Country Records 100% Fatality Rate In All Human Bird Flu Cases

Credits: Health and me
A 11-year-old boy from Kampong Speu province in Cambodia has died of H5N1 avian influenza, the country’s Health Ministry confirmed. This marks the fourth confirmed human case of bird flu in Cambodia in 2025 and all four have been fatal.
Laboratory analysis performed at the Pasteur Institute of Cambodia confirmed the virus presence in the child, who had a sudden onset of serious respiratory manifestations such as high fever, continuous cough, breathlessness, and acute respiratory distress. He was taken to a hospital but died on May 2, 2025.
Also Read: CDC No Longer Recommends COVID Vaccine For Kids And Pregnant Women - What Do Experts Think?
The ministry's probe found that chickens and ducks in and around the child's house had been falling ill and dying in the days prior to the child's symptoms appearing, suggesting zoonotic transmission, a distressing reminder of the thin lines between human and animal well-being.
Although human illnesses of H5N1 are uncommon and not a food safety threat, this year has also witnessed an alarming increase in cases in the world. The World Health Organization (WHO) reported 10 human bird flu cases across the world in 2025 before this death in Cambodia. Five of them led to fatality. Four of those deaths have now been reported from Cambodia and all of them have been linked with direct contact with infected or dead birds.
This trend is mirroring an increasingly global reality: the rate of H5N1 spillover into humans, while remaining low, is rising. The more often it occurs, the greater the possibility of the virus evolving to be able to live in human hosts.
Also Read: Female Cancer Crisis On An Increase, Climate Change Could Be Responsible
Why the H5N1 Threat Can't Be Ignored?
Avian flu A(H5N1) is a contagious disease that primarily infects birds but has been found to be capable of crossing species. This cross-species capability keeps scientists and health authorities on their toes. The Global Virus Network just reported more than 70 cases of human infections in the U.S. alone since the wider outbreak started, with one confirmed death.
Although human-to-human transmission has not yet taken place, specialists warn that mutations, particularly in mammals, may bring us to the verge of a tipping point. Should H5N1 develop the potential for effective human transmission, the result might equal the magnitude of past pandemics.
After the child's death, Cambodia's Ministry of Health sent a team of emergency response workers to the village affected to track down the source of the infection and stop further transmission. Steps include contact tracing, health screening, dispensing of the antiviral drug Tamiflu to potentially exposed people, and public education campaigns alerting about contact with infected poultry.
In a public health alert, the ministry called on citizens who had flu-like symptoms—particularly those with recent contact with birds—to get immediate medical attention. "To delay treatment increases you to a high risk of eventual death," the warning added.
How Does H5N1 Infect Humans?
H5N1 is not contagious among humans, and that is why every confirmed case attracts immediate global attention. The majority of infections in humans are due to direct contact with sick birds or contaminated habitats, especially via saliva, nasal discharges, feces, or blood.
Even other creatures—like milk cows—can carry the virus in milk and respiratory secretions. When those things come in contact with humans, the virus enters through inhalation of contaminated dust or droplets, eyes, nose, or mouth.
Also Read: Can Drinking Alcohol Increase Your Risk Of Pancreatic Cancer? WHO Study Reveals Alarming Link
This cross-host transmission highlights the importance of adopting a One Health policy, which acknowledges the interrelatedness of human, animal, and environmental health.
Symptoms of Bird Flu In Humans To Watch For
Incubation for H5N1 in humans usually lasts for 2 to 5 days, although it may be as long as 17 days. Symptoms tend to worsen like normal flu but may quickly become severe respiratory illness. Typical symptoms are:
- High fever
- Fatigue and muscle pains
- Ongoing cough
- Nausea, vomiting, and diarrhea
- Sore throat
- Conjunctivitis (pink eye)
- Shortness of breath
While some of the U.S. cases have had less severe symptoms, around the world the virus has carried a high mortality rate, so early diagnosis and intervention are paramount.
The WHO has been warning of the pandemic threat posed by avian influenza for years. In the United States alone, over 168 million birds have been killed since 2022 to contain outbreaks of avian flu—testifying to the virus's economic and agricultural impact. But the more general concern is how close we may be to a mutation that makes possible efficient transmission from person to person.
The recent Cambodian fatality, though isolated, is just a piece in a larger mosaic. With H5N1 now emerging in an expanding array of animal hosts, including mammals such as mink, cats, and even sea mammals, the path to human adaptation may be shortening.
Who's Most at Risk Right Now?
According to the U.S. Centers for Disease Control and Prevention (CDC), the general public remains at low risk, but the agency recommends heightened vigilance among farmers, poultry workers, veterinarians, and dairy handlers. Preventive steps include:
- Avoiding contact with sick or dead animals
- Using protective gear (gloves, masks, eye protection)
- Practicing good hygiene—especially handwashing
- Cooking poultry and eggs thoroughly (to 165°F/74°C)
- Choosing pasteurized dairy products
India Records 1,010 Active Covid Cases, New Variants LF.7 & NB.1.8.1 Raise Concerns

Credits: Health and me
India, with the world's largest population and a frontline state in the war against Covid-19, is seeing a steady but significant increase in active cases. On May 27, 2025, the country had 1,010 active cases, with the majority of the cases in Kerala, Maharashtra, Tamil Nadu, and Karnataka. This recent upsurge coincides with the detection of two newly emerging subvariants—NB.1.8.1 and LF.7—both descendants of the Omicron lineage, raising cautious concern among public health experts and virologists.
Although numbers are still relatively low compared to previous peaks hence there is no need for panic, the appearance of new mutations and uneven booster uptake have pushed India back into the international Covid-19 spotlight. Here's what the resurgence says, what is currently known about the subvariants, and how it might affect global pandemic preparedness.
Also Read: CDC No Longer Recommends COVID Vaccine For Kids And Pregnant Women - What Do Experts Think?
India had 257 active cases on May 19. Within about a week, the number had passed 1,000, with Kerala contributing more than 400 of them and Delhi reporting over 100 cases. Maharashtra, which includes Mumbai, Pune, and Thane, remains a Covid hotspot, the Ministry of Health and Family Welfare reports.
The recent discovery of new strains, especially NB.1.8.1 in Tamil Nadu and LF.7 in Gujarat, also complicates the epidemiological scenario. The latest such confirmed case, that of a 55-year-old woman from Noida in Uttar Pradesh, is the first for that district in the current surge, underlining the slow but consistent dissemination of the virus across geographies.
What Are The New Covid Variants Currently Circulating?
The new-found sub-lineages NB.1.8.1 and LF.7 belong to the larger JN.1 Omicron lineage. Although these mutations have not yet been tagged as "Variants of Concern" by the World Health Organization (WHO), they are included in "Variants Under Monitoring"—a label for the mutations that can influence virus traits like transmissibility and potential for immune evasion.
Early investigations and genomic monitoring indicate that NB.1.8.1 possesses spike protein mutations like A435S, V445H, and T478I, which may make it more infectious and resistant to earlier immunity. LF.7 has also indicated capacity for partial immune evasion, while it is still premature to conclusively evaluate the clinical severity.
Dr. Arup Halder, Consultant Pulmonologist, CMRI Kolkata, provided essential insight, "As of May 2025, India is experiencing a modest but significant surge in COVID-19 cases. Though the majority of cases are still mild with low hospitalization rates, the increase is being fueled by newer sub-lineages of the JN.1 variant, namely LF.7 and NB.1.8, which are known to be highly transmissible and partially immunoevasive."
What's Driving the Rise in Covid-19 Cases?
A number of factors are driving the increasing trend:
Declining Immunity: Naturally, immunity from past infections or vaccination weakens with time, increasing the susceptibility of populations to reinfection. Immunocompromised people and older adults are most vulnerable.
Weather and Climate: The advance arrival of monsoon in most Indian states has brought with it rising humidity and unstable temperatures—both conducive to transmission of respiratory viruses like SARS-CoV-2.
Improved Testing and Reporting: Maharashtra and Kerala states have had strong genomic surveillance infrastructure, which has helped in the early identification of new variants.
"Maharashtra's high test positivity rate is also due to its population density, international transit points, and early exposure to previous pandemic waves", Dr. Halder added.
Vaccination and Booster Status
India has so far given over 2.2 billion Covid-19 vaccine doses. Experts have, however, raised red flags over the patchy uptake of booster shots, particularly among high-risk categories like the elderly and healthcare workers. The bivalent boosters are still available, but variant-specific shots remain unavailable in India.
"Although new variant-specific vaccines are not yet ready, current bivalent boosters continue to reduce symptomatic infections by 50% and severe disease by as much as 80%," said Dr. Halder. "It is important that high-risk individuals receive a booster dose immediately, continue to mask in crowded areas, and practice basic hygiene measures."
Across the world, there is increasing concern over access to vaccines. In America, health officials recently dropped Covid-19 vaccination for healthy kids and expectant mothers from the CDC's vaccination calendar on the grounds of requiring more comprehensive clinical trials. Experts are concerned that such limitations may impact global confidence in vaccines and booster campaign momentum in nations such as India.
The WHO is monitoring seven variants under consideration, among which are NB.1.8.1 and LF.7. None have been designated as Variants of Concern, but the agency continues to assess how they're evolving using global genomic data.
NB.1.8.1, which has been found in more than 22 countries, has demonstrated a consistent rise in share across the world. This suggests a possible competitive edge over other existing circulating strains—worth watching through genomic surveillance and public health readiness.
Should You Be Worried?
Though the ongoing Covid-19 wave in India is mild in severity and containable with available healthcare infrastructure, it comes as a timely reminder: the pandemic does not end. The virus still mutates, and any slip in surveillance, booster coverage, or public health messaging can lead to populations being susceptible to future waves.
Delhi has already advised the hospitals to make beds available, oxygen supplies, and medicines and vaccine stockpiles. States such as Kerala are taking localized containment measures in order to trace the spread and promote testing in high-risk areas.
© 2024 Bennett, Coleman & Company Limited

