- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
New Once-a-Week Pill May Transform Schizophrenia Treatment, Lancet Study Finds
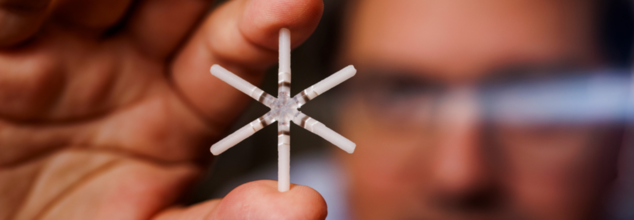
Credits: Melanie Gonick/MIT
A team of researchers from MIT, New York Medical College, and Lyndra Therapeutics have introduced a once-a-week oral pill for schizophrenia. Published in The Lancet Psychiatry, this new treatment model could transform how antipsychotic medications are administered—enhancing patient compliance, improving long-term outcomes, and reducing relapse risk.
One of the most formidable challenges in treating schizophrenia is ensuring patients consistently take their medication. Daily dosing can be a significant hurdle, particularly in psychiatric conditions where cognitive and emotional symptoms hinder memory and motivation.
Enter the newly designed pill: a once-a-week oral capsule featuring a star-shaped drug delivery system that slowly releases risperidone over seven days. The innovation, led by Giovanni Traverso of MIT and Leslie Citrome of New York Medical College, aims to simplify schizophrenia treatment and drastically improve medication adherence.
"We’ve converted something that had to be taken once a day into a weekly oral solution using a novel delayed-release technology," said Traverso, also a gastroenterologist at Brigham and Women’s Hospital. “This innovation can be adapted for a variety of medications."
How Does The Star-Shaped Drug Delivery Device Work?
Roughly the size of a multivitamin, the capsule houses a six-armed, foldable device that expands once it reaches the stomach. This unique shape keeps the device in the stomach for about a week, allowing the steady release of medication.
Over time, each arm breaks off and safely passes through the digestive tract. This ensures the body gradually absorbs the medication while preventing gastrointestinal blockages. “It’s a breakthrough that allows drug delivery in a controlled and sustained manner,” said Dr. Citrome.
Promising Phase III Results
In the Phase III trial, 83 participants with schizophrenia were enrolled across five clinical sites in the US. Of these, 45 patients completed the full five-week regimen, taking one risperidone-loaded capsule per week.
The results were compelling. Drug levels peaked immediately post-dose and tapered slowly over the week. The consistency was superior to daily oral dosing, where patient-administered pills often result in fluctuating drug concentrations.
Symptom control, measured using the Positive and Negative Syndrome Scale (PANSS), remained stable across the board. Patients did not experience the spikes and troughs commonly observed with daily oral intake, a factor often linked to symptom relapses and hospitalizations.
Does This This Offer Minimal Side Effects With Major Potential?
The trial noted only mild side effects such as acid reflux and constipation, which were temporary and manageable. Importantly, the pill demonstrated an impressive safety profile over the trial duration.
“This really validates our hypothesis from over a decade ago—that a once-weekly oral drug delivery capsule could function as a depot system in the gastrointestinal tract,” Traverso remarked.
What are the Other Application?
Beyond schizophrenia, the research team is already eyeing broader applications for this delivery system. Phase I trials are being planned for drugs used in managing conditions like hypertension, asthma, and even for oral contraceptives.
The capsule’s ease of use, combined with its potential to deliver various drugs, makes it an attractive option for chronic conditions where daily adherence is challenging. Patients often prefer oral medications over injections, and this technology could serve as a bridge between convenience and efficacy.
Schizophrenia affects approximately 24 million people worldwide, according to the WHO. Medication adherence remains one of the key challenges in managing the condition. The consequences of missed doses can be severe—leading to relapse, hospitalization, or deterioration in quality of life.
The once-a-week oral capsule has the potential to fill this long-standing gap, offering hope for better disease control and reduced burden on caregivers and healthcare systems.
Dr. Richard Scranton, chief medical officer of Lyndra Therapeutics and senior author of the study, emphasized that the results support moving forward toward FDA approvals. “We’re incredibly optimistic about what this means for the future of psychiatric and chronic disease management.”
Lyndra Therapeutics and MIT are currently preparing for larger Phase III studies to confirm safety and efficacy on a broader scale. If successful, the capsule could be submitted for FDA approval within the next few years.
“This marks a paradigm shift in how we think about oral drug delivery,” added Robert Langer, MIT’s renowned bioengineer and co-founder of Lyndra. “And we’re just getting started.”
World Blood Donor Day 2025: Theme, Significance, And History

Credits: Canva
Every year on June 14, World Blood Donor Day is observed. As per the World Health Organization (WHO), the world celebrates World Blood Donor Day, a global tribute to the millions of voluntary, unpaid blood donors who give others a second chance at life.
Each time you donate blood, you’re giving more than a life-saving gift—you’re enabling critical medical tests that guide treatment and improve care. This World Blood Donor Day, remember: your donation isn’t just for emergencies, it plays a vital role in everyday healthcare too.
History of World Blood Donor Day
The World Blood Donor day dates back to 2004, when it was established by the WHO and is partners. The aim for this was to create a global recognition for he contributions of voluntary donors and to encourage safe blood practices in every country.
Since then, it has become an essential health campaign that brings attention to the need for regular donation. The day also celebrates unsung heroes who, through this simple ac, save lives.
World Blood Donor Day 2025 Theme
This year, as notes WHO, the theme is "Give blood, give hope, together we save lives".
This year’s World Blood Donor Day campaign, with the slogan “Give blood, give hope: together we save lives,” emphasizes the life-changing role blood donors play in saving lives. It underscores the power of community and collective action, showcasing how a simple act of donating blood can create a ripple effect of hope for those in need. Through the sharing of personal stories from both recipients and donors, the campaign aims to inspire more individuals, particularly young adults, to take part in blood donation—whether as first-time donors or as regular contributors.
The campaign will feature, as WHO notes, a variety of activities to celebrate and acknowledge the efforts of blood donors. These could include commemorative events, workshops, social media initiatives, donor appreciation ceremonies, and special broadcasts to honor those who give blood. In addition, musical and artistic performances may be held to express gratitude, while impactful stories will be shared to raise awareness about the importance of blood donation. This year’s objectives are to increase public awareness about the critical need for blood donations, encourage both new and returning donors to donate regularly, and promote solidarity and compassion through these life-saving acts. Furthermore, the campaign seeks to rally support from governments and global partners to ensure sustainable national blood programs, aiming for universal access to safe blood transfusion worldwide.
World Blood Donor Day Significance
This day encourages more and more people to donate blood and save a life. Blood transfusions provide life-saving support, notes WHO. This is especially true for women who experience bleeding related to pregnancy and childbirth, or children who suffer from severe anemia due to malaria or malnutrition.
Other scenarios, notes WHO, where blood transfusion helps include, complex medical procedures, patients with sickle-cell disease, thalassemia, hemophilia, or immune deficiency disorder, or for emergency responses, in cases of natural disasters or armed conflicts.
Social Media Isn’t Just Addictive—It’s Potentially Depressing Your Teen, Study Finds

Credits: Canva
On the surface, social media is just a harmless distractiona virtual playground where teens bond over memes, music, and makeup tips but behind filters and faddish trends, there is a deepening concern for mental health. Emerging evidence indicates that for preteens, scrolling through carefully crafted lives may not only define them it could be quietly undermining their emotional health. A new study now verifies what many mental health professionals and parents have long suspected: social media isn't only addictive—it's potentially driving a more profound wave of depression in today's kids.
Social media is a daily habit for many teenagers and preteens. With TikTok, Instagram, and Snapchat dominating their screen hours, it has become their primary platform for expression, entertainment, and social interaction but beneath the endless scrolling and viral memes is a mounting public health issue: rising data indicates social media use is correlated with rising depression rates among young users. A recent study from UC San Francisco puts this issue into sharper relief, indicating that social media does not just mirror mental illness in children—it could potentially be causing it.
A study led by Dr. Jason Nagata of the Department of Pediatrics at UCSF and published in JAMA Network Open tracked close to 12,000 children ages 9 through 13. By using within-person longitudinal data, researchers could tease out the cause-and-effect link between depression and social media use. What they found was, in a word, sobering: while social media usage went up from seven minutes a day to 73 minutes every three years, symptoms of depression increased by 35%. Most importantly, the study explained that although greater social media usage had resulted in greater depressive symptoms, the opposite was not the case—already-existing depressive symptoms did not cause a rise in screen time.
Hidden Risks Lurking Behind the Screen
Why does social media exert such a strong influence on preteen mental health? While the exact mechanisms remain under investigation, researchers suspect several culprits. One is cyberbullying—a separate study by Nagata and his team, published in The Lancet Regional Health – Americas, found that 11- to 12-year-olds who experienced cyberbullying were over 2.6 times more likely to report suicidal thoughts or attempts within a year. Alarmed, they were also much more likely to use substances like marijuana, nicotine, and alcohol.
Another contributing factor is disturbed sleep. The blue light from screens can interfere with melatonin levels, and emotionally stimulating content can make it hard for young users to relax at night. Poor sleep over time is very closely linked to deteriorating mental health, adding to the stress of social media use.
What is the Paradox of Connection?
Even with the bad data, social media also serves as the place where kids make and sustain friendships. During a post-pandemic era in which in-person socialization was curtailed, a number of adolescents became dependent upon social media as a lifeline. The paradox, therefore, exists in balancing the psychological detriment against the real social benefits of such sites.
This paradox is a challenge to parents, caregivers, and policymakers. Forcing adolescents away altogether is unrealistic or counterintuitive. Proactive, subtle approaches to healthier involvement are the recommendations of experts instead.
How Parents Can Take Charge and Change?
American Academy of Pediatrics (AAP) suggests the use of tools such as the Family Media Plan, which promotes open discussion and clear boundaries around screen time. "Just telling kids to 'get off your phone' doesn't really work," says Dr. Nagata. "Parents can model the way with open, nonjudgmental discussions."
Some strategies that are suggested are:
- Assigning screen times, e.g., family meals or bedtime.
- Promoting activities that are free from technology and emphasize physical and emotional health, e.g., sports, arts, or journaling.
- Watching for indicators of digital distress—mood swings, withdrawal from social interactions, and disruption of sleep patterns.
Assisting children to critically assess the information they consume, especially in terms of body image and diet fads like the recently prohibited #skinnytok on TikTok.
With over 2.4 million users of TikTok in Tennessee alone, and millions more across the country, social media is obviously not going anywhere. That doesn't mean, however, that its dangers need to be dismissed. Research such as that by UCSF is a much-needed wake-up call, compelling families as well as tech firms to recognize the mental health cost of social sites.
From inaccessible hashtags such as #skinnytok to the more subtle, mundane pressures of edited perfection, the online world is shaping the mental topography of the young in real time. Awareness, discussion, and empathy need to be at the forefront of how we steer our youngsters through this changing landscape.
The answer isn't to shut down social media, but to reimagine its place in kids' lives. Integrating scientific research with compassionate parenting and responsible technology design, we can build a world where social media supports instead of destroys because at the end of the day, it's not only about shielding our teens from depression, but empowering them with the ability to flourish, online and offline.
World’s First ‘Trojan Horse’ Blood Cancer Drug Rolled Out By NHS In England

Credits: Canva
The England National Health Service (NHS) is the world's first healthcare system to offer a revolutionary blood cancer treatment called a "Trojan horse" drug. The trailblazing treatment, officially known as belantamab mafodotin, has the potential to add years to the lives of thousands of patients fighting multiple myeloma, a vicious and currently untreatable form of bone marrow cancer.
This innovation, now being rolled out to eligible patients throughout England, highlights the revolutionary promise of precision medicine and targeted treatments to change cancer care.
How Does This Therapy Work?
At the center of this medical innovation is belantamab mafodotin, also known as Blenrep and produced by GlaxoSmithKline. In contrast to traditional chemotherapy that gets into both healthy and cancer cells, this new medication uses a targeted approach: it binds to myeloma cells, enters them quietly, and delivers a fatal dose of chemotherapy directly within, effectively killing the malignancy from the inside out.
This "Trojan horse" metaphor comes from Greek mythology, as Greek warriors entered the city of Troy disguised within a wooden horse. In the same way, this drug corrupts cancer cells by smuggling a toxic payload into them disguised as an antibody—spared most healthy tissues in the process.
NHS England National Clinical Director for Cancer Professor Peter Johnson called the treatment "life-changing" and said, "Myeloma is an aggressive blood cancer, but the advent of belantamab mafodotin brings with it a new hope of highly extended disease control.
Multiple myeloma is a plasma cancer that arises in plasma cells present in the bone marrow. Although there are continued advances in medicine, the disease is still incurable and relapsing in nature. The majority of patients have a pattern of recurrence after remission, requiring multiple treatment lines.
Trials of belantamab mafodotin, particularly in combination with other drugs such as bortezomib and dexamethasone, have shown that the treatment can stop disease from progressing for a period of three years—three years longer than the 13-month postponement achieved with the drug of choice at present, daratumumab.
The National Institute for Health and Care Excellence (NICE), having checked the effectiveness and value for money, accelerated approval for the rollout of the treatment. NICE director Helen Knight stated, "This recommendation shows our determination to get patients the best treatment quickly while protecting value for the taxpayer."
Who Will Benefit?
The NHS rollout will first address about 1,500 patients per year in England that have relapsed or are resistant to their existing treatments. These are often those with advanced myeloma who have run out of other standard treatments.
Significantly, this represents a move toward personalized, next-generation treatments being accessible through public healthcare facilities—an accomplishment welcomed by health activists and oncologists alike.
Shelagh McKinlay, Myeloma UK's Director of Research and Advocacy, hailed the announcement: "We have campaigned aggressively for the last year to get this drug approved. It will change the lives of thousands of myeloma patients."
Paul Silvester, who is 60 and from Sheffield, was diagnosed with multiple myeloma in 2023. When ordinary treatment and even a bone marrow transplant did not halt the disease, he was put on an early-access trial for belantamab mafodotin at the Royal Hallamshire Hospital.
The change was almost instant," he explained. "In the first two or three weeks following the first dose, I was in remission. I like to think this treatment has brought the party balloons into the house."
Paul is now in remission and mapping out history-themed travel excursions—something he never thought he'd ever be able to do a few months ago.
How Does Belantamab Mafodotin Work?
Belantamab mafodotin is an antibody-drug conjugate (ADC), a new class of cancer drugs. The drug's antibody component targets a protein (BCMA) on the outside of myeloma cells. After binding to the cancer cell, the complex is taken into the cell where it drops off a potent chemotherapy drug, essentially killing it from within.
This internal targeting results in much less collateral damage to normal cells—a major problem with standard chemotherapy—and decreases the overall treatment burden.
Side Effects and Safety Issues
Although thought to be less toxic than many standard therapies, belantamab mafodotin is not without adverse effects. Patients can have dry eyes, blurred vision, and occasionally more severe ocular toxicity due to the mechanism of action of the drug leaking into surrounding tissues after cell kill.
Clinical teams are trained to monitor and manage these effects, often adjusting dosage or incorporating supportive therapies to preserve patient safety.
Health Minister Karin Smyth emphasized the significance of this development: “This groundbreaking therapy puts the NHS at the forefront of cancer innovation. By harnessing cutting-edge ‘Trojan horse’ technology, we’re offering new hope to blood cancer patients across the country.”
In fact, the move by the NHS to be the first healthcare system in the world to introduce this treatment establishes a precedent for the incorporation of high-cost, high-impact biologic therapies into national care.
With its effective implementation in England, belantamab mafodotin could soon be used as a worldwide standard of care for relapsed or refractory multiple myeloma. As other nations observe outcomes and cost-effectiveness trends, it is possible that health systems globally will look into implementing this Trojan horse technique.
Researchers in oncology are also looking at similar antibody-drug conjugates for other types of cancer, including breast, lung, and ovarian cancers—implying that we are just beginning to see what this technology has to give.
© 2024 Bennett, Coleman & Company Limited

