- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Hulk Hogan, The Wrestling Legend, Dies From Cardiac Arrest At 71
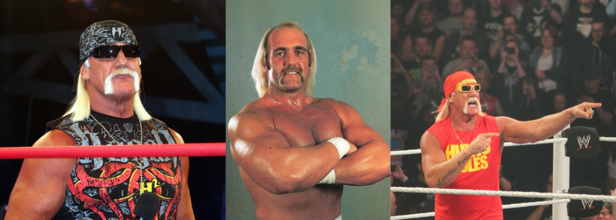
Credits: Wikimedia Commons
Hulk Hogan, the wrestling legend has passed away at the age of 71, according to a report by TMZ Sports. Emergency services were reportedly dispatched to his Florida residence following a 911 call for a suspected cardiac arrest.
TMZ also reported that a video outside Hogan's residence show that the responders had tried to desperately save him while he was being transported to an ambulance. The clip shows that several paramedics were, what it seems like, conducting compression as Hogan was being wheeled to the emergency vehicle.
Hogan's death comes just weeks after his wife publicly denied rumors that the WWE Hall of Famer was in a coma, reassuring fans that his heart was “strong” and that he was recovering well after multiple surgeries.
Widely credited with transforming professional wrestling into a mainstream global phenomenon, Hogan—born Terry Bollea—was more than just a wrestler. With his signature bandana, handlebar mustache, and larger-than-life personality, he became a household name in the 1980s and 1990s, helping to usher in an era when wrestling became part of pop culture.
What Happens During Cardiac Arrest?
Jonathan Chrispin, MD, from John Hopkins Medicine, writes, that a cardiac arrest, also known as a sudden cardiac arrest, in when the heart stops beating suddenly. The lack of blood flow to the brain and other organ can cause a person to lose consciousness, become disabled or die if not treated immediately.
Is cardiac arrest the same as a heart attack? The answer is no, as per the Heart Organization, a heart attack occurs when blood flow to the heart is blocked, whereas in a cardiac arrest, heart suddenly stops beating.
What Are The Symptoms Of A Cardiac Arrest?
In some cases of cardiac arrest, there may be no symptoms at all. You may experience these symptoms prior to cardiac arrest:
- Fatigue
- Dizziness
- Shortness of breath
- Nausea
- Chest pain
- Heart palpitations (fast or pounding heart beat)
- Loss of consciousness
What Causes A Cardiac Arrest?
Common Causes of Cardiac Arrest:
Arrhythmia and Ventricular Fibrillation
Arrhythmia refers to an irregular heartbeat caused by disrupted electrical signals in the heart. One of the most dangerous types is ventricular fibrillation—a rapid, chaotic heartbeat in the ventricles. Instead of pumping blood effectively, the heart quivers, leading to sudden cardiac arrest.
Enlarged Heart (Cardiomyopathy)
Cardiomyopathy occurs when the heart muscle becomes enlarged—either dilated or thickened—resulting in weak or abnormal heart contractions. This condition increases the risk of heart failure and cardiac arrest.
Coronary Artery Disease (CAD)
CAD is caused by plaque buildup that narrows and hardens the coronary arteries, restricting blood flow to the heart. If untreated, it can lead to arrhythmias or heart failure—both of which can trigger cardiac arrest.
Other Potential Causes of Cardiac Arrest
- Severe blood loss
- Valvular heart disease (damage or defects in the heart valves)
- Lack of oxygen (such as from drowning or choking)
- Electrolyte imbalances, particularly high levels of potassium or magnesium, which can disrupt heart rhythm and lead to arrhythmia
Early diagnosis and timely medical intervention are critical in preventing these conditions from progressing to cardiac arrest.
US Weighs China Travel Warning As Chikungunya Cases Near 5,000: Report

Credits: Canva
The United States Centers for Disease Control and Prevention (CDC) is assessing a potential travel notice for China following a sharp rise in cases of chikungunya, a mosquito-borne viral infection that has sparked public health alarms in southern China, as reported by the Independent and the South China Morning Post.
Nearly 5,200 infections have been reported in the Guangdong province since early July, with most of them concentrated in the city of Foshan. Health officials there have since escalated their emergency response to a level III alert, which signals a “relatively major” public health threat in China’s four-tier system.
While the CDC has not yet published a formal advisory, a spokesperson told The Independent that the agency is “aware of the reported chikungunya outbreak in Guangdong Province in China and is currently assessing the size and extent of the outbreak.”
What is chikungunya?
Chikungunya is a viral infection transmitted by the bite of an infected Aedes mosquito, the same mosquito species responsible for dengue and Zika. Symptoms typically include sudden onset of fever and joint pain, but may also include headache, muscle pain, swelling, and rash.
Although most cases are mild and self-limiting, some infections can lead to prolonged joint pain or, in rare cases, long-term complications. Serious outcomes are more likely among those with pre-existing health conditions. There are no antiviral treatments available, so prevention, particularly mosquito control and bite avoidance, remains the primary approach.
Vaccines against chikungunya have recently become available and are recommended for travelers to high-risk areas, although they are not yet widely accessible.
According to local health authorities in Foshan, around 95% of reported cases have been mild, with patients recovering within a week. However, the outbreak’s rapid spread has raised concern among international health bodies.
Global spread and WHO alert
The outbreak in China follows a global pattern of chikungunya resurgence. The World Health Organization (WHO) issued an alert last week warning of the risk of the virus repeating its global spread from two decades ago. Diana Rojas Alvarez, a medical officer with WHO, said that nearly 5.6 billion people across 119 countries live in areas where the virus could potentially spread.
Chikungunya was first identified in 1952 in Tanzania and has since been detected in more than 110 countries, including major outbreaks in India, Italy, and the Americas. The virus is not spread from person to person; instead, it is carried by mosquitoes that have fed on infected individuals and then pass it to others.
The concern is not just local: international travel plays a key role in how the virus crosses borders. Infected travelers returning to or visiting countries with mosquito populations capable of transmitting the virus can trigger new outbreaks.
China’s response: Mosquito control and surveillance
The first case in this outbreak was reported in Foshan’s Shunde district on July 8 and was believed to be imported. Since then, local and national health authorities have moved quickly to contain the spread.
Measures taken include the use of drones to detect rooftop water accumulation, the release of larva-eating fish into lakes, and widespread public awareness campaigns. Residents have been urged to eliminate standing water, install window screens, and wear protective clothing.
Hospitals in affected areas have increased bed capacity for confirmed cases and designated specialized treatment centres. Border controls have been stepped up in Hong Kong to prevent imported cases from mainland China, with expanded testing capabilities introduced at key entry points.
CDC travel warnings: What it means for travelers
The CDC’s travel health notices are used to inform travelers about global disease risks and provide precautionary guidelines. The warning system has four levels, ranging from “practice usual precautions” (Level 1) to “avoid all travel” (Level 4).
As of now, China has only a Level 1 travel health notice for measles. However, the CDC has issued Level 2 notices for chikungunya in several countries including Bolivia, Kenya, and Madagascar in recent months.
If the CDC decides to escalate China’s status, it would be a significant development, both in terms of travel planning and diplomatic perception.
US–China tension and public health
The potential issuance of a travel notice also comes against the backdrop of complex US–China relations. While the CDC’s move would be grounded in public health data, the optics of a travel warning could have broader implications.
On Thursday, Chinese foreign ministry spokesperson Guo Jiakun responded to the reports, saying that China is in communication with the WHO and “making every effort to ensure a safe environment for travelers.”
The WHO has not issued any travel restrictions related to the outbreak but continues to monitor the situation closely.
A word of caution for travelers
With mosquito-borne diseases on the rise globally, driven by climate change, urbanization, and increased mobility, health experts advise travelers to stay informed and take preventive measures.
“Mosquito control is key,” said an official from the Hong Kong Centre for Health Protection. “Simple actions like using insect repellent, sleeping under mosquito nets, and avoiding stagnant water can go a long way in preventing infection.”
As global health agencies monitor the chikungunya outbreak in China, travelers to affected areas should remain vigilant and stay updated with official advisories. Prevention remains the best protection in the face of a disease with no cure.
World Alopecia Day 2025: Theme, Origin, And Significance

Credits: Canva
August is known as the Hair Loss Awareness Month and the first Saturday of this month is known as the International Alopecia Day.
Hair loss is a common concern, affecting over 85% of men, 55% of women, and between 15–38% of adolescents at some point in their lives. For those with advanced or long-lasting alopecia, the emotional and social impact can be profound.
Baldness has been linked to significant declines in mental health and quality of life, with higher rates of anxiety, depression, stress, and reduced self-esteem.
What Is Alopecia?
It is a term used for hair loss that affects the scalp or even the entire body, temporarily or permanently. Alopecia can happen due to variety of reasons, including heredity, hormonal changes, and medical conditions, or as simple as normal aging.
Aim of Alopecia Day
The day aims to form a community of those who experience this autoimmune disease.
Origin of International Alopecia Day
International Alopecia Day was initiated by American activist Lynn W. Walker in 2011. She herself lives with a diagnosis of alopecia totalis and created this day to unite people with similar experiences, reduce stigma, and highlight beauty and strength regardless of the presence of hair.
Theme of Alopecia Day 2025
This year's theme as per Alopecia UK is, 'Strength in Numbers', which urges more and more people to join the International Alopecia community and to do away with the shame of hair loss and form a support group, across the world.
Alopecia And Its Kinds
As per the National Library of Medicines, US, alopecia refers to the loss or absence of hair in areas where it normally grows. It can be localized or widespread, temporary or permanent, and affects people of all ages and genders. As a symptom with diverse underlying causes, alopecia is generally categorized into two main types: nonscarring (the most common) and scarring (cicatricial).
For many patients, hair loss leads to significant emotional distress and a reduced quality of life. Accurate diagnosis requires a thorough history, physical examination, and targeted investigations to identify the root cause and guide effective treatment. Managing alopecia can be challenging, but this overview outlines key assessment and treatment approaches for the most common forms to support better outcomes.
Forms of alopecia
There are several main types of alopecia, including:
alopecia areata: an autoimmune disease that causes hair loss, often in small, round patches on the scalp, but it can occur anywhere on the body
alopecia totalis: complete loss of scalp hair
alopecia universalis: hair loss over the entire body
androgenetic alopecia: hereditary baldness
Ways You Can Participate In International Alopecia Day
- Learn and share knowledge about alopecia
- Participate in activities for Alopecia Day
- Embrace the symbol by wearing blue
- Share you story to build a support group
- If you are a doctor, you can also advocate for the right alopecia treatment
- Contribute financially to alopecia research and awareness groups
- Volunteer to help spread alopecia awareness
- Raise voice against bullying, as many people are bullied due to their hair loss
CDC Data Flags Alarming Rise In Childhood Vaccine Exemptions, Here's Why Doctor's Are Worried

Credits: Canva
For the 2024–25 school year, the United States has recorded its highest percentage of kindergartners with vaccine exemptions—4.1%, or roughly 138,000 children. This new data from the Centers for Disease Control and Prevention (CDC) follows a worrying trend that’s gained momentum since the COVID-19 pandemic disrupted routine immunizations. With measles outbreaks on the rise and herd immunity slipping, pediatricians and public health experts are asking a pressing question: what happens when vaccine complacency meets misinformation?
According to the CDC’s most recent report, vaccine exemptions for kindergartners have jumped more than a full percentage point over the last four years. Nearly all of these exemptions are classified as nonmedical, which means they’re granted for religious or personal reasons—not for health-related concerns.
Exemptions increased in 36 states this school year, and in 17 states, more than 5% of kindergartners have opted out of one or more required vaccinations. That’s a critical problem for public health officials, as it creates fertile ground for vaccine-preventable diseases to return.
Measles—a disease that was declared eliminated in the U.S. in 2000—is making a grim comeback. So far in 2025, there have been 1,333 measles cases in 39 states, the highest number recorded in more than three decades. CDC officials note that most of these cases are among unvaccinated children.
Why does this matter? Because measles is one of the most contagious viruses on the planet. To prevent outbreaks, at least 95% of a community needs to be vaccinated. In the U.S., however, MMR (measles-mumps-rubella) vaccine coverage has dropped to 92.5%—the fifth year in a row it’s fallen below the federal target.
The effects of declining trust in vaccines, what concerns me most is that we’re playing with fire, and children will get burned.
While several variables contribute to vaccine hesitancy, some experts point to political shifts at the federal level. Dr. Besser specifically criticized Health and Human Services Secretary Robert F. Kennedy Jr., a long-time vaccine skeptic, for what he believes is a growing culture of doubt and fear around childhood immunizations.
While these numbers are bad, they don’t even begin to reflect the impact that Secretary Kennedy will have on future exemptions.
In response, HHS spokesperson Andrew Nixon stated, “Vaccination remains the most effective way to protect children from serious diseases like measles and whooping cough,” adding that the decision to vaccinate “is a personal one.”
That last line is what’s worrying public health experts—many of whom believe the public needs firmer messaging in favor of vaccinations, not neutrality.
What’s Causing the Decline?
Beyond political rhetoric, a few key factors are contributing to the rise in exemptions:
Pandemic Disruption: Children born around 2020 missed well-child visits during lockdowns, leading to gaps in scheduled vaccinations.
Misinformation: Social media platforms continue to amplify vaccine myths, often unchecked.
Policy Loopholes: Forty-five states allow religious exemptions, and 15 states permit personal or philosophical exemptions. In some places, the process to opt out is easier than completing immunization requirements.
Complacency: Because vaccines have worked so well historically, many parents no longer see the diseases they’re meant to prevent—and underestimate their risks.
Vaccines are often victims of their own success, once you stop seeing disease, people forget why we needed protection in the first place. Here’s what the latest CDC data reveals about vaccine coverage among kindergartners during the 2024–25 school year:
MMR (Measles-Mumps-Rubella): 92.5% vaccinated (down from 92.7%)
DTaP (Diphtheria-Tetanus-Pertussis): 92.1%
Polio: 92.5%
Total kindergartners lacking MMR documentation: 286,000
This is far below the 95% coverage goal set by HHS to prevent disease spread.
Why Are Experts Calling for Urgent Action?
The American Academy of Pediatrics has reiterated its position, nonmedical exemptions should be eliminated. Public health leaders argue that making vaccine refusal easy puts the entire population at risk—especially children too young or medically unable to be vaccinated.
“There’s a growing body of evidence that where it’s easy to get an exemption, exemption rates go up,” said a 2019 study by health policy researchers. “Removing personal-belief exemptions leads to fewer kids being left unprotected.”
Several states are now reconsidering their policies. However, in others, new legislation may make it even easier to opt out. For instance, one state is introducing an online affidavit form that parents can print at home without needing any medical consultation.
What’s at Stake?
This year’s outbreak has already led to three deaths and dozens of hospitalizations, mostly in unvaccinated children. And the worst may still be ahead. If the trend of rising exemptions continues, experts fear a resurgence of diseases like polio, whooping cough, and chickenpox—diseases that once caused widespread suffering and death before vaccines became available.
Vaccination is not just a personal choice—it’s a public responsibility. The recent CDC data serves as a warning. If exemptions continue to rise, the U.S. could see the return of once-eradicated diseases on a larger scale.
© 2024 Bennett, Coleman & Company Limited

