- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
High-Dose Nimesulide Oral Medicines Banned By Centre Over Safety Concerns

Credits: Canva
The central government has announced a decisive regulatory move concerning nimesulide, a widely prescribed non-steroidal anti-inflammatory drug used to treat pain, fever, and inflammation. In an effort to protect public health, the Centre has barred the manufacture, sale, and distribution of oral nimesulide formulations that contain more than 100 mg of the drug. The restriction has come into force with immediate effect and applies across the country, as per NDTV.
The decision follows mounting safety concerns linked to high-dose oral preparations of the medicine. According to the official notification issued by the government, doses exceeding 100 mg may pose a risk to human health. The order also notes that safer and well-established alternatives are already available in the market. Given this, the authorities concluded that continuing the availability of high-dose nimesulide does not serve the public interest.
What Is Nimesulide and Why Is It Prescribed?
Nimesulide belongs to a group of medicines known as non-steroidal anti-inflammatory drugs, or NSAIDs. Doctors commonly prescribe it to manage acute pain, reduce fever, and relieve inflammation associated with conditions such as musculoskeletal injuries, dental pain, or post-surgical discomfort. The drug works by blocking substances in the body that cause pain and swelling, as per Mayo Clinic.
Despite its effectiveness in symptom relief, nimesulide has remained controversial for years due to questions surrounding its safety, especially when used in higher doses or for longer durations. While it continues to be prescribed in India under regulated conditions, its use has been closely watched by health authorities and medical experts.
Legal Basis for the Ban
The prohibition has been issued under Section 26A of the Drugs and Cosmetics Act, 1940. This provision allows the central government to restrict or ban drugs if they are found to be unsafe, ineffective, or harmful to patients. Before finalising the decision, the government sought the opinion of the Drugs Technical Advisory Board, or DTAB, which is the highest advisory body on technical matters related to drugs and cosmetics in India.
After reviewing available scientific data and expert input, the board supported the move, leading to the issuance of the nationwide ban on high-dose oral formulations, as per NDTV.
Safety Concerns and Global Position
Nimesulide has faced sustained scrutiny from regulators and healthcare professionals, primarily due to concerns about liver-related side effects. Several studies and post-marketing surveillance reports have linked the drug to cases of liver toxicity, particularly when used in higher doses.
The World Health Organization has not included nimesulide in its Model List of Essential Medicines, a key reference document that guides countries on priority medicines for basic healthcare needs. This exclusion reflects ongoing global caution around the drug’s safety profile. In fact, regulatory authorities in multiple countries have either restricted its use or removed it from the market altogether after reviewing reports of hepatic injury documented in WHO pharmacovigilance data.
Indian Regulatory Reviews and Safer Alternatives
In India, the Central Drugs Standard Control Organisation has reviewed the risk-benefit balance of nimesulide on several occasions. These reviews were prompted by both domestic data and international findings related to adverse effects. Medical experts in the country have consistently highlighted that alternatives such as paracetamol and ibuprofen offer a more reliable safety record when taken at recommended doses.
These commonly used pain relievers are backed by extensive clinical evidence and guidance from bodies like the Indian Council of Medical Research, which supports their use for pain and fever management under standard dosing protocols.
Superbug Fungus Candida Auris Is Spreading In The U.S., Check Where Cases Are Rising Fastest?
Credits: Canva
A dangerous superbug that does not respond to most antibiotics is spreading rapidly across the United States, with Alabama reporting 158 cases so far this year. The data, shared by the Alabama Department of Public Health, highlights growing concern among health officials as infections continue to rise in healthcare settings.
The organism, known as Candida auris, is a type of yeast or fungus that can lead to severe and sometimes life-threatening infections. According to the Centers for Disease Control and Prevention, the fungus is especially troubling because it can survive on human skin and hard surfaces for months, even after routine cleaning and disinfection.
Why Candida auris Is Hard to Control
Unlike many other infections, Candida auris can spread easily through shared medical equipment and direct contact between people. Its ability to withstand commonly used disinfectants makes it difficult to eliminate once it enters a healthcare facility.
State health officials say cases have increased every year, pointing to a steady and worrying trend. “Each year, we have seen increases in our case counts which underscores the need for sustained vigilance,” the Alabama Department of Public Health told AL.com.
Superbug Fungus Candida Auris: Nursing Homes Among the Worst Affected
Nursing homes and long-term care facilities are bearing the brunt of the outbreak. According to ADPH, these settings face a higher risk because residents often have weakened immune systems and require frequent medical care.
“At this time, the Alabama Department of Public Health’s primary concern is the potential for unrecognized transmission within and between healthcare facilities,” the department said. Officials fear that infections may spread silently before being detected.
Superbug Fungus Candida Auris: CDC Guidelines and State Response
The health department confirmed via email that it is following the CDC’s recommended containment strategy to limit further spread. Healthcare providers and laboratories in Alabama are voluntarily reporting cases, although the state’s figures are not currently listed on the CDC’s national tracking dashboard, as per USA Today.
Alabama is not alone in dealing with the superbug. Nearby states are also seeing significant numbers. CDC data shows Tennessee has reported 189 cases, Mississippi 108, and Georgia 377. Florida, like Alabama, does not yet have figures publicly listed on the CDC website.
Superbug Fungus Candida Auris: A Growing National Problem
Candida auris was first identified in 2009 and has become increasingly common since then. The CDC said the fungus was first detected in the United States in 2016, when 51 cases were reported. By 2020, that number had climbed to more than 700.
This year, the rise has been sharp. As of December 20, 7,046 cases have been reported nationwide. In 2025 alone, 28 states recorded infections, with Nevada reporting the highest number of cases.
Superbug Fungus Candida Auris: Symptoms and Health Risks
The fungus can infect different parts of the body, including the bloodstream, wounds, and ears. Symptoms vary depending on where the infection occurs and how severe it is. In some cases, people may not show symptoms at all.
The CDC noted that most patients who develop Candida auris infections are already seriously ill. This makes it difficult to determine how much the fungus contributes to death compared to other existing health conditions.
Superbug Fungus Candida Auris: Preventing Further Spread
ADPH stressed that stopping the spread will require strong coordination across healthcare systems. “Continued collaboration with healthcare partners, timely reporting, and adherence to recommended infection control practices are critical to preventing further spread and limiting outbreaks,” the department said.
Health officials say ongoing awareness, strict hygiene measures, and early detection remain the best tools to contain this growing threat.
Whooping Cough Deaths Rise in the US as Infections Stay Above Pre-Pandemic Levels

Credits: iStock
Whooping cough deaths are rising in the US, as the country sees a surge in the infection. So far, tens of thousands have been infected, with at least 13 people dead from the bacterial infection this year. While the infection rate is lower than last year it continues to remain above typical pre-pandemic years. The Scientific American reports that the number of deaths have also seen a rise.
What Causes Whooping Cough?
Whooping cough or what is scientifically known as the respiratory infection called pertussis is severe, and is characterized by violent cough. It could leave people, especially infants, struggling to breath. While it is rarely fatal, it can have lingering symptoms and thus have earned the name '100-day cough'. Whooping cough is caused by the bacterium Bordetella pertussis, which emits toxins into a person's respiratory tract. This is why early treatment with antibiotics vital to managing the infection. The bacterium is easily spread between people, through direct contact and droplets from mouth or nose. This is what makes it contagious.
According to the Centers for Disease Control and Prevention, the US and its territories recorded 27,871 confirmed cases of whooping cough as of December 20 this year. By the same point last year, cases had reached 41,922, marking a sharp rebound after four pandemic years when annual infections stayed below 10,000.
Also Read: What Is Candida Auris Infection? The Deadly Superbug Spreading In US
How Lethal Is Whooping Cough?
As of now, 13 people have died of pertussis this year. As per the report from the Pan American Health Organization, and provision CDC data from last year, 10 deaths were noted in 2024, while three increased in 2025.
Public health experts worry that persistently high whooping cough cases this year, following last year’s surge, may reflect falling vaccination rates. The DTaP vaccine protects infants and young children, while Tdap covers older children and adults. CDC guidelines recommend multiple doses starting at two months, yet only 79 percent of children born in 2021 had received four DTaP doses by age two.
Who All Can Get The Shot For Whooping Cough?
Whooping cough is most dangerous, especially among infants under a year old. Public health experts also recommended that pregnant people must get the Tdap vaccine to transfer the antibodies to newborns. All adults are also advised to get the Tdap vaccine in every 10 years to ensure a continued protection.
What Are The Common Symptoms Of Whooping Cough?
Early symptoms that can last for 1 to 2 weeks usually include:
- Runny or stuffed-up nose
- Low-grade fever (less than 100.4°F)
- Mild, occasional cough
CDC notes that later symptoms could be rapid, violent, and uncontrolled coughing fits. About one to two weeks after early symptoms begin, many people develop intense coughing spells, known as paroxysms. These fits typically last one to six weeks, but in some cases can continue for up to 10 weeks. As the illness progresses, the cough becomes more frequent and severe.
During these episodes, people may produce a high-pitched “whoop” when breathing in, vomit during or after coughing, feel extreme exhaustion, struggle to breathe, have trouble sleeping, or even fracture a rib. Many describe it as the worst cough they have ever experienced.
What Is Candida Auris Infection? The Deadly Superbug Spreading In US
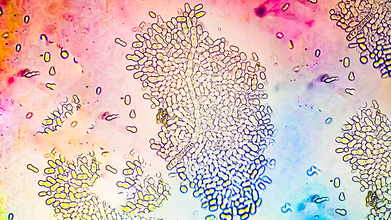
Credits: iStock
As 2025 ends, more and more people are falling ill. With a surge in flu cases, and mystery disease like adenovirus, thousands of people are already infected. Now, a deadly fungus, also considered a superbug due to its resistance to all types of antibiotics. This is Candida auris.
Also Read: What To Know About The Super Flu Surge In US; 'It Will Likely Get Worse', Say Experts
What Is Candida Auris? The Superbug Resisting All Antibiotics
It is a type of invasive year that can cause deadly infections in people, especially with weakened immune system. As of now, it has infected at least 7,000 people across 27 US states, confirmed the data from the Centers for Disease Control and Prevention (CDC).
The fungus can spread easily in healthcare settings, especially in hospitals and nursing homes. It is also spreading at an "alarming" rate, says CDC. The Hill reported that some strains of the fungus are troublesome because they are resistant to all types of antibiotics that are commonly used to treat fungal infections.
Due to fungus's resistance to antibiotics, it is becoming difficult to contain. As of now, more than half of the states have reported clinical cases of Candida auris in 2025. Another factor that makes it more dangerous is that standard lab tests cannot detect it. In a CDC press release, a CDC epidemiologist Dr Meghan Lyman said, "The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control."
Origins Of Candida Auris - The Superbug
This was first discovered in 2009 in Japan from the ear canal of a patient. Since then, it has spread to many countries, including India, where it was identified as a major public health threat in 2014.
Also Read: New Year's Eve Safety Tips, Fire Departments Across US Share Ways To Welcome 2026 Safely
Can Anyone Fight Off This Superbug?
Healthy people could possibly fight off this infection on their own. However, the population vulnerable could find it more difficult to fight off this deadly fungus. Melissa Nolan, an assistant professor of epidemiology and biostatistics at the University of South Carolina told Nexstar, "If you get infected with this pathogen that’s resistant to any treatment, there’s no treatment we can give you to help combat it. You’re all on your own."
Like the mystery disease, adenovirus, this fungus too can survive on surfaces, said Nolan. “It’s really good at just being, generally speaking, in the environment. So if you have it on a patient’s bed for example, on the railing, and you go to wipe everything down, if in whatever way maybe a couple of pathogens didn’t get cleared, then they’re becoming resistant. And so over time, they can kind of grow and populate in that hospital environment," said Nolan.
Is This Superbug Only Limited To The US?
Studies show that this superbug is not just limited to the US, but is spreading globally. It has already been found in at least 61 countries and on 6 continents. The study also found that the fungus is becoming more and more drug resistant, all due to its ability to switch from a yeast-like growth to a filament-driven spread. It also contains a cell wall that has proteins and makes it easier to stick on human skin "like glue". This is what enables it to colonize the human cells.
© 2024 Bennett, Coleman & Company Limited

