- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Source: Northwell Health/Cohen Medical Center and Canva
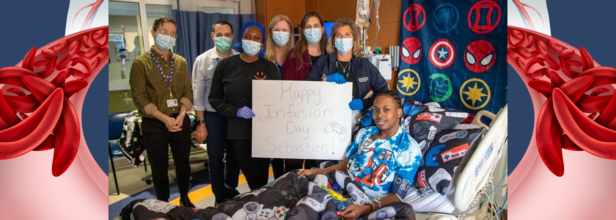
Meet The First Man In New York's History To Be Cured Of Sickle Cell Disease
A long Island man became the first in New York history to be cured of sickle cell anemia. This man is Sebastien Beauzile, who, for the last 21 years of his life lived with the chronic pain of sickle cell anemia. However, he owes it to the groundbreaking genetic treatment for curing his condition.
The hospital where he was getting his treatment used an advanced therapy called Lyfgenia.
What Is Lyfgenia?
It is an FDA approved genetic therapy that treats sickle cell disease in patients 12 years of age or older and a history of vaso-occlusive events. It is made specifically for each patient, using the patient's own blood stem cells, from which the red blood cells are produced. It adds functional copies of the beta-globin gene to your cells leading to production of anti-sickling hemoglobin that may decrease or stop vaso-oclusive events.
The process of preparing it from your own blood stem cells takes about a week and it may be needed to repeat to obtain sufficient number of cells.
For this process, even "back up" stem cells or "rescue cells" are also collected and stored at the treatment center as a precaution in case there is a problem in the treatment process. If any issue occurs, your back up stem cells will be given back to you. In case you receive the back up stem cells, you will have no benefit from Lyfgenia.
Before you receive Lyfgenia, your healthcare provider will give you chemotherapy for a few days to make room in the bone marrow. You will be admitted to the treatment center for this step and remain there until after Lyfgenia infusion. It is given by an intravenous infusion and you may need more than one bag of it.
What Is Sickle Cell Disease?
As per the National Heart, Lung, and Blood Institute, sickle cell disease or sickle cell anemia is a group of inherited disorder that affect hemoglobin, the major protein that carriers oxygen to red blood cells. In this disease, the red blood cells are misshaped, in the shape of 'sickle' and they do not move or bend easily and can in fact it can block the blood flow to the rest of the body.
Sickle cell disease was first described in 1910 that affected people for African, Mediterranean and Middle Eastern descent.
It can lead to serious problems like onset of strong episodes of pain, also called pain crises that occur due to blocked blood flow and may require medical attention. People with sickle cell disease could also experience chronic pain, stroke, lung problems, eye problems, infections, and kidney diseases.
Back On The Case
Beauzile is now cured and he told the CBS News, "Sickle cell was like a blockade for me, but now it is just like a wall that I just jumped over."
His mother informed that he had been coming to the hospital since he had been 2 months old. Seeing things get better and him recover has been a dream come true and "there is not enough words" for her to show how grateful she is, she said.
Being free from the disease, Beauzile now looks forward to travelling, exercising, and pursuing his education. Being inspired by the doctors who cured him, he too wants to work in the medical field. "I cannot wait to get back to my day-to-day life because now I feel unstoppable," he said.
New RNA-Based TB Detection Could Soon Take Minutes, Not Months
Tuberculosis (TB) is a deadly global health crisis despite being a curable disease. In 2023 alone, TB killed about 1.25 million people globally — more than any other infectious pathogen. While the ability of months- or years-long courses of antibiotics to kill Mycobacterium tuberculosis, the bacteria that cause the disease, treatment success is not certain for all. In fact, in approximately 12% of patients, TB recurs even after treatment.
The major roadblock is that clinicians today lack a specific test to see if TB bacteria were completely removed from the body by treatment. Failing to have accurate monitoring mechanisms, doctors have to implement the same six-month treatment regimen in all patients and accept that some will be over-treated and some will be failures. However, all that may soon change, thanks of a breakthrough RNA-based TB detection test that Dr. Kayvan Zainabadi, assistant professor of molecular microbiology at Weill Cornell Medicine, and his India-based team are developing.
Modern TB treatment protocols are dependent on clinical experience and sputum-based diagnostic procedures that identify bacterial DNA. However, these procedures are fraught with limitations. Despite the successful treatment, residual bacterial DNA can continue to be present in the patient's system, resulting in false positives and making it difficult to clearly perceive the status of the disease.
This diagnostic imprecision compels physicians to remain with a "one-size-fits-all" six-month treatment regimen, even when evidence indicates that most patients might be cured earlier. Long-term exposure to highly effective antibiotics not only risks patients developing side effects but also places a heavy burden on healthcare systems, particularly in low-resource settings where TB is most prevalent.
Dr. Zainabadi’s research introduces a groundbreaking concept: using ribosomal RNA (rRNA) as a rapid, sensitive, and accurate marker of TB infection. Unlike DNA, RNA is inherently less stable and degrades quickly after bacterial death, minimizing the risk of false positives.
The innovation is aimed at the detection of the 16S rRNA of Mycobacterium tuberculosis, which is a part essential to bacterial protein synthesis. Its prevalence in the cell makes it a prime target for detection even in small or difficult-to-access samples.
Significantly, this RNA-based method might overcome the sputum reliance that is sometimes tricky to obtain from high-risk populations such as children or HIV-infected individuals. Rather, less intrusive sample forms might be utilized, providing a more patient-centered, convenient, and scalable platform.
How Does It Work?
The RNA test operates by extracting 16S rRNA from patient samples and amplifying it using highly sensitive molecular methods. Since rRNA degrades quickly after bacterial cells die, detecting it gives real-time feedback regarding the presence of active TB infection — something DNA-based tests cannot consistently provide.
In practice, a sample would be taken from the patient (possibly from gastric fluid, blood, or other more readily accessible fluids) and run through the RNA detection system. If live bacteria are present, the 16S rRNA signature would show up in the test results, providing clinicians with an instant readout of disease activity.
The rapidity and precision of this methodology may significantly reduce diagnostic turnaround times from weeks or months to mere minutes or hours. This results in quicker clinical decisions, more targeted interventions, and substantial reductions in patient anxiety and healthcare expenditures.
Is It More Helpful Than Other Diagnostic Tests?
In comparison to conventional sputum microscopy and DNA-based molecular diagnostics, the RNA-based test has a number of revolutionary benefits.
First, its ability to target active infection — not just bacterial residue — prevents patients from being subjected to unnecessary or excessive treatment. This specificity is especially important in combating multidrug-resistant TB, where inappropriately using antibiotics exacerbates resistance problems.
Secondly, the fact that it can accept non-sputum samples makes it much more convenient. It is not possible for several children and immunocompromised individuals to produce sufficient sputum, and clinicians are left with the option of using invasive and less effective gastric lavage methods. An RNA-based test would equalize access to proper TB diagnosis among these high-risk populations.
Third, in the field of TB drug discovery, this test might be a game-changer. Rather than waiting two years to determine if a drug is effective, researchers would be able to monitor bacterial clearance in real-time, moving clinical trials forward more quickly and lowering costs.
Lastly, at a macro health systems level, a quick, precise, and less intrusive diagnostic device would be a game-changer for TB-endemic countries where resources are tightly constrained and the disease burden is highest.
The stakes are as high as they could possibly be. TB has continued to be a recalcitrant worldwide killer, too often fueled by diagnostic ambiguity and treatment inefficacy. An RNA-based diagnostic test such as the one Dr. Zainabadi and his colleagues are creating is not only an incremental step but a potential paradigm shift in how we combat the disease.
As the study continues, the expectation is that this new technology will not only revolutionize individual patient treatment but also redefine the public health sector in the global fight against tuberculosis.

Measles Cases In US Hit 900 Mark, 10 States Reporting Active Outbreak; Is Prevention The Only Cure?
With measles cases soaring to nearly 900 across the United States, public health officials are raising the alarm over what is rapidly becoming an escalating crisis. The U.S. Centers for Disease Control and Prevention (CDC) has reported 884 cases in 29 states, a whopping threefold increase over all of 2024. With ten states now reporting active outbreaks, the urgent question remains- is prevention really the only cure?
The United States, in 2000 having declared measles eliminated, now confronts a sobering resurgence. Most of the cases currently, 646, are from Texas, where an outbreak based in West Texas continues to expand after almost three months. Some of the states that are struggling with ongoing outbreaks are Indiana, Kansas, Michigan, Montana, New Mexico, Oklahoma, Ohio, Pennsylvania, and Tennessee.
Unfortunately, two West Texas unvaccinated children and a New Mexico adult have died from measles complications. These deaths reinforce the outbreak's severity and the vulnerability of unvaccinated groups.
Adding to the worry, North America is not alone in this battle. Nearby nations report similar crises — Ontario, Canada, has recorded more than 1,020 cases, and Mexico's Chihuahua state has recorded 605 cases attributed to the Texas outbreak, reports the World Health Organization (WHO).
Why Is Measles Making a Comeback?
Measles is among the most infectious viruses, able to stay in the air and on surfaces for hours after a person infected with it coughs, sneezes, or even breathes. In an extremely immunized population, the disease cannot spread — an effect called "herd immunity." But when vaccination rates are low, vulnerability pockets form.
A number of factors are to blame for the outbreak:
Waning Vaccination Coverage: CDC reports a troubling trend. For the 2023–24 school year, vaccination coverage of kindergartners in the United States declined to 92.7% for the MMR vaccine from 93% in the last school year. Worryingly, vaccine exemptions reached 3.3%, a record high.
Regional Vulnerabilities: In the epicenter of the outbreak, Gaines County, Texas, MMR vaccination coverage has fallen to a mere 82%, well short of the 95% required to ensure herd immunity. Not surprisingly, children have borne the brunt: of 198 cases in the region, 153 were in people under the age of 18, the majority of whom were unvaccinated or whose vaccination status was unknown.
Global Trends and Misinformation: Globally, vaccine hesitancy, driven by misinformation, concern over side effects, and public health messaging distrust, is weakening immunization efforts. Discredited theory linking MMR vaccines to autism, though disproven, remains active, with special presence on social media outlets.
Though frequently confused as a harmless illness of childhood, measles can be fatal. Measles attacks the respiratory tract first and then the rest of the body, producing high fever, cough, nasal discharge, red, watery eyes, and a characteristic rash that initially appears on the face and travels downward.
Measles can have serious complications, including:
- Pneumonia: One of the main causes of death in measles.
- Blindness: Due to scarring of the cornea.
- Encephalitis: Fatal brain swelling that may result in permanent brain damage or death.
The CDC says the rash accompanied by fever may rise to more than 104 degrees Fahrenheit. Most healthy children will bounce back, but for at-risk groups — especially the unvaccinated — the virus can rapidly become deadly.
Why MMR Vaccine is The First Line of Defense?
CDC and WHO are in agreement: vaccination is still the best way to prevent measles. The measles, mumps, and rubella (MMR) vaccine is most often given in two doses — the first dose between 12 and 15 months, and the second dose between 4 and 6 years. The vaccine is safe, works, and has decades of proven success.
For those worried about declining immunity, taking an extra dose is harmless. Those vaccinated prior to 1968 with an ineffective "killed" virus vaccine should have at least one additional dose.
Where vaccination coverage is over 95%, outbreaks are uncommon because the virus has few susceptible hosts. Widespread exemptions and misinformation have, however, resulted in severe immunity gaps, enabling measles to gain a foothold once again.
The increase in cases is not so much a matter of gaps in healthcare logistics. It is symptomatic of deeper loss of faith in science and public health organizations.
Experts refer to a range of factors promoting vaccine hesitancy:
Misinformation: Rumors about the side effects of vaccines, with a focus on unfounded speculations about an MMR-a Autism link.
Skepticism following COVID-19: Distrust generated by the pandemic has seeped over into routine vaccination.
Needle Phobia or Side Effects: Fear and misconceptions regarding ingredients or eventual outcomes of vaccines remain a concern among parents.
Similar trends globally are reflected in concerns. In the United Kingdom, for example, MMR vaccination coverage at age 5 decreased to their lowest levels since the 2010–11 periods, contributing to more than 2,900 cases of measles to date this year.
Is Prevention the Only Cure?
Plain and simple, yes. There is no antiviral therapy for measles. Supportive care — treating fever, maintaining hydration, and managing secondary infections — is all that can be provided once infection has been established.
In the absence of curative treatments, vaccination is not only the best weapon against measles — it is the sole weapon.
Public health experts stress that immediate action is imperative. Targeted public awareness campaigns, coordination with global agencies such as WHO and UNICEF, and combating vaccine misinformation directly are key strategies. Re-establishing trust and guaranteeing mass vaccination is the only long-term solution to forestalling future outbreaks.
The current upsurge in cases of measles all over the U.S. and globally is a chilling reminder: complacency can reverse decades of public health advances.
In a time of unparalleled access to medical information and resources, no child should ever die from a preventable illness like measles. The way forward is simple — revitalize immunization programs, fight misinformation, and advance community health through fact-based, science-driven advocacy.
Preventing measles isn't merely about saving individual lives — it is about protecting future generations.
Credits: Canva
World Immunization Week: India Pushes To Eliminate Measles And Rubella By 2026
As a part of World Immunization Week, which is observed from April 24 to 30, to promote the life-saving power of immunization, notes the World Health Organization (WHO), India has launched a week-long campaign to vaccinate 100% of children against measles and rubella. This is a move described as crucial to country's goal of eliminating the two viral diseases by 2026, noted Union Health Minister JP Nadda.
As per WHO, this week aims to promote the power of immunization to protect people of all ages against vaccine-preventable diseases. Vaccines are one of humanity's greatest achievements, notes WHO. Since 1974, they have saved 150 million lives.
As per India's aim, Nadda suggests that health workers must not only ensure complete vaccination overage, but also remain vigilant through robust disease surveillance. “Measles is very contagious. Even a single case must be treated as a warning signal. We have to cover immunity gaps and ensure no child is left behind,” he said.
As per WHO, India has reported 4,388 cases of measles and 527 cases of rubella so fat this year.
What Are Measles And Rubella?
Measles is a highly contagious viral infection marked by symptoms such as high fever, rash, cough, red eyes, muscle pain, and headache. Though often seen as a childhood illness, measles can lead to severe complications, including pneumonia, brain swelling (encephalitis), and even death, particularly in malnourished children and those with weakened immune systems.
Rubella, caused by a different virus, typically results in milder symptoms in children and adults. However, it poses a grave risk to pregnant women. Infection during pregnancy, particularly in the first trimester, can cause miscarriage, stillbirth, or congenital rubella syndrome (CRS) — a condition leading to serious birth defects like heart problems, deafness, and developmental delays. According to WHO, rubella control is essential for reducing infant mortality and morbidity.
History of Measles and Rubella Vaccination In India
India has a long battle with measles, which had accounted for a significant portion of global measle deaths. In order to tackle this, the country introduced measles vaccination in 1985, under the Universal Immunisation Programme. However, rubella vaccination lagged behind until the Measles-Rubella (MR) vaccination campaign was launched in 2017.
This massive drive aimed to immunize 410 million children between 9 months and 15 years of age, marking one of the largest vaccination campaigns in the world, according to the Ministry of Health and Family Welfare. Post-campaign, the MR vaccine was incorporated into India’s routine immunization schedule, with two doses given between 9–12 months and 16–24 months of age.
Since measles and rubella are both highly contagious, health authorities say that achieving very high vaccination coverage — over 95% — is critical for creating herd immunity and stopping outbreaks.
Is India Close To Its Goal?
Health Ministry data shows promising progress: in 2024–25, 93.7% of children received the first MR vaccine dose, while 92.2% received the second. However, to achieve disease elimination, India needs to push these numbers above 95% consistently across all regions.
Highlighting the importance of full coverage, Nadda called upon public representatives to actively support the campaign and spread awareness, particularly in hard-to-reach areas.
Despite progress, India faced a significant measles outbreak in 2023. The country was among 57 globally that saw major outbreaks after routine immunization services were disrupted during the Covid-19 pandemic. In 2023 alone, India reported 68,794 cases of measles and 2,930 cases of rubella.
Responding to the surge, the government intensified supplementary immunization activities, targeting areas where outbreaks occurred. The impact is visible: measles cases dropped by 73% and rubella by 17% in 2024 compared to the previous year.
With sustained efforts, India is now on a strong path towards achieving measles and rubella elimination by 2026.
Note: The data is taken from World Health Organization and Ministry of Health and Family Welfare, Government of India.
© 2024 Bennett, Coleman & Company Limited

