- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Influenza Raises Heart Attack Risk By 6X– Here's Another Reason To Get Your Flu Shot

Each year, millions brace for the flu season, armed with cough drops, hand sanitizers, and the age-old debate- should I get the flu shot? While many associate influenza with little more than a fever and fatigue, mounting research suggests the consequences could be far more severe. A new study has added a significant warning to the mix: contracting the flu could increase your risk of a heart attack by six times in the week following infection.
A heart attack, or myocardial infarction, occurs when blood flow to the heart muscle is abruptly cut off, often due to a blood clot. While risk factors like smoking, high cholesterol, and obesity are well-known contributors, seasonal influenza now emerges as a stealthy but significant trigger, particularly in those already vulnerable.
This link isn't new. For years, scientists have warned that viral infections can increase cardiovascular risk. However, this latest data provides one of the clearest pictures yet. Researchers evaluated 401 patients who had a heart attack within a year before or after a confirmed flu diagnosis. Alarmingly, 25 heart attacks occurred in the first seven days following influenza infection.
How Influenza Triggers Heart Conditions?
Influenza does more than inflame the lungs — it can inflame the arteries, too. When the virus attacks, the immune system responds with inflammation. In people with existing plaque buildup in their arteries, this inflammation can weaken plaque stability, making it more likely to rupture. Once ruptured, the body reacts with clot formation, blocking blood flow and causing a heart attack.
In some cases, the flu virus may also increase blood coagulation, further raising the risk of clot formation. “When people get influenza or the flu, it taxes your body and puts a lot of stress on all of the other systems,” explains Dr. Susan Rehm, an infectious disease specialist at the Cleveland Clinic.
The study, led by Dr. Annemarijn de Boer and conducted using data from 16 diagnostic labs across The Netherlands, confirms what many health professionals have long suspected. It found that patients who suffered a heart attack after getting the flu were at significantly higher risk of mortality with 35% dying within a year of their flu diagnosis.
“While it isn’t clear from our results if those with less severe flu are also at risk, it is prudent for them to be aware of the link,” Dr. de Boer notes. The findings will be presented at the European Congress of Clinical Microbiology and Infectious Diseases.
How Can A Flu Shot Protect Against Potent Cardiac Condition?
Perhaps the most actionable takeaway from this research is simple- get your flu shot. For years, influenza vaccination has been recommended primarily for its ability to reduce flu-related complications, especially among vulnerable populations like the elderly, children, and those with chronic conditions.
Now, cardiologists and infectious disease experts are urging people especially those with cardiovascular conditions to think of the flu vaccine as an indirect heart attack prevention tool.
A study conducted by the Glasgow Institute of Cardiovascular and Medical Sciences found that heart attack patients who received the flu vaccine within 72 hours of their first event had a 50% lower risk of death from a subsequent heart attack. “Flu puts stress on your arteries and makes your blood thicker, so if you have heart disease, it could tip you over the threshold,” said Professor Naveed Sattar of the Institute.
The data is clear: flu shots save more than just lungs — they may save hearts. Consultant cardiologist Professor Martin Cowie of the Royal Brompton Hospital supports this proactive approach. “This is interesting and could be relatively easy to implement in general practice,” he notes. With flu vaccine supplies already stocked by national health systems, including the NHS, implementing flu shots as part of post-heart attack care could be done swiftly and effectively.
Long-Term Heart Health
While influenza vaccination is a crucial tool, long-term heart health requires broader lifestyle changes. Coronary heart disease is the most common cause of heart attacks is primarily driven by modifiable risk factors: high-fat diets, inactivity, smoking, high blood pressure, and obesity.
One form of preventive care gaining renewed interest is cycling. A recent study published in the journal Sports Medicine found that individuals who cycle regularly especially for commuting or errands were 23% less likely to die prematurely. Just 130 minutes of cycling per week can significantly reduce the risk of cardiovascular disease.
As flu season approaches, getting vaccinated should be considered not just a personal choice but a cardiovascular strategy. The six-fold increase in heart attack risk following influenza infection is a sobering statistic — especially for those already living with heart disease.
Non-Communicable Diseases Driving More Deaths in India With Women Facing Highest Risk, Says Lancet Report

Credits: iStock
While most of the world is experiencing fewer deaths from chronic disease, India is heading in the opposite direction. The Lancet's latest analysis reveals non-communicable disease such as diabetes, cancer, and heart disease are shortening more lives—particularly among women. The statistics don't simply provide data, they tell a tale of lifestyle changes, unequal healthcare access, and who bears the largest burden.
A recent paper in The Lancet has shed new light on a disconcerting Indian trend: deaths due to non-communicable diseases (NCDs) are increasing, even as the remainder of the globe experiences improvement. These results indicate a pressing public health threat, with women shouldering the highest burden.
During 2010-2019, the majority of the globe experienced a decline in deaths due to long-term conditions like heart disease, diabetes, and some cancers. Indeed, about 80 percent of nations witnessed a fall, enhancing survival for millions. But India defied this. The research monitored 185 nations and determined that deaths from NCDs went down globally, but India saw a dramatic rise.
For men, the probability of dying from an NCD between birth and age 80 rose from 56 percent in 2001 to nearly 58 percent in 2019. For women, the picture was starker. After a modest decline between 2001 and 2010, mortality rates surged in the following decade. By 2019, the likelihood of an Indian woman dying from an NCD before turning 80 was 48.7 percent, compared to 46.7 percent in 2001.
Why Women Are at Higher Risk?
Whereas men gained advantages in the case of some disease categories like chronic obstructive pulmonary disease (COPD), heart disease, and cirrhosis of the liver, women did not experience gains in most of these categories. Apart from marginal increases in COPD, cirrhosis, and remaining NCD categories, women's mortality risks deteriorated across the board. This indicates increasing gender inequality in access to healthcare, screening, and treatment.
What Are Non-Communicable Diseases?
NCDs, also referred to as chronic diseases, are chronic conditions that unfold gradually. They consist of cardiovascular diseases (heart disease and strokes), cancers, chronic lung diseases such as COPD and asthma, diabetes, and neuropsychiatric diseases. NCDs, as reported by the World Health Organization (WHO), are responsible for 71 percent of total deaths globally. Remarkably, almost three-quarters of premature NCD deaths—deaths that occur before the age of 70—occur in low- and middle-income nations such as India.
The Alarming Case of Lung Cancer in India
A specific trend in lung cancer was emphasized by the Lancet report. Worldwide, lung cancer death decreased among men in 92 percent of nations. But India, Armenia, Iran, Egypt, and Papua New Guinea followed the opposite trend. This highlights India's peculiar susceptibility to lifestyle influences like excess tobacco use, air pollution, and late diagnosis.
Globally, lower deaths due to cardiovascular diseases and certain cancers led to most of the reduction in NCD mortality. However, this achievement was countered by increasing deaths from dementia, liver and pancreatic cancers, and alcohol use disorders. According to the study, although clinical advances such as improved diabetes and hypertension medication, cancer screening, and better emergency treatment of heart attack saved many countries, not all populations were equally exposed.
Why India Is Trailing Behind from the World?
Various structural issues seem to account for India's deteriorating performance. The report cited that the health data quality from India is "very low," which made it more difficult to monitor, prevent, and treat NCDs properly. Meanwhile, disparities in access to medicines, screenings, and preventive care continue to be widespread.
This was also fueled by the 2008 global recession. Its long shadow cut short health budgets and global health aid. Growing poverty, employment insecurity, and inadequate access to healthy foods also intensified inequalities in health. The poor, as well as vulnerable populations—usually women, the old, and poorer communities—were disproportionately hit.
Risk Factors Fueling NCDs
NCDs are highly interrelated with environmental and lifestyle determinants. They are largely driven by tobacco smoking, alcohol consumption, unhealthy diet, and physical inactivity. In India, these are added to by urbanization, air pollution, and unequal access to health care. Social determinants of health, where individuals are born, live, and work, further determine their exposure to the risk factors.
Experts say that it will take systemic transformation to turn around India's NCD burden. Majid Ezzati, lead author of the study and professor at Imperial College London, urged huge investments in healthcare infrastructure, along with tobacco and alcohol control campaigns. These interventions, already proved effective elsewhere in the world, could save millions of lives if successfully adopted in India.
The Lancet report gives a straightforward message: while large parts of the world are set to limit premature deaths from non-communicable diseases, India is in danger of being left behind. Women are especially hit with overly high risks that reflect underlying social and health inequalities.
It will take a two-pronged response—better short-term access to NCD treatments and addressing upstream determinants such as tobacco smoking, unhealthy diets, and air pollution. It also calls for improved monitoring and improved healthcare systems to ensure all groups of people enjoy the benefits.
Scientists Behind Life-Changing Cystic Fibrosis Treatment That Extends Life By Decades Win Medical ‘Nobel’ Prize
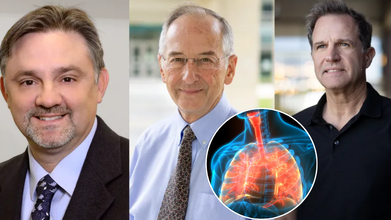
Three scientists whose groundbreaking work redefined the future of cystic fibrosis (CF) care have been awarded one of the world’s most prestigious honors in medicine: the Lasker-DeBakey Clinical Medical Research Award. Often referred to as the “American Nobel,” the award recognizes contributions that radically improve human health. This year, it went to Dr. Michael Welsh of the University of Iowa, Paul Negulescu of Vertex Pharmaceuticals, and Jesús (Tito) González, now of Integro Theranostics.
Together, their decades of research led to the creation of Trikafta, a therapy that has extended the lifespan of cystic fibrosis patients by decades and fundamentally reshaped what it means to live with the disease.
When cystic fibrosis was first described in the 1930s, it was considered a fatal childhood condition. Patients rarely survived past elementary school. Even as late as the 2010s, before Trikafta’s approval in 2019, half of patients with CF died before the age of 40.
Today, the outlook is dramatically different. Children born with CF between 2020 and 2024 who have access to Trikafta now face a median survival age of 65 years — nearly indistinguishable from the general population.
As Dr. Eric Sorscher of Emory University explained in The New England Journal of Medicine, “Available projections suggest that health and longevity may increase further as modulators begin to be administered at younger ages.”
This shift marks one of the most profound turnarounds in modern medicine.
The Role of the CFTR Gene
Cystic fibrosis is caused by mutations in a single gene: CFTR (cystic fibrosis transmembrane conductance regulator). The gene is critical for regulating the movement of ions across cell membranes, which in turn ensures proper water balance in tissues.
In healthy cells, CFTR forms channels that allow ions to flow freely. But in CF, the mutated gene produces faulty channels. The result is thick, sticky mucus that clogs the lungs and digestive system, fuels recurrent infections, and damages organs over time.
Dr. Michael Welsh, a pulmonologist and molecular biologist, helped illuminate the exact ways the most common CF mutation, delta-F508, disrupts cell function. He discovered two problems: the defective protein often gets “trapped” inside cells before reaching the surface, and even when it does reach the surface, it underperforms.
In a pivotal experiment, Welsh showed that simply lowering the temperature of cells allowed the trapped protein to move correctly. “That meant it was not totally broken,” he later recalled — a crucial realization that opened the door to correcting the defect.
Meanwhile, as a postdoctoral researcher in Nobel laureate Roger Tsien’s lab, Jesús (Tito) González developed a real-time system to track ion movement across membranes. Initially designed to study neurons, this tool proved invaluable for testing whether new drugs could restore CFTR function.
Negulescu and the Push to Find a Therapy
At Vertex Pharmaceuticals, Paul Negulescu helped drive the systematic search for compounds that could repair CFTR defects. Guided by Welsh’s molecular insights and González’s imaging system, the team screened thousands of molecules. The result was Trikafta, a triple-drug therapy that addressed the underlying cause of CF for most patients.
'Trikafta' Of Game-Changer in CF Treatment
Approved by the FDA in 2019, Trikafta combines three drugs — elexacaftor, tezacaftor, and ivacaftor — that work synergistically to help defective CFTR proteins fold correctly, reach the cell surface, and function effectively. The impact has been extraordinary. Since its introduction:
- Hospitalizations for lung infections have plummeted.
- The need for lung transplants has declined.
- Patients report stronger lung function, weight gain, and dramatically improved quality of life.
- For many families, the treatment has meant that milestones once unimaginable — graduating college, starting families, living into retirement — are now within reach.
Recognition at the “American Nobels”
The Lasker Awards, founded in 1945, celebrate biomedical achievements that shape the future of health. They are considered one of the highest honors in science, often predicting future Nobel Prizes.
The recognition of Welsh, González, and Negulescu underscores the profound impact of their work. The $250,000 prize, while symbolic compared to the billions Trikafta has generated, highlights the ethical and humanitarian dimension of their achievement: turning a once uniformly fatal disease into a chronic, manageable condition.
What CF Treatment Means for Medicine?
The CF breakthrough is not just about one disease. It represents a paradigm shift in genetic medicine. By targeting the root molecular defect rather than simply managing symptoms, Trikafta has become a model for other genetic conditions, from sickle cell disease to rare metabolic disorders.
It also illustrates the power of partnerships between academic researchers, biotech innovators, and patient foundations. The Cystic Fibrosis Foundation’s early investments in research were critical to advancing the work that ultimately led to Trikafta’s approval.
While Trikafta has transformed care in wealthy countries, challenges remain. The therapy is expensive — with an annual price tag of over $300,000 in the U.S. — putting it out of reach for many patients globally.
Furthermore, a subset of CF patients with rare genetic mutations still do not benefit from the drug, leaving an urgent need for alternative therapies. And as with all long-term treatments, researchers must continue monitoring for side effects and resistance.
Roughly 100,000 people worldwide live with cystic fibrosis. For decades, their lives were defined by daily medical regimens, frequent hospitalizations, and shortened lifespans. Today, thanks to the pioneering work of Welsh, González, and Negulescu, those same patients are looking toward futures filled with possibility.
FDA Approves Inlexzo For Bladder Cancer: Could This End Organ Removal Surgery?

Credits: iStock
The US Food and Drug Administration (FDA) has granted approval to Inlexzo (gemcitabine intravesical system) for the treatment of certain types of bladder cancer. This decision marks a milestone for patients with Bacillus Calmette-Guérin (BCG)-unresponsive, non-muscle-invasive bladder cancer (NMIBC), particularly those living with carcinoma in situ (CIS), with or without papillary tumors.
Unlike systemic therapies, Inlexzo works through a novel drug-releasing intravesical system designed for extended local delivery of gemcitabine into the bladder. For patients who wish to preserve their bladder and avoid radical surgery, the approval opens a long-awaited alternative.
Bladder cancer is the sixth most common cancer in the United States, disproportionately affecting older adults. Patients with NMIBC often start with BCG immunotherapy, the gold standard treatment. While many respond well initially, a significant proportion develop resistance or fail to sustain remission.
For these patients, the only widely recommended option has been radical cystectomy—a surgery to remove the bladder. Though effective, the procedure carries high risks, including a 3–8 percent post-surgical mortality rate, long recovery periods, and significant impact on quality of life. Many older patients are either unfit or unwilling to undergo the operation.
What this really means is that patients who have exhausted BCG therapy have been left with limited, often life-altering choices. Inlexzo offers a chance to delay or avoid bladder removal while still pursuing effective treatment.
The FDA’s approval was based on results from the SunRISe-1 phase 2b trial, a single-arm, open-label study. Findings showed:
- 82 percent of patients achieved a complete response following treatment.
- 51 percent of those maintained their response for at least a year.
Dr. Sia Daneshmand, principal investigator of SunRISe-1 and a urologic oncologist at the University of Southern California, emphasized the significance of these results, “I see many patients that ultimately become BCG-unresponsive and often face life-altering bladder removal. In my experience, Inlexzo is well tolerated and delivers clinically meaningful results. This will change the way we treat appropriate patients that haven’t responded to traditional therapy.”
Such durability of response signals a meaningful step forward in NMIBC care, particularly for patients for whom cystectomy is not feasible.
What Is Non-Muscle-Invasive Bladder Cancer (NMIBC)?
NMIBC represents a subset of bladder cancers confined to the inner lining of the bladder wall. It is categorized as low, intermediate, or high risk, depending on tumor size, multiplicity, and the presence of CIS. Approximately 10 percent of NMIBC patients are diagnosed with CIS, a flat but aggressive form of cancer that requires close management.
The reliance on BCG has long been the standard of care, but when patients become unresponsive, treatment options have been scarce. Radical cystectomy has remained the fallback. The approval of Inlexzo helps close a treatment gap that has persisted for decades.
How Inlexzo Works?
Inlexzo is not a traditional infusion or oral drug. It uses a drug-eluting intravesical system, placed inside the bladder during a short, office-based procedure. It does not require general anesthesia and begins releasing gemcitabine immediately, maintaining extended exposure directly to the bladder tissue. This approach is significant for two reasons:
- It keeps the chemotherapy localized, limiting systemic exposure.
- It allows for continuous therapeutic action without repeated, invasive interventions.
- For many patients, this translates into a treatment that is not only effective but also easier to tolerate and less disruptive to daily life.
Risks, Safety, and Limitations
While Inlexzo is a major advancement, it is not without risks. The FDA has issued clear precautions:
- Patients with bladder perforations or compromised bladder lining should not receive Inlexzo, as systemic exposure to gemcitabine may cause severe reactions.
- Delaying cystectomy in patients with persistent CIS could increase the risk of progression to muscle-invasive or metastatic bladder cancer, which is often lethal.
- MRI safety is limited to specific conditions, requiring close adherence to guidelines.
Reproductive risks include embryo-fetal toxicity and potential male infertility, based on animal studies. Women are advised to avoid pregnancy during treatment and for at least a week after device removal.
The most common side effects include urinary frequency, infections, bladder irritation, and blood in the urine. Serious adverse events occurred in 24 percent of patients, with 1.2 percent experiencing fatal outcomes, though these were rare.
Is This System A Patient-Centered Shift in Bladder Cancer Care?
Bladder cancer disproportionately impacts older adults—72 percent of patients in the SunRISe-1 study were over 65 years old. For this group, surgery carries heightened risks. Inlexzo’s approval gives clinicians a new tool to help manage NMIBC without immediately resorting to bladder removal.
As Dr. Daneshmand noted, this drug-delivery innovation may change the treatment landscape by filling a crucial gap in care. For patients who have exhausted BCG and face limited choices, Inlexzo offers hope for improved survival and quality of life.
Inlexzo’s approval is a win not only for patients but also for the field of urologic oncology. The drug’s placement under Johnson & Johnson’s portfolio signals strong industry investment in localized, bladder-preserving therapies.
Experts caution, however, that long-term follow-up studies will be essential to fully understand Inlexzo’s durability, risks, and potential role in combination with other therapies. For now, the FDA’s decision gives patients an urgently needed option that bridges the gap between immunotherapy failure and radical surgery.
© 2024 Bennett, Coleman & Company Limited

