- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Locked-in syndrome: Neurologist Reveals Scariest Condition Suffered By Many

Neurologist (Credit: Canva)
There are a lot of things that can go wrong in your brain and can lead to conditions as serious as schizophrenia. A mere breakage in the neural connection in your brain is enough to devastate your entire life. Now, a video has gone viral on social media that shows a neurologist revealing "the most terrifying neurological condition" he has ever seen.
“Imagine being fully aware, able to feel everything, hear everything and see everything, and able to think clearly — but completely unable to move or speak, and only able to blink and move your eyes up and down,” he said in the clip.
This condition is called locked-in syndrome. Also known as pseudocoma, it is a rare and severe neurological disorder. Unlike coma, individuals with this condition are completely conscious but have almost total body paralysis. They retain only limited control over eye movements and blinking, making these the only means of communication for most patients. While their minds remain alert, their bodies are unresponsive to voluntary commands.
The damage in locked-in syndrome typically affects the pons, a critical part of the brainstem responsible for transmitting signals between the brain and the rest of the body. Injuries to this area can result from strokes, traumatic brain injuries, infections, or diseases like multiple sclerosis that degrade the protective myelin sheath around nerve fibers. It is an extreme form of paralysis and can leave individuals unable to speak, move, or even react to painful stimuli. As a result, diagnosing locked-in syndrome is often challenging. Many patients have been mistakenly declared brain dead, as their lack of physical response can be easily misinterpreted.
Locked-in syndrome also profoundly impacts basic bodily functions. Patients often require a tracheotomy to aid breathing, as their respiratory muscles may no longer function effectively. Similarly, a gastrostomy tube (G-tube) is frequently necessary to ensure they receive adequate nutrition and hydration. Without these medical interventions, their survival would be severely compromised.
One of the most heartbreaking aspects of locked-in syndrome is the inability to communicate effectively. The condition robs individuals of their voice, leaving them reliant on eye movements to express themselves. Even this form of communication can be painstakingly slow and requires immense patience from both the patient and their caregivers.
Diagnosis
Diagnosing locked-in syndrome requires advanced medical imaging and tests to assess brain and nerve function. Magnetic resonance imaging (MRI) can help identify the location and extent of brainstem damage, while an electroencephalogram (EEG) measures electrical activity in the brain to confirm consciousness.
Treatment
There is no cure or specific treatments for locked-in syndrome other than treating the cause and preventing further complications, if possible.
Bird Flu Detected in Dutch Cow, Marking Europe’s First Case

Credit: Canva
Avian or bird flu (H5N1) is a viral infection that spreads in birds, cows and other animals and can cause severe illness and at times, be fatal to humans in rare cases. Until now, the flu primarily affected wild aquatic birds including ducks, geese, gulls and poultry such as chickens as well as turkeys.
However earlier this month, a dairy cow in the Netherlands appears to have been contracted bird flu, making this the first time cattle outside of the United States has suffered the infection.
Previously, transmission of avian flu from cattle to humans has only been reported in the US among farm workers exposed to infected cattle or contaminated environments, and such cases remain sporadic and all developed only mild symptoms.
How Was The Cow Infected?
According to a detailed letter from the Dutch agriculture minister, a cat on a dairy farm in the province of Friesland died from H5N1 last month, which prompted officials to sample blood and milk from cattle at the farm.
Out of the 20 tested, one cow had antibodies to the virus in its milk but did not test positive for the virus itself. “There are also no signs of avian influenza spreading to other dairy farms,” the minister wrote.
The cow had mastitis and respiratory problems last month and its milk was not processed, the letter stated. Also, milk from the farm had been pasteurized, which inactivates the virus and prevents it being transmitted to humans.
“This means that there is very little chance that virus from the infected cow has ended up in the milk for human consumption,” the minister assured. It remains unclear how the virus arrived at the farm or how the cat and cow became infected.
Since October 2025, more than three dozen farms in the Netherlands have had outbreaks and over 1.5 million chickens, turkeys and ducks have been killed to stop the virus’ spread.
Is Bird Flu Dangerous For Humans?
Even though birds are the primary hosts for avian influenza viruses, certain strains can cross species barriers and infect humans and other animals, sometimes causing severe illness.The H5N1 strain drew worldwide concern in the early 2000s because of its high fatality rate in infected people. Although sustained human-to-human transmission is uncommon, infection can occur through close contact with sick or dead birds, their droppings, or contaminated environments.
Bird flu has posed major challenges for both the poultry industry and public health systems, with outbreaks often resulting in large-scale culling to limit the spread.
India has experienced recurring avian influenza outbreaks, particularly in regions with dense poultry farming. Even with strict control measures in birds, the risk of human infection persists, making awareness, hygiene practices, and preventive steps essential for protecting public health.
The common ways humans can contract the virus include:
- Direct contact with infected birds: Handling sick or dead birds, cleaning poultry farms, or working in live bird markets increases the risk
- Exposure to contaminated surfaces: The virus can survive on surfaces such as bird cages, equipment, and clothing. Touching these and then touching the eyes, nose, or mouth can lead to infection
- Consumption of undercooked poultry or eggs: While properly cooked poultry is safe, raw or undercooked meat and eggs from infected birds may pose a risk
- Airborne transmission in poultry farms: In rare cases, workers in enclosed spaces with infected birds may inhale tiny virus-laden particles
Spanish Scientists Find Breakthrough Cure For Pancreatic Cancer
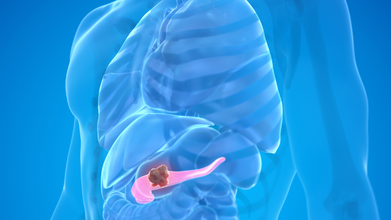
Credit: Canva
In a breakthrough study, a group of Spanish researchers have created a drug-based cure that can kill pancreatic cancer tumors in the body and eliminate the disease completely.
A study from the Spanish National Cancer Research Centre (CNIO) found that a combination of three drugs, known as CNIO therapy, can shut down multiple tumor survival mechanisms at the same time, preventing the cells from the rewiring themselves and defeating the treatment
Led by renowned cancer biologist Dr Mariano Barbacid, the authors wrote of the results: 'These studies open a way to design new combination therapies that can improve the survival of patients with pancreatic ductal adenocarcinoma. These results set the direction for the development of new clinical trials."
How Does The Drug Work?
To overcome cancer's ability to block the effects of singular therapy drugs, Dr Barbacid’s team attempted attacking the cancerous tumors from three directions together.
The first drug, daraxonrasib, blocked the main KRAS signal that drives tumor growth while the second drug, afatinib, shut down EGFR and HER2, both pathways that cancer cells often use to escape KRAS-targeted treatment.
The third drug, SD36, stopped the functioning of bSTAT3, a backup system that helps cancer cells survive stress and resist therapy.
In the mice study, when scientists combined and used all three drugs together in the rodents, they saw the pancreatic tumours shrank completely and did not return, even more than 200 days after treatment stopped.
The same effect was seen in genetically engineered mouse models and in tumors taken from human patients that were grown in a laboratory. The animals who underwent CNIO therapy did not show serious side effects, suggesting the combination could be safe enough to test in humans.
Despite promising results, the authors advised caution and noted: ""We are not yet in a position to carry out clinical trials with triple therapy. The authors themselves warn that optimising this combination for patients will be a complex process, although they are confident that the finding will set the course for future trials."
Pancreatic Cancer: All You Need To Know
Pancreatic cancer typically begins in the ducts of the organ and can rapidly spread from there to the rest of the organ. Early-stage pancreatic tumors do not show up on imaging tests, making this version of the disease difficult to diagnose until it infects other organs.While there are no clear signs of early pancreatic cancer, symptoms begin to show once the disease reaches the digestive system. Some of these include:
- Jaundice (yellowing of your skin).
- Dark urine
- Light-colored stool
- Upper abdominal pain
- Middle back pain
- Fatigue
- Itchy skin
- Nausea and vomiting
- Gas or bloating
- Lack of appetite
- Blood clots
- Weight loss
- New-onset diabetes
Certain prominent risk factors include smoking cigarettes, cigars and using other forms of tobacco; obesity; Type 2 diabetes and genetic factors.
Pancreatic cancer is also resistant to many common cancer drugs and it notoriously difficult to treat, making this discovery exceptionally important in the search for a permanent cure.
About 22,000 new cases of pancreatic cancer are estimated to occur annually in India out of which nearly 13,000 die from the cause, making it the 24th most common cancer in India.
Brain-Eating Amoeba That Thrives In High Heat Is Spreading Fast: What You Need To Know
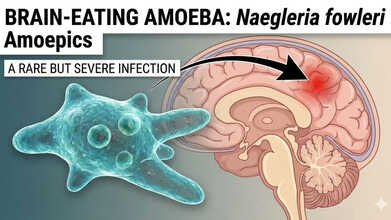
Credits: AI Generated
A collective of environmental and public health researchers has raised serious concerns over free-living amoebas, warning that these organisms could become an increasing global health risk. Their concern stems from the amoebas’ ability to survive in harsh conditions and bypass routine water treatment processes.
These tiny protozoa occur naturally in soil and freshwater and are usually harmless. However, certain species, particularly Naegleria fowleri, widely referred to as the “brain-eating amoeba,” can trigger rare but deadly infections when contaminated water enters the nose during activities such as swimming or diving.
This issue is especially significant for India, as Naegleria fowleri causes primary amoebic meningoencephalitis (PAM), a fatal condition that has seen repeated outbreaks in states such as Kerala.
What Is Naegleria Fowleri?
Naegleria fowleri is a free-living ameba, meaning it is a single-celled organism that survives independently in the environment. It flourishes in warm freshwater sources such as lakes, rivers, ponds, and hot springs. Commonly labelled the “brain-eating ameba,” it earns this name because of its ability to infect the brain and damage brain tissue. The organism is found worldwide in soil and warm freshwater bodies.
On rare occasions, it has also been detected in inadequately maintained swimming pools, splash pads, and other recreational water facilities. In some instances, the ameba has even been identified in tap water.
According to the US Centers for Disease Control and Prevention (CDC), when water containing the ameba enters the nose and reaches the brain, it can lead to an infection known as primary amebic meningoencephalitis (PAM). In the United States, PAM affects fewer than 10 people each year. Almost everyone diagnosed with PAM does not survive. From 1962 to 2024, 167 cases were reported in the US, with only four known survivors.
What Is Primary Amebic Meningoencephalitis?
Primary Amebic Meningoencephalitis (PAM) is a rare but almost always fatal brain infection caused by the Naegleria fowleri amoeba, often called the “brain-eating amoeba.” The organism enters the body through the nose from warm freshwater or soil, travels to the brain, and destroys brain tissue. This leads to intense inflammation, confusion, seizures, and, in most cases, death within days of the onset of severe symptoms.
Primary Amebic Meningoencephalitis Signs And Symptoms
Early signs of PAM may include headache, fever, nausea, and vomiting. The disease progresses very quickly. Most patients die within one to 18 days after symptoms appear, with coma and death often occurring within five days. As the infection advances, symptoms can worsen to include a stiff neck, confusion, reduced awareness of people and surroundings, loss of balance, and hallucinations.
Brain Eating Amoeba Can Thrive In Heat
In a recent perspective published in the journal Biocontaminant, scientists led by Longfei Shu from Sun Yat-sen University explain how climate change, ageing infrastructure, and poor monitoring systems are creating conditions that allow these microbes to spread into areas where they were previously uncommon. Some species are capable of surviving high temperatures and can withstand disinfectants such as chlorine, making them particularly difficult to remove from drinking water supplies and distribution systems.
Adding to the concern, free-living amoebas can serve as protective carriers for harmful bacteria and viruses, housing them inside their cells and helping them spread. This so-called “Trojan horse” effect has raised fresh questions about water safety and how pathogens move through the environment, highlighting the need for coordinated, One Health-based approaches.
Experts warn that without strong intervention and improved water management policies, free-living amoebas could emerge as a major and largely overlooked threat to global public health in the coming years.
© 2024 Bennett, Coleman & Company Limited

