- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Higher-Pitched Voices Could Signal Imminent COPD Flare-Up- Key Symptoms To Watch For

A recent study has found that changes in a person's voice can predict an upcoming flare-up of chronic obstructive pulmonary disease (COPD). Researchers discovered that patients with COPD experience higher-pitched, breathy, or hoarse voices when an exacerbation is imminent. The study was presented at the European Respiratory Society (ERS) Congress in Vienna, Austria.
The findings offer a promising step toward early detection of COPD exacerbations through non-invasive methods. Researchers from Maastricht University Medical Center in the Netherlands, led by investigator Loes van Bemmel, conducted the study, which focused on using smartphone voice recordings to track changes in a patient’s voice.
These changes were correlated with the onset of a flare-up. If validated further, this could lead to the development of a smartphone app that would help patients manage their symptoms before they worsen.
The research involved 28 COPD patients who were asked to record their voices daily for 12 weeks using a smartphone app. They were required to say “aah” in one breath for as long as possible and either read a short paragraph or answer a question. In addition to recording their voices, participants completed daily questionnaires about their COPD symptoms. The study tracked 16 instances of symptom exacerbations during this period.
By analyzing the voice recordings, the research team observed clear changes in the patients’ voices just before a flare-up. Notably, patients’ voices became higher-pitched and more breathy or hoarse.
“There were clear differences between patients’ recordings on a normal day and on the first day of an exacerbation,” van Bemmel explained. These voice changes may serve as early markers of an exacerbation, allowing for timely intervention.
Chronic Obstructive Pulmonary Disease (COPD) Symptoms
COPD is a group of lung diseases that includes emphysema and chronic bronchitis, both of which hinder airflow to the lungs and make it difficult for sufferers to breathe. COPD is a serious, long-term condition, and the World Health Organization ranks it as the third leading cause of death worldwide.
Typical symptoms of COPD include:
- Difficulty breathing, especially during physical activities.
- A persistent cough that may produce mucus (sputum).
- A whistling sound when exhaling.
- A feeling of constriction or discomfort in the chest.
- Feeling tired or exhausted due to the body’s reduced ability to take in oxygen.
- Increased susceptibility to colds, flu, or other infections affecting the lungs.
COPD flare-ups, or exacerbations, can be life-threatening if not treated early. These flare-ups can lead to hospitalization and increase the risk of death. However, early treatment significantly reduces these risks, highlighting the importance of detecting exacerbations before they progress.
The researchers are already looking into ways to apply their findings in real-world settings. Plans are underway to develop a smartphone app that will use speech signals to detect COPD flare-ups. “This would enable patients to manage these events themselves at home,” van Bemmel said. The app, tentatively named SPEAK, will be co-developed with COPD patients to ensure it meets their needs.
Professor Frits Franssen, Secretary of the ERS assembly on respiratory clinical care and physiology, emphasized the potential impact of this technology. He noted that COPD exacerbations, if caught early, can prevent serious health complications.
Franssen added that the smartphone-based voice analysis could provide a quick and efficient way to alert patients and doctors that treatment is needed. “Because it works via a smartphone, voice analysis could be used by anyone, at any time and anywhere. This could ultimately save money, time, and patients’ lives.”
While these findings are promising, researchers caution that larger studies are needed to confirm the results. If successful, speech analysis could become a vital tool in managing COPD and potentially other respiratory diseases, helping improve patient outcomes through early detection and intervention.
Had COVID? Your Next Flu Could Reactivate Dormant Breast Cancer Cells, Researchers Warn
Credits: Canva
Breast cancer survivors have lived with a guarded sense of relief. Even after beating the disease, the possibility of recurrence remains a faint shadow but new research has raised an alarming possibility- respiratory viruses, including common ones like influenza and SARS-CoV-2, may act as a catalyst, reawakening dormant breast cancer cells that linger quietly in the lungs long after remission.
In a new study published in Nature, researchers from the University of Colorado and Utrecht University have found that viral infections can reignite cancer’s flame literally. Dormant cancer cells are like the embers left in an abandoned campfire, and respiratory viruses are like a strong wind that reignites the flames.
This study marks a crucial turning point in how we understand long-term remission and highlights the importance of continued vigilance among cancer survivors.
Why COVID-19 Infection Is First Red Flag?
The investigation kicked off in the aftermath of the COVID-19 pandemic. Clinicians and researchers began to notice an uptick in metastatic cancer cases, especially among individuals previously in remission. Something wasn’t adding up. Cancer recurrences were occurring at an unusual rate and too often to be dismissed as coincidence.
The researchers turned to two key data sources: the UK Biobank and a large U.S. breast cancer database with over 37,000 patient records. In the UK Biobank cohort, survivors who had contracted COVID-19 exhibited a twofold increase in cancer-related mortality. In the U.S. dataset, those with prior SARS-CoV-2 infection faced a more than 40% increase in metastatic breast cancer, particularly in the lungs.
The extent of this increased risk is almost unheard of in cancer epidemiology, it’s a significant effect.
What’s Happening in the Body?
To understand the mechanics, the researchers turned to mouse models—long used as reliable proxies for studying human disease behavior. When the mice with previously dormant breast cancer cells were infected with either SARS-CoV-2 or influenza A, it took only days for those latent cells to wake up. Within two weeks, there was a more than 100-fold increase in metastatic tumor burden in the lungs.
Here’s the crucial insight, the cancer cells didn’t reawaken because the virus directly interacted with them. Instead, the viruses triggered an inflammatory immune response, rich in signaling proteins called cytokines—especially interleukin-6 (IL-6). This cytokine storm appeared to create an environment ripe for dormant cancer cells to start proliferating again.
According to lead researcher Shi Chia from the University of Colorado, “Although species differences warrant caution in interpreting mouse data… collectively, these findings underscore the substantial metastatic risk COVID-19 posed to cancer survivors.”
Role of Viruses in Cancer Biology
The link between viruses and cancer isn’t new. Human papillomavirus (HPV) has long been known to cause cervical and other cancers. The Epstein-Barr virus (EBV) has been implicated in several types of lymphoma. In fact, EBV has been found in five times higher concentrations in breast cancer tissue compared to healthy tissue.
The idea that viruses could influence cancer development or recurrence has been around since the 1930s, particularly in mouse models. But this new research is among the first to show how non-oncogenic, respiratory viruses—those not traditionally associated with cancer—might still play a key role in its resurgence.
Role of Inflammation and the Immune System
One of the most compelling parts of the study is the insight into how the immune system's response, not the virus itself, may be the real driver of cancer recurrence.
After remission, it’s common for a few cancer cells known as dormant disseminated cancer cells (DCCs), to remain hidden in tissues like the lung, bone, or liver. These DCCs are typically inactive, posing no threat unless triggered.
Inflammatory responses to infections, especially those that involve cytokines like IL-6, appear to disturb this dormancy. In simple terms, inflammation acts like a wake-up call for these sleeping cells.
The researchers demonstrated that only when the viral infections resulted in elevated levels of inflammatory markers did the dormant cells awaken. This opens up new avenues for therapeutic research focused on blocking inflammation, rather than targeting cancer cells directly.
What This Means for Breast Cancer Survivors?
This is not a reason for panic but it is a call for caution. As DeGregori explains, “If you are a cancer patient who has these dormant cells, you may end up living a normal life and dying with these dormant cells, instead of dying because those dormant cells awakened. But if you get a respiratory virus like influenza or COVID, your chance of dying from those dormant cells awakening is much greater.”
Millions of breast cancer survivors around the world, many of whom are years or even decades into remission—could unknowingly carry dormant cells. For them, a common respiratory illness may no longer be just an inconvenience; it may be a risk factor for relapse.
Could Vaccination Be Protective?
Can we reduce this risk with vaccines? It’s too early to say definitively, but the idea is promising. If viral infections act as a trigger, then preventing infection might, in turn, prevent relapse.
DeGregori’s team is now exploring whether flu and COVID-19 vaccinations could lower the likelihood of dormant cell reactivation. This would have wide-ranging implications not just for cancer survivors, but for public health policy as a whole.
The idea that a respiratory virus could reignite cancer long after remission is unsettling but not entirely surprising. As science continues to unravel the complex relationship between our immune system, viruses, and cancer, this study offers one clear message:
Remission isn’t always the end and staying healthy may mean more than avoiding recurrence it could mean avoiding infection altogether.
Legionnaires Outbreak: All That You Need To Know About The Disease That Killed 1 And Left 22 Sick In New York
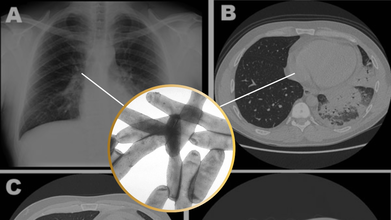
Credits: Canva
With 6,000 cases of Legionnaires reported annually in the United States, scientists still think it is underdiagnosed as it could be hard to distinguish from other kinds of pneumonia or respiratory issues.
As of now, New York City has fallen prey to Legionnaires' disease outbreak. At least 22 people have fallen ill, and one person has been declared dead in Harlem, as per the New York City Health Department.
The Reason Of This Spread
As per the city health officials, people became ill after breathing in bacteria sprayed from cooling tower in central Harlem. Cooling towers help regulate building temperature. The city health department also said in a news release on Wednesday that it was testing cooling towers in the area and are continuously investigating the outbreak.
What Is The Legionnaire's Disease?
As per the Centers for Disease Control and Prevention (CDC), Legionnaire's disease is a serious type of pneumonia that is caused by Legionella bacteria. This bacteria is known for causing two types of diseases, one of them being Legionnaire's disease, a severe form of pneumonia; while the other one is Pontiac fever, which is a mild illness that can include fever, muscle aches and headaches.
It is very rare that this bacteria can cause infection outside of the lungs and affect heart or wound infections, notes CDC.
Common Symptoms
Legionnaires' disease symptoms usually develop 2 to 14 days after exposure to Legionella bacteria, but it can take longer.
The symptoms of Legionnaires' disease are similar to other types of pneumonia.
Symptoms include:
- Cough
- Fever
- Headaches
- Muscle aches
- Shortness of breath
Other symptoms, such as confusion, diarrhea, or nausea can also occur.
After this outbreak, which has been linked with a cluster, the deputy commissioner of division of infectious diseases at the New York City Department of Health and Mental Hygiene, Dr Celia Quinn, said that the risk is low for most people, however, there could be additional cases linked with this cluster.
Legionnaire's Disease in the US
Cases have been steadily rising over the past two decades. While there isn’t a single known cause for this increase, experts believe several factors may be contributing, including aging water infrastructure, poor system maintenance, rising water temperatures, and improved disease tracking and awareness.
Outbreaks are more common during the warmer months, particularly summer, when more buildings rely on cooling towers for air conditioning systems.
Health professionals note that while a similar report in winter might raise fewer concerns, the combination of summer heat and rising case numbers highlights the importance of staying vigilant during peak Legionella season.
Who Are At Risk?
While most healthy people exposed to the bacteria do not get sick, people who are 50 or older, or are current or former smokers, or people with a weakened immune system or chronic conditions, such as cancer, lung disease, diabetes or kidney and liver failure may be at a higher risk.
Legionnaires’ disease often becomes more severe within the first week of symptoms. In serious cases, patients may need hospitalization and oxygen support. If the illness progresses, it can lead to complications like lung failure or heart damage. According to the CDC, about 1 in 10 people who contract Legionnaires’ disease do not survive.
Is It Contagious?
Legionnaires’ disease doesn’t spread from person to person. It’s usually contracted by breathing in mist or vapor contaminated with the bacteria. Outbreaks are often linked to cooling towers in large cities. In rare instances, the illness can also be caused by inhaling contaminated soil.
Justin Timberlake Reveals Lyme Disease Diagnosis: Here’s What That Means For His Health

Credits: IMDb and Canva
After wrapping up a two-year long world tour, pop icon Justin Timberlake, 44, opened up about a private health battle that’s been affecting him behind the scenes. In a heartfelt Instagram post shared on Thursday, the singer revealed that he has been diagnosed with Lyme disease, a tick-borne illness that can cause lingering and unpredictable symptoms.
The announcement came just one day after the conclusion of his tour in Istanbul, marking the end of a musical chapter that spanned more than 70 performances across North America, Europe, and South America.
Diagnosis Behind the Scenes
Timberlake disclosed that during his Forget Tomorrow World Tour, which promoted his sixth solo album Everything I Thought It Was, he had been quietly “battling some health issues.”
“When I first got the diagnosis, I was shocked for sure,” Timberlake wrote. “But at least I could understand why I would be onstage and in a massive amount of nerve pain, or just feeling crazy fatigue or sickness.”
He admitted that the symptoms forced him to reconsider continuing the tour, saying, “I was faced with a personal decision. Stop touring? I decided the joy that performing brings me far outweighs the fleeting stress my body was feeling.”
Despite the physical toll, Timberlake pushed through his JT LIVE 25 tour leg, which included festival performances like Lollapalooza Brazil, before finally wrapping things up on July 31.
What Is Lyme Disease?
Lyme disease is caused by bacteria transmitted to humans through the bite of an infected black-legged tick. It's most common in certain parts of North America and Europe, especially during the warmer months.
The most common early sign of Lyme is a red rash that often resembles a bull’s-eye, typically appearing within 3 to 30 days after the bite.
The Center for Disease Control and Prevention (CDC), US, notes that the early symptoms can also mimic the flu, fever, chills, headache, fatigue, and muscle aches. If caught early and treated with antibiotics, most people recover completely within a few weeks.
However, for some, like Timberlake, symptoms can persist or worsen even after treatment. This condition, sometimes called Post-Treatment Lyme Disease Syndrome (PTLDS), includes ongoing fatigue, nerve pain, cognitive issues, and more.
“Lyme can be incredibly tricky because its symptoms overlap with many other conditions,” explained Dr. Christopher Bazzoli, an emergency medicine expert at the Cleveland Clinic, as reported by the New York Times. “When it’s not caught early, it can lead to a wide range of complications, from joint pain to neurological issues.”
In some untreated or severe cases, complications can include:
- Chronic fatigue
- Arthritis
- Heart palpitations
- Dizziness or shortness of breath
- Nerve pain
- Memory or concentration problems
- And in rare instances, meningitis
Doctors are still researching why some people recover quickly while others experience long-term effects. For now, treatment usually includes rest, medications for symptom relief, and in some cases, extended antibiotic therapy.
Timberlake has now joined a growing list of celebrities, including Avril Lavigne and Shania Twain, who’ve opened up about their experiences with Lyme disease in hopes of raising awareness.
Takeaway For You: If you’ve spent time in wooded or grassy areas and experience unusual fatigue, joint pain, or rashes, it’s worth getting checked for Lyme. Early diagnosis can make all the difference.
© 2024 Bennett, Coleman & Company Limited

