- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Eli Lily's Weight Loss Drug Mounjaro Now Available In India

Credit: Canva
US pharma major Eli Lilly launched the much-awaited diabetes and obesity management drug Mounjaro in India on Thursday at one-fifth of the US price. The company rolled out the drug in a single-dose vial following the marketing authorisation from the Central Drugs Standard Control Organization (CDSCO). It has been priced at Rs 3,500 for a 2.5 mg vial and Rs 4,375 for a 5 mg vial. "It is a first-of-its-kind treatment for obesity, overweight, and type 2 diabetes that activates both GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) hormone receptors," the company said.
What Is Mounjaro And How Is It Different From Ozempic?
Like Ozempic and Wegovy, Mounjaro is also a weight-loss drug. However, like the other two, it is not a semaglutide. It is a Tirzepatide. Another difference is that instead of working as a single receptor agonist, it works on two hormones. Muanjaro activates both GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) hormone receptor agonists, leading to an increase in the production of insulin when needed. It also reduces the amount of glucose, or sugar, produced by the liver, and slows down how quickly food is digested. This all helps to lower blood sugar levels and HbA1c. Notably, the fact that it works on two receptors doubles its efficiency than semaglutide like Ozempic and Wegovy.
How Much Would Mounjaro Cost Per Month?
The drug, usually taken once a week, would cost in the range of Rs 14,000 to Rs 17,500 for a month’s therapy depending on the dosage recommended by the doctor. The average monthly price of Mounjaro in the US is around 1000-1200 dollars a month (or Rs 86000-1 lakh."This India-specific pricing reflects Lilly’s commitment to expanding access to innovative treatments in the country," the company said, adding that it is not yet going ahead with any local collaboration for marketing and distributing the drug. "We are committed to expanding access to innovative treatments in India. At this stage, we do not have any partnership announcements regarding Mounjaro (tirzepatide)," the company said. As of now, adults over the age of 18 years with type 2 diabetes can take Mounjaro. However, since it is now rebranded and launched as an anti-obesity drug then it is not clear who would be able to take it. An official statement on usage is awaited.
How Big Is the Anti-Obesity Market In India?
With obesity rates rising in India, the market for weight loss drugs has grown exponentially in the country. Novo Nordisk's oral semaglutide tablet, Rybelsus, launched in India in January 2022, has already captured nearly 65 per cent of the anti-obesity drugs market, which includes other weight-loss medications such as dulaglutide, orlistat, and liraglutide. Notably, Ozempic the most popular drug in this criteria is not officially launched in the country.
Could This New Alzheimer’s Drug Buy Patients Four More Good Years? Here Is What We Know

Not forever, but what if you could press pause on Alzheimer’s just long enough to enjoy a few more good years? That is the tantalising promise behind a new drug called lecanemab, hailed as a game-changer in the fight against dementia.
The drug has already been licensed for use in the UK after trials showed it could slow the pace of decline in people with early-stage Alzheimer’s. But new long-term findings are turning cautious hope into something stronger: patients who stayed on lecanemab for four years experienced a noticeable delay in the disease's progression. Some even showed no decline at all.
How It Works
Alzheimer’s is known for its slow but relentless grip on memory and cognition, typically marked by the build-up of sticky proteins in the brain. Lecanemab targets tau, a protein that increases as the disease worsens.In the initial 18-month trial, the drug delayed Alzheimer’s progression by just under six months. That might not sound like much, but it’s the long game that matters here. Among 478 patients who remained on the drug for four years, the average delay before their disease advanced to the next stage stretched to almost 11 months.
Even more striking: 69 per cent of those with low levels of tau saw no decline at all over the four years. And over half in that same group actually improved their cognitive scores.
A Slow Slide Instead of a Steep Drop
Typically, people with mild Alzheimer’s see their scores on memory and function tests worsen by one or two points each year. But for those taking lecanemab, the total decline across four years was just 1.75 points. That’s a major shift in the rhythm of the disease, changing it from a downhill tumble to a slow shuffle.
Professor Christopher Van Dyck, who led the study at Yale School of Medicine, puts it simply: “You will get worse over time, but it will take longer to get there.” That extra time could mean more independence, more connection with loved ones, and more living.
Why Early Treatment is Key
The benefits weren’t evenly distributed. Patients who had less evidence of Alzheimer’s pathology, that is, fewer early changes in the brain, showed the most striking outcomes. In other words, the earlier you start treatment, the better your odds of preserving function.This makes a strong case for early diagnosis and intervention, which could shift the way we approach Alzheimer’s care. No longer is it just about managing symptoms; it’s about changing the trajectory of the disease.
Not a Cure, But a Clear Step Forward
Lecanemab isn’t a miracle cure. It doesn’t reverse Alzheimer’s, and it’s not suitable for all patients. But experts say it’s a major milestone. Reportedly, this is the first wave of disease-modifying treatments and there’s still plenty to understand.
Other Contenders in the Ring
Lecanemab isn’t the only drug showing promise. A similar treatment called donanemab was tested over a three-year period, though it was only administered for 18 months. Still, the results were encouraging: patients on the drug gained an extra six to 12 months before their disease progressed.
That might not sound earth-shattering, but in a condition where time is everything, even a few more months of clarity and connection can be priceless.
The research is still evolving, but the signs are encouraging. With continued trials, this could be the start of a new chapter in dementia treatment, one where patients and families have more time to prepare, more time to enjoy life, and more hope than ever before.
Dizzy Spells Misread as Vertigo Led to Brain Tumour Diagnosis for 63-Year-Old
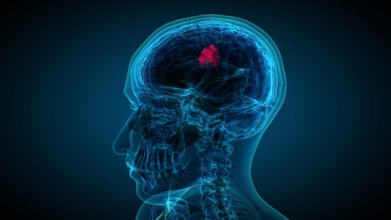
When 63-year-old John Starns slumped on a train station bench in Sevenoaks, drenched in sweat and struggling to stay upright, most passers-by assumed he was drunk. He looked wobbly, pale, and visibly disoriented. But what looked like an awkward case of public intoxication turned out to be something far more sinister: a brain tumour hiding behind symptoms commonly mistaken for vertigo.
From “It’s Just Vertigo” to “You Have a Brain Tumour”
Initially told he had vertigo, John tried to carry on with his life. But as the months passed, his dizziness became more intense and debilitating. At their worst, the episodes forced him to lie down, eyes shut, until the world stopped spinning. Still, no one suspected the real cause.Three months and one MRI scan later, John finally got the truth. He reportedly had a vestibular schwannoma, a rare, benign brain tumour sitting on the nerve that connects the brain to the inner ear. It was affecting his balance, hearing, and overall coordination, symptoms that, in hindsight, were never typical of garden-variety vertigo.
What is Vestibular Schwannoma?
Despite the intimidating name, a vestibular schwannoma is not cancerous. It develops slowly over time from Schwann cells, the fatty insulation on your nerves. In this case, the tumour formed on the vestibulocochlear nerve, which governs both hearing and balance.That is why the symptoms can masquerade as something much less serious.
- Dizziness or vertigo
- Hearing loss in one ear
- Ringing or buzzing sounds (tinnitus)
- Poor sound localisation
- In more advanced cases, numbness on one side of the face
Because these tumours grow at a glacial pace, symptoms tend to hide for months or even years. According to Cancer Research UK, they account for around 8 per cent of all brain tumours, with risk increasing significantly after the age of 65. In rare cases, they are linked to a genetic condition called neurofibromatosis, which often causes tumours on both sides of the brain.
Why Dizziness Deserves a Second Look
Most of us treat dizziness like a mild inconvenience. You get up too fast, feel woozy for a second, then go about your day. Maybe you chalk it up to dehydration, skipping breakfast, or scrolling on your phone in bed for too long. But dizziness could be a sign of something more serious.For John, it was not just one woozy episode. It was a string of unsettling, spin-the-room moments that left him lying flat on his back, eyes squeezed shut, praying for the world to stop pirouetting. And while vertigo was the first suspect, his brain had other plans, like growing a tumour on his vestibulocochlear nerve.
That is the thing with dizziness: it is vague, common, and often misunderstood. It can signal anything from low blood pressure and ear infections to neurological conditions that need serious medical attention. But because it is so easy to dismiss and hard to describe without wildly gesturing, it often gets brushed under the rug until it insists on being noticed.
If you face dizziness, do not ignore it. Especially if the dizziness is intense, recurrent, or comes with sidekicks like hearing loss, balance issues, or ringing in your ears.
Top U.S. Medical Associations Ousted from CDC Vaccine Workgroups in Sudden Shake-Up

Credits: Canva
In a controversial move that has rattled the U.S. medical community, federal health officials have severed ties with more than half a dozen major medical organizations from participating in government vaccine advisory workgroups.
The decision, communicated via email on Thursday, disinvites top experts from these groups from contributing to the workgroups that support the Advisory Committee on Immunization Practices (ACIP), a key body that guides the nation’s vaccination policies.
Organizations affected include the American Medical Association (AMA), the American Academy of Pediatrics (AAP), the Infectious Diseases Society of America (IDSA), and several others, many of whom have historically played a critical role in shaping vaccine guidelines.
“This is deeply concerning and distressing,” said Dr. William Schaffner, a renowned vaccine expert from Vanderbilt University who has been involved with ACIP workgroups for decades. “Removing these organizations will likely create conflicting messages about vaccine guidance. Patients might hear one thing from the government and another from their personal doctors.”
Longstanding Collaboration Ends Abruptly
For years, the ACIP has relied on a structured system where experts from various medical and scientific fields evaluate vaccine data and help draft recommendations. These recommendations, once approved by the Centers for Disease Control and Prevention (CDC), often inform clinical practice and determine insurance coverage.
But according to an email obtained by Bloomberg and confirmed by federal officials on Friday, the medical organizations are now being sidelined on the grounds that they are “special interest groups” and are assumed to carry a “bias” due to the populations they serve.
Dr. Schaffner defended the former system, highlighting how professional organizations offered practical insights on how recommendations could be realistically implemented in clinical settings. Importantly, all members were subject to conflict-of-interest vetting, ensuring objective guidance, he added.
Health Secretary Kennedy’s Sweeping Changes
This latest shake-up follows an earlier, unprecedented move in June when U.S. Health Secretary Robert F. Kennedy Jr. abruptly dismissed the entire ACIP panel, accusing it of being too closely aligned with vaccine manufacturers. Kennedy, a former leader in the anti-vaccine movement, has since appointed several known vaccine skeptics to the new committee.
Among the organizations removed from the workgroup process are the American Academy of Family Physicians, American College of Physicians, American Geriatrics Society, American Osteopathic Association, National Medical Association, and the National Foundation for Infectious Diseases.
In a joint statement released Friday, the AMA and several of the disinvited organizations denounced the decision, calling it “irresponsible” and “dangerous to our nation’s health.” The statement warned that excluding their medical expertise “will further undermine public and clinician trust in vaccines.”
The groups urged the administration to reverse the decision, emphasizing the importance of transparency and collaboration in public health decision-making.
Lawsuit and Fallout
Several of the ousted organizations had previously criticized Kennedy’s overhaul of the ACIP. Last month, three of them joined a lawsuit challenging the government’s decision to halt COVID-19 vaccine recommendations for most children and pregnant women, a policy shift that has been widely criticized by public health experts.
Meanwhile, newly appointed ACIP member Retsef Levi, a professor of business management with no formal medical background, defended the administration's direction on social media. Levi wrote that future workgroups would “engage experts from an even broader set of disciplines,” and claimed that membership would be based on “merit & expertise, not organizational affiliations with conflicts of interest.”
The Department of Health and Human Services (HHS) has not yet disclosed which experts will replace the disinvited members or when the new workgroups will begin operating.
© 2024 Bennett, Coleman & Company Limited

