- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Joe Biden Is Diagnosed With Aggressive Prostate Cancer: All That You Need To Know

Credits: Wikimedia Common and Canva
Former US President Joe Biden's office confirmed on Sunday that he has been diagnosed with prostate cancer. Earlier, a small nodule was found in his prostate gland, however, not much had been revealed about his medical evaluation.
It was last week when Biden went to see the doctors after urinary symptoms and prostate nodule was found. He was then diagnosed with prostate cancer on Friday, and the cancer cells have spread to the bone.
“While this represents a more aggressive form of the disease, the cancer appears to be hormone-sensitive which allows for effective management," his office said. "The President and his family are reviewing treatment options with his physicians.”
How Is the Aggressiveness Of Prostate Cancer Graded?
The aggressiveness of prostate cancers is graded on the basis of Gleason scores. These scores range between 2 to 10, with 8,9,and 10 behaving more aggressively. Biden's office confirmed that his score was 9, suggesting that his cancer is the most aggressive.
The Gleason score works on the basis of the lower scores indicating slower growth and spread, and higher scores suggesting more aggressive disease.
Like Biden's cancer cells have spread to his bones, it is common for prostate cancer to spread to other parts of the body, especially to bones. Metastasized cancer is more difficult to treat than localized cancer because it's challenging for medication to reach every tumor and eliminate the disease entirely.
However, in cases like President Biden’s, where prostate cancer relies on hormones to grow, treatments that block or reduce hormone levels can be effective in targeting the tumors.
Dr Matthew Smith of Massachusetts General Brigham Cancer Center told the US News, "It is very treatable, but not curable. Most men in this situation would be treated with drugs and would not be advised to have either surgery or radiation therapy."
At the age of 82, Biden's health has been a topic of concern. During his presidency, he had a 'cancerous' skin lesion removed from his chest. In February 2023, the White House in a statement said that the skin tissue was removed and after biopsy it was revealed to be cancerous.
How Common Is Prostate Cancer In Men?
As per the American Cancer Society, about 1 in 8 men will be diagnosed with prostate cancer during their lifetime. The National Institutes of Health notes that 50% of men between 70 to 80 years of age also showed histological evidence of malignancy.
While it is not clear what causes prostate cancer, healthcare professional have often found that age, obesity and a family history of prostate cancer could increase the chances of being diagnosed with it.
What Happens In Prostate Cancer?
As per Urology Care Foundation, prostate cancer develops when abnormal cells form and grow in the prostate gland. Not all abnormal growths, also called tumors, are cancerous. Some are benign growth and are not life threatening. They also do not spread to nearby tissue or other parts of the body.
Whereas cancerous growths can spread to nearby organs and tissues, as in the case of Biden.
What Have Been The Reaction On Biden's Diagnosis?
The current US President and a long time opponent Donald Trump posted on social media that he was saddened by the news and "we wish Joe a fast and successful recovery."
Kamala Harris also posted on social media that she was keeping him and in her family's "hearts and prayers during this time." She wrote: "Joe is a fighter — and I know he will face this challenge with the same strength, resilience, and optimism that have always defined his life and leadership."
Delhi Pollution Is A Major Health Hazard, Toxic Air Could Even Cause Organ Damage, According To Doctors

Credits: PTI and Aqi.in
As of 8am, in Delhi, the city's average AQI stands at 513 according to aqi.in. Major pollutant in the Delhi's air include PM2.5, PM10, Carbon Monoxide, Sulfur Dioxide, Nitrogen Dioxide, and Ozone. The AQI is equivalent to smoking 11.8 cigarettes per day, 82.6 cigarettes per week, and 354 cigarettes in a month. Amid this, doctors have called this major public health hazard, and warned people about the damage it can cause to our organs.
"The smaller the particle the more dangerous it is because it really goes into the depth of our lungs and causes damage there," says Dr. Vivek Nangia, Vice Chairman and Head of Pulmonology at Max Healthcare Saket, as told to news agency PTI.
Speaking to news agency ANI, Dr. Naresh Trehan, MD, Medanta, called the current situation “a major, major health-wise hazard,” stressing that the impact is unfolding across all age groups.
“A disaster for humanity,” says Dr Trehan
According to Dr. Trehan, pollution is now causing illness “many fold,” with outpatient departments packed with people suffering from cough, cold, chest congestion, asthma attacks, and severe breathing difficulties. But his biggest concern goes beyond the lungs.
He explained that the particulate matter present in polluted air moves far deeper into the body than most people realise. “These particulates go everywhere,” he told ANI. “They get absorbed into the blood, they go to your brain, they go to your kidneys, they go to your liver.”
Dr. Trehan added that the chronic effects of such constant exposure are making the public “sicker than they would be if they were living in a cleaner area.” Children, he warned, face an even greater threat as trapped toxic gases and particulate matter during winter behave “like a gas chamber,” potentially harming neurological development.
Dr Nangia breaks down the danger of PM2.5
Giving the scientific context behind this damage, Dr Nangia told PTI that the toxicity varies by particle size.
Particles larger than 5–10 microns usually stay in the upper respiratory tract, causing symptoms like throat irritation, watery eyes, and a runny nose. However, “a particle size less than 2.5 microns goes into the lungs,” he explained. Even more dangerous are particles smaller than 0.5 microns, which “go directly into the bloodstream from the lungs and trigger an inflammatory cascade.”
This cascade, Dr. Nangia said, spreads through the body and can inflame various organs—contributing to asthma, heart disease, high blood pressure, and even conditions like rheumatoid arthritis.
Reading Delhi's AQI
As per the aqi.in there are six categories under which air pollution levels are measured, which are as followed:
- Good 0 to 50
- Moderate 50 to 100
- Poor 100 to 150
- Unhealthy 150 to 200
- Severe 200 to 300
- Hazardous 301+
Fact: AQI in Delhi is 1.9 times above than in India
Public Health Emergency
There are many short-term and long-term impact on public health from the constant exposure of air pollution. As per IQAir, in the short-term, people experience irritation in eyes, throat, and nose, along with irregular heartbeats, asthma attacks, coughing, chest tightness, and difficulty breathing.
Prolonged exposure also intensifies these risks and leads to long-term effects such as chronic respiratory illnesses like bronchitis, asthma, and emphysema. Pollutants can also damage lung tissue, increasing the likelihood of lung cancer. Air pollution also leads to an increased risk of heart attacks and strokes and could also be linked to premature death.
David Cameron, Former UK Prime Minister, Has Prostate Cancer
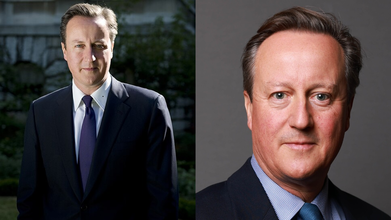
Credits: Wikimedia Commons
Former UK Prime Minister David Cameron revealed his prostate cancer diagnosis and has called for a targeted screening. In an interview with Times, he said, "You always hope for the best. You have a high PSA score - that is probably nothing. You have an MRI scan with a few black marks on it. You think, ‘Ah, that’s probably OK.’ But when the biopsy comes back, and it says you have got prostate cancer. You always dread hearing those words. And then literally as they’re coming out of the doctor’s mouth you’re thinking, ‘Oh, no, he’s going to say it. He’s going to say it. Oh God, he said it.’"
The former PM, 59, said that he had a prostate-specific antigen (PSA) test for the screening that looks for proteins associated with the form of the disease. His result was high, and a biopsy after that revealed his cancer.
It was his wife, Samantha, who urged him to get tested, after the couple heard the founder of Soho House, Nick Jones, talking about his diagnosis on radio. Cameron had received focal therapy for treatment, where electrical pulses target and destroy the cancer cells.
Cameron Calls for National Prostate Cancer Screening
He has urged the government to introduce a national screening programme to detect prostate cancer earlier, when treatment is far more effective.
Cameron said, “I want to, as it were, come out. I want to add my name to the long list of people calling for a targeted screening programme.
“I don’t particularly like discussing my personal intimate health issues, but I feel I ought to. Let’s be honest. Men are not very good at talking about their health. We tend to put things off.”
Prostate Cancer: The UK’s Most Common Male Cancer
Prostate cancer remains the most common cancer among men in the UK, with around 55,000 cases diagnosed every year. Despite this, there is currently no national screening programme because of concerns over the accuracy of PSA tests.
In October 2024, six-time Olympic gold medallist Chris Hoy revealed he had been diagnosed with terminal stage 4 cancer. His prostate cancer had spread to his shoulder, pelvis, hips, ribs and spine.
Read: Olympic Cyclist Sir Chris Hoy Shares His Diagnosis Of Prostate Cancer From A Common Shoulder Pain
Cameron, who stepped down as prime minister and MP in 2016, returned to government as foreign secretary under Rishi Sunak in 2023 and was appointed a life peer in the House of Lords.
New Screening Trial Begins Across the UK
Cameron’s announcement comes just days after eligible men began receiving invitations to join a major trial testing the most promising prostate cancer screening technologies.
The Transform project will evaluate new screening methods against current NHS diagnostic pathways, which typically include blood tests and biopsies. The trial is being run in partnership with the NHS through the National Institute for Health and Care Research, which has committed £16 million, with additional funding from Prostate Cancer UK.
Its launch coincides with the UK National Screening Committee’s upcoming decision on whether current evidence supports introducing national screening.
‘Men’s Lives Should Not Be Left to Chance’
Chiara De Biase, director of health services, equity and improvement at Prostate Cancer UK, welcomed Cameron’s openness about his diagnosis.
Also Read: Joe Biden Is Diagnosed With Aggressive Prostate Cancer: All That You Need To Know
“We’re glad to hear that David Cameron found his prostate cancer at an early stage and had successful treatment,” she said. “We thank him for sharing his story and raising vital awareness of this disease, which is completely curable if found early. But men’s lives should not be left to chance.
“We lose 12,000 dads, brothers, sons and friends every year. We’ve reached a tipping point in the UK, with too many men dying from a curable disease and worse outcomes for higher-risk groups like black men and men from working-class communities.
“Prostate cancer is the last major cancer without a screening programme, and we need change now.”
What Happens In Prostate Cancer?
As per Urology Care Foundation, prostate cancer develops when abnormal cells form and grow in the prostate gland. Not all abnormal growths, also called tumors, are cancerous. Some are benign growth and are not life threatening. They also do not spread to nearby tissue or other parts of the body.
Whereas cancerous growths can spread to nearby organs and tissues, as in the case of Biden.
Donald Glover Opens Up About A Stroke He Had On Childish Gambino’s 2024 Tour
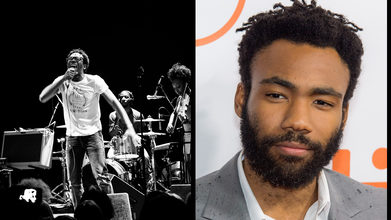
Credits: Wikimedia Commons
Donald Glover, who formerly performed under the stage name of Childish Gambino revealed that he had a stroke last year due to which he had to cancel his world tour date. Now, 42, he said he is dealing with an "ailment", after the New Orleans performance. He revealed that after that performance, he had gone to hospital in Houston, where he discovered that his condition required surgery.
As a result, he postponed his tour, which eventually was cancelled. This tour was remainder of his US tour and his UK, European, and Australian tour dates. He wrote: "Unfortunately, my path to recovery is taking longer than expected."
While performing at Tyler, the Creator’s Camp Flog Gnaw festival in Los Angeles on Saturday, Glover shared the real reason behind his sudden tour halt.
“I was doing this world tour … really loving seeing you guys,” he said, as reported in Guardian. “I had a really bad pain in my head in Louisiana and did the show anyway. I couldn’t really see well, so when we went to Houston, I went to the hospital and the doctor was like, ‘You had a stroke.’”
He joked that his first thought was, “Here I am still copying Jamie Foxx,” referencing Foxx’s 2023 stroke, before admitting his immediate fear was that he was letting fans down—though he knows that isn’t true.
Glover added that doctors also found he had a broken foot and a hole in his heart, which required two surgeries.
“They say everybody has two lives, and the second starts when you realize you only have one,” he told the crowd. “You’ve got one life, guys, and the life I’ve lived with you has been such a blessing.”
Glover, a five-time Grammy winner, has since retired the Childish Gambino moniker after releasing his final album, Bando Stone & the New World. The cancelled tour had been planned as his farewell to the stage name.
What Happens In A Stroke?
When you have a stroke, the blood supply to part of your brain is interrupted. This cause brain cells to die from a lack of oxygen and nutrients. This could also lead to lasting brain damage, long-term disability, or even death.
What Does It Mean To Have A Hole In Heart?
As per Cleveland Clinic, hole in heart means to have an atrial septal defect or ASD, which is an opening in the wall that separates the heart's chambers. While some small holes may close on their own and have no symptoms, larger holes can cause blood to mix between oxygenated and deoxygenated sides, forcing the heart to work harder and potentially leading to health issues like shortness of breath. Treatment options range from monitoring to surgery or minimally invasive procedures, depending on the size and severity of the defect.
Types of holes in the heart
- Atrial Septal Defect (ASD): A hole in the wall (septum) between the two upper chambers (atria) of the heart.
- Ventricular Septal Defect (VSD): A hole in the wall between the two lower chambers (ventricles).
- Patent Foramen Ovale (PFO): A common type of ASD, where the opening between the atria doesn't close after birth.
What Happens When Someone Has A Hole In Their Heart?
- Normally, the left side of the heart pumps oxygen-rich blood to the body, and the right side pumps oxygen-poor blood to the lungs.
- A hole in the heart allows oxygen-rich and oxygen-poor blood to mix.
- This can cause oxygen-rich blood to recirculate to the lungs instead of the body, or cause the heart to pump extra blood to the lungs.
© 2024 Bennett, Coleman & Company Limited

