- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
In An Extremely Rare Surgery, Doctors Remove Fetus From A 1-Year-Old Baby's Brain
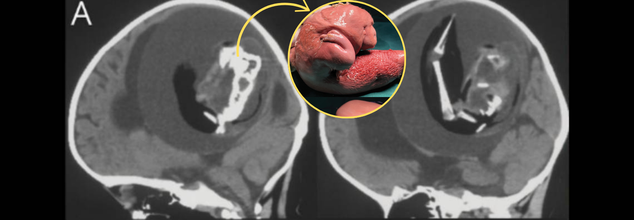
Image Credits: Journal Neurology
In a case that has left the medical community stunned, Chinese doctors successfully extracted a fetus from the brain of a 1-year-old boy. This very rare condition, "fetus in fetu," is when one twin gets engulfed by the other early in fetal development. Most fetus-in-fetu cases are discovered in the abdomen, but this case, where absorption into the brain occurred, is almost unheard of.
The parents of the young girl obtained medical care after they observed that she was developing delayed motor skills and had an abnormally large head circumference. Physicians found an abnormal growth in her skull, which was subsequently diagnosed as a malformed twin. The condition is estimated to happen in only 1 in 500,000 live births, making it a rare occurrence in the history of medicine.
Fetus-in-fetu is a situation where one twin gets trapped within the other in early embryonic development. It happens when identical twins do not fully separate and one embryo gets enclosed within the other. Usually, the engulfed twin does not develop, but the host twin develops normally.
Here, the mass in the infant's brain was a "monochorionic diamniotic twin," which means that the two fetuses initially shared the same placenta but existed in distinct amniotic sacs. In most cases, identical twins completely separate from each other, but in exceptionally rare instances such as this, unseparated blastocysts (early-stage embryonic cells) can result in one twin being imprisoned within the other. As the host embryo grows, it can wrap around the captive twin, incorporating it into its body structure.
Physicians concluded that removal of the parasitic twin by surgery was mandatory to ensure the baby's well-being. Scans of the brain indicated that the deformed fetus had a vertebral column, leg bones, and even the embryonic beginnings of arms and fingers. It also showed spina bifida, where the spinal cord is exposed because of the insufficiency of growth of the tissue around it.
The fetus was about 10 centimeters long and was trapped in a fluid-filled sac inside the child's head. With the unprecedented nature of such a case, medical experts were confronted with an untested challenge of conducting the delicate operation. The operation was completed successfully, excising the fetal mass without any reported complications, although the child's post-operative status has not been made public.
What is Fetus-in-fetu Condition?
Fetus-in-fetu can be confused with a teratoma, another tumor type which also involves undifferentiated tissue such as hair, teeth, and bone. Fetus-in-fetu differs, however, in that it is the result of a real twin instead of abnormal cellular development. Fetus-in-fetu is identified most commonly based on the formation of a vertebral column and internal structures which imply fetal development.
The fact that the fetal twin was found within the brain indicates that the condition presumably occurred during a developmental stage of neural plate folding. This step is important to the development of the brain and spinal cord. If a parasitic twin were trapped at this time, then it could get integrated into the forming nervous system, as noted in this scenario.
Genome-wide sequencing verified that the fetal mass was genetically equivalent to the surviving twin, further establishing its status as a malformed identical twin instead of a tumor.
Although fetus-in-fetu has been previously reported, cases in which the brain is involved are rare. Perhaps one of the earliest recorded instances occurred in 1982 when a 6-week-old infant underwent surgery to have a parasitic twin removed from inside its skull. That fetus was 14 centimeters long and had formed limbs, a torso, and a head.
The rarity of such cases makes them highly significant for medical research. Understanding how and why fetus-in-fetu occurs can provide insights into early fetal development and the mechanisms that lead to identical twinning. Additionally, these cases highlight the importance of early medical intervention when developmental abnormalities are detected in infants.
These cases underscore the need for prenatal and postnatal medical examinations. Early diagnosis by the use of sophisticated imaging technologies like MRI and CT scans may identify such anomalies early enough to prevent them from causing life-threatening complications.
Though much is yet to be discovered about fetus-in-fetu, this case will remain a vital point of reference for all future medical research. It also makes one more aware of the intricacies of fetal development and the unusual conditions that can develop as a result of anomalies in early cell division.
The excision of a malformed twin from the brain of a 1-year-old is a milestone in pediatric neurosurgery. It highlights the wonders of contemporary medicine and the need for ongoing research to comprehend unusual congenital conditions. With advancing medical science, these findings will make early diagnosis and treatment options more effective for future cases of this nature.
WHO Recommends Tongue Swabs For Faster Tuberculosis Diagnosis, Curbing Transmission

Credit: Canva
In a significant breakthrough for faster diagnosis of tuberculosis -- the world’s most infectious disease --, the World Health Organization (WHO) has recommended tongue swab tests.
The new recommendations come as many people with TB do not produce sputum, but are contributing to transmission. The swab tests may not only expand access to testing but also enable early and timely treatment that can help break chains of TB transmission.
The updated guidance also includes recommendations for the use of near point-of-care molecular tests - the nucleic acid amplification tests (NPOC-NAATs) for drug-resistant TB and pooling of sputa as a diagnostic strategy for the initial detection of TB and drug resistance.
“The WHO has just issued recommendations on new near-point-of-care (NPOC) tests for the diagnosis of #TB; easy-to-collect tongue swab samples to expand access to testing; & a cost-saving sputum pooling strategy to increase testing efficiency for TB & RR-TB,” Tereza Kasaeva, Director - WHO department on HIV, Tuberculosis, Hepatitis, in a post on social media platform X.
“These new recommendations mark a major step toward making #TB testing faster and more accessible,” she said, while calling on countries to roll out the guidelines to close diagnostic gaps.
What Are Tongue Swabs
Tongue swabs are new, readily available, and easy-to-collect specimens for use with NPOC-NAATs and low-complexity automated NAATs (LC-aNAATs) for the initial detection of TB, with and without drug resistance.
The global health body recommends using the low-complexity automated NAATs as initial diagnostic tests in adults and adolescents with signs and symptoms of lung TB.
However, in cases where respiratory samples such as sputum (expectorated or induced), tracheal aspirate, and bronchoalveolar lavage (BAL) cannot be obtained, tongue swabs may be used as initial diagnostic tests for TB.
Tongue swabs may be collected by trained personnel or self-collected with guidance from trained personnel.
Dr Rakesh PS, from the International Union Against Tuberculosis and Lung Disease (The Union), in a LinkedIn post mentioned individuals having no or minimal symptoms, and often cannot present respiratory specimens.
"Tongue swabs offer a practical way to include this otherwise “missed” group in the diagnostic pathway. By enabling testing of individuals who would otherwise be excluded, tongue swab–based testing can enhance the efficiency of active systematic screening," Dr. Rakesh said.
"Tongue swabs are a strategic alternative when obtaining a respiratory specimen is difficult or not possible -- and, when used appropriately, they can strengthen our fight against TB," he added.
What Are NPOC-NAATs
NPOC-NAATs are swab-based molecular tests for TB detection that can produce results from a primary sputum or tongue swab sample in less than one hour. These tests use instruments that can be battery-operated and do not require specialized infrastructure for use or storage.
The tests can be done in basic peripheral laboratories, such as those that perform smear microscopy, and health clinics, mobile units, or community sites that do not have laboratories.
They can be performed by health care workers with basic technical skills because they do not require laboratory methods like precision pipetting.
What Is Sputa Pooling
In sputum pooling, samples from several individuals are mixed and tested together. It is a proven strategy to improve testing efficiency and reduce costs in resource-constrained environments.
Global TB burden
While being preventable and curable, TB remains a top infectious killer, with an estimated 10.7 to 10.8 million new cases and 1.23–1.25 million deaths in 2024, as per WHO.
The infectious disease disproportionately affects low- and middle-income countries.
While TB incidence rates have shown a slight, uneven decline since 2015, the overall burden remains high, with 30 countries accounting for 87 percent of global cases, led by India, Indonesia, China, the Philippines, and Pakistan.
Why Are NHS Doctors Choosing To Work Independently?

Credits: Representational Image (Canva)
An increasing number of the National Health Service or the NHS UK doctors are now choosing to practise privately. This has happened at the backdrop of mounting pressures and burnout that reshaped the landscape of general practice in England. According to a recent BBC report on Care Quality Commission (CQC), data found a sharp rise in doctors registering to work outside the NHS.
In the five years to the end of 2025, the CQC received 1,238 new registrations for "independent consulting doctors" in England. This is a 212 per cent increase as compared to 396 doctors registering to work independently over the five years. Between 2024 and 2025, registrations rose by 58 per cent.
Independent consulting doctors provide care privately, either in person or online, across a range of specialties including general practice, skin conditions, women’s health and aesthetics.
"You Don't Have Time To Go To The Toilet"
Dr Yvonne Girgis-Hanna is among those dividing her time between NHS and private practice. Speaking to the BBC, she said full-time NHS work had become unsustainable.
“I could not work as a full-time NHS GP,” she said. “The days I do in the NHS, the next day I'm totally wiped out… You might have 30 face-to-face contacts, then extra telephone calls and paperwork. You just don't have time to even go to the toilet.”
She now sees private patients in Essex, charging from £129 for a 20-minute appointment, with options of up to an hour. Longer consultations, she told the BBC, allow for continuity of care reminiscent of the “cradle to grave” model that once defined family medicine.
Demand, she argues, is the central strain on NHS general practice. With practices receiving roughly £120 per patient annually, frequent attenders can stretch resources thin. “If you imagine £120 for somebody that might be presenting 20 times, it is very little,” she said.
Patients Pay For Time And Familiarity
A 2024 LaingBuisson report noted that 13 per cent of GP consultations were private, which is up by 3 per cent two decades ago. This is because, some patients want faster access and longer appointments. Vanessa Ravazzotti, 51, told BBC that NHS wait worsened her symptoms and heightened anxiety. This is when seeing a private GP felt "mentally better". "She knows me; I know her."
Ian Miller, 85, who has arthritis, told the BBC he found short NHS appointments difficult and disliked seeing different clinicians. Private care offered familiarity and focus: “You immediately get down to the problem.”
Greater Autonomy, But Less Affordability
Dr Karen Benson, who works privately from a pharmacy in Hertfordshire, said the environment is calmer. “I haven't got constant interruptions… it's a much more relaxed atmosphere." She said she is better able to offer longer appointments and address the root cause of the illness. However, some patients switch back to NHS for specialist referrals that they cannot afford privately.
Dr Oliver Denton of the British Medical Association (BMA) told the BBC that while it is difficult to pinpoint a single cause, “with growing pressures within the NHS it is no wonder more may be considering looking to work outside the health service.”
Meningococcal B Vaccine Ineffective In Preventing Gonorrhea In Gay And Bisexual Men: Study
Credit: Canva
The meningococcal B vaccine (4CMenB) is completely ineffective in preventing gonorrhea -- a sexually transmitted infection (STI) --, especially among high-risk groups like gay and bisexual men, according to the results of the world’s largest randomized control trial (RCT).
Gonorrhea is a common bacterial STI caused by the bacterium Neisseria gonorrheae, and is transmitted through unprotected sex.
Even as antimicrobial resistance in gonorrhea has increased rapidly in recent years, Australian researchers explored the efficacy of 4CMenB against the disease.
The large randomized, placebo-controlled trial involving 587 gay and bisexual men showed that the risk of gonorrhea incidence remains essentially the same even after vaccination.
“Across both arms, the gonorrhea incidence was virtually the same -- at around 48 per cent per year, indicating very clearly that the vaccine had no effect on preventing gonorrhea,” said Professor Kate Seib, from Griffith University, in Australia, who led the trial.
In light of the study, the researchers stressed the need to explore other options to combat gonorrhea, such as condoms and regular testing.
The 4CMenB Vaccine
While meningococcal disease (caused by Neisseria meningitidis) and gonorrhea (caused by Neisseria gonorrhoeae) are distinct infections, both are caused by Neisseria bacteria, which share 80-90 percent genetic material.
The bacterium N. meningitidis primarily causes meningitis and septicemia, and observational studies have shown that meningococcal B (MenB) vaccines such as the 4CMenB offer 33-40 percent cross-protection against gonorrhea.
However, the latest study, presented at the Conference on Retroviruses and Opportunistic Infections in Denver, US, found no protection against gonorrhea.
The study “provides strong evidence that the 4CMenB meningococcal vaccine is not effective at preventing gonorrhea in gay and bisexual men who are at high risk of contracting it,” Seib said.
According to the US National Institute of Health, the 4CMenB vaccine is a highly effective, protein-based vaccine designed to protect against invasive meningococcal disease (IMD) serogroup B.
Approved in over 50 countries, it offers 71-95 percent effectiveness in infants and 100 percent in adolescents.
What Is Gonorrhea
Gonorrhea is a common STI, and sexually active people of any age can get the disease and pass it on to partners, and even to their baby during childbirth.
Gonorrhea is the second most common STI caused by bacteria, just behind chlamydia.
As per data from the World Health Organization (WHO), in 2020, there were an estimated 82.4 million new infections among adults globally.
The NIH noted that nearly 1 million new gonorrhea infections occur in the United States every year. About half of these infections occur in people ages 15 to 24.
The symptoms of Gonorrhea in men include:
- White, yellow, or green discharge from the penis
- Pain or burning (possibly severe) when peeing
- Testicular pain and swollen testicles.
Notably, the condition also occurs in women, but up to 50 percent of them won’t experience symptoms. This increases the risk of spread to other partners.
- Common symptoms in women include:
- Unusual vaginal discharge (white or yellow).
- Pain in your lower abdomen or pelvis.
- Pain during sexual intercourse
- Pain when you pee
- Bleeding between periods
© 2024 Bennett, Coleman & Company Limited

