- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
New Study Suggests People That Take Fish Oils Display Lower Aggression

Omega-3 Vitamin (Credit-Freepik)
If you’re one of the people who regularly take fish oil pills on a daily basis, research suggests that you may start displaying different behavioural symptoms as a result of your intake. The study itself is rather fascinating, conducted by a neurocriminologist, Adrian Raine, to understand whether omega-3 supplementation could substantially play a role in changing a person’s actual decision-making capabilities.
What Did Raine’s Studies Find?
The past body of research has already shown that nutrition does have a hand in assessing the probability of behavioural issues from specific demographics in the population along the lines of economic status. Now Raine’s study has unrooted evidence seems to suggest that these specific pills make enough of a change to affect decision-making capabilities.
Taking data using randomized controlled trials from 29 different countries, the study shows that there are several modest short-term effects that take place across the population, regardless of age or gender, that directly translates to a 30% reduction in aggression.
What Could The Study Mean For The Criminal Justice System
Raine doesn’t believe that his study mandates a large-scale reform across how violent crime needs to be dealt with, however he has asserted that it shows that omega-3 supplementation can reduce aggression regardless of its setting. He also highlighted the fact that the nutrient is inexpensive and relatively safe to use,
Simply adding more fish to the diet of an aggressive individual could be enough to observe changes, the paper notes. It also suggests future research to be conducted on for a more detailed analysis on how omega-3 supplementation reduces aggression, either through brain imaging techniques or comparisons with self-reported measures.
Rather than being a replacement, Raine advocates for the implementation of omega-3 nutrients as an additive to current programmes that deal with patients that display violent symptoms like psychological regimens like Cognitive Behavioural Therapy, CBT) or pharmacological supplements like risperidone. That being said, the other authors of the study do advocate for the need to study the long-term effects of the pill across other populations.
Dizzy Spells Misread as Vertigo Led to Brain Tumour Diagnosis for 63-Year-Old
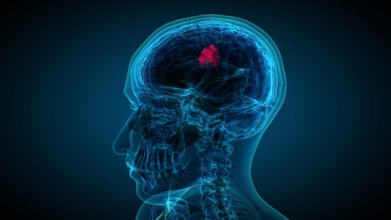
When 63-year-old John Starns slumped on a train station bench in Sevenoaks, drenched in sweat and struggling to stay upright, most passers-by assumed he was drunk. He looked wobbly, pale, and visibly disoriented. But what looked like an awkward case of public intoxication turned out to be something far more sinister: a brain tumour hiding behind symptoms commonly mistaken for vertigo.
From “It’s Just Vertigo” to “You Have a Brain Tumour”
Initially told he had vertigo, John tried to carry on with his life. But as the months passed, his dizziness became more intense and debilitating. At their worst, the episodes forced him to lie down, eyes shut, until the world stopped spinning. Still, no one suspected the real cause.Three months and one MRI scan later, John finally got the truth. He reportedly had a vestibular schwannoma, a rare, benign brain tumour sitting on the nerve that connects the brain to the inner ear. It was affecting his balance, hearing, and overall coordination, symptoms that, in hindsight, were never typical of garden-variety vertigo.
What is Vestibular Schwannoma?
Despite the intimidating name, a vestibular schwannoma is not cancerous. It develops slowly over time from Schwann cells, the fatty insulation on your nerves. In this case, the tumour formed on the vestibulocochlear nerve, which governs both hearing and balance.That is why the symptoms can masquerade as something much less serious.
- Dizziness or vertigo
- Hearing loss in one ear
- Ringing or buzzing sounds (tinnitus)
- Poor sound localisation
- In more advanced cases, numbness on one side of the face
Because these tumours grow at a glacial pace, symptoms tend to hide for months or even years. According to Cancer Research UK, they account for around 8 per cent of all brain tumours, with risk increasing significantly after the age of 65. In rare cases, they are linked to a genetic condition called neurofibromatosis, which often causes tumours on both sides of the brain.
Why Dizziness Deserves a Second Look
Most of us treat dizziness like a mild inconvenience. You get up too fast, feel woozy for a second, then go about your day. Maybe you chalk it up to dehydration, skipping breakfast, or scrolling on your phone in bed for too long. But dizziness could be a sign of something more serious.For John, it was not just one woozy episode. It was a string of unsettling, spin-the-room moments that left him lying flat on his back, eyes squeezed shut, praying for the world to stop pirouetting. And while vertigo was the first suspect, his brain had other plans, like growing a tumour on his vestibulocochlear nerve.
That is the thing with dizziness: it is vague, common, and often misunderstood. It can signal anything from low blood pressure and ear infections to neurological conditions that need serious medical attention. But because it is so easy to dismiss and hard to describe without wildly gesturing, it often gets brushed under the rug until it insists on being noticed.
If you face dizziness, do not ignore it. Especially if the dizziness is intense, recurrent, or comes with sidekicks like hearing loss, balance issues, or ringing in your ears.
Top U.S. Medical Associations Ousted from CDC Vaccine Workgroups in Sudden Shake-Up

Credits: Canva
In a controversial move that has rattled the U.S. medical community, federal health officials have severed ties with more than half a dozen major medical organizations from participating in government vaccine advisory workgroups.
The decision, communicated via email on Thursday, disinvites top experts from these groups from contributing to the workgroups that support the Advisory Committee on Immunization Practices (ACIP), a key body that guides the nation’s vaccination policies.
Organizations affected include the American Medical Association (AMA), the American Academy of Pediatrics (AAP), the Infectious Diseases Society of America (IDSA), and several others, many of whom have historically played a critical role in shaping vaccine guidelines.
“This is deeply concerning and distressing,” said Dr. William Schaffner, a renowned vaccine expert from Vanderbilt University who has been involved with ACIP workgroups for decades. “Removing these organizations will likely create conflicting messages about vaccine guidance. Patients might hear one thing from the government and another from their personal doctors.”
Longstanding Collaboration Ends Abruptly
For years, the ACIP has relied on a structured system where experts from various medical and scientific fields evaluate vaccine data and help draft recommendations. These recommendations, once approved by the Centers for Disease Control and Prevention (CDC), often inform clinical practice and determine insurance coverage.
But according to an email obtained by Bloomberg and confirmed by federal officials on Friday, the medical organizations are now being sidelined on the grounds that they are “special interest groups” and are assumed to carry a “bias” due to the populations they serve.
Dr. Schaffner defended the former system, highlighting how professional organizations offered practical insights on how recommendations could be realistically implemented in clinical settings. Importantly, all members were subject to conflict-of-interest vetting, ensuring objective guidance, he added.
Health Secretary Kennedy’s Sweeping Changes
This latest shake-up follows an earlier, unprecedented move in June when U.S. Health Secretary Robert F. Kennedy Jr. abruptly dismissed the entire ACIP panel, accusing it of being too closely aligned with vaccine manufacturers. Kennedy, a former leader in the anti-vaccine movement, has since appointed several known vaccine skeptics to the new committee.
Among the organizations removed from the workgroup process are the American Academy of Family Physicians, American College of Physicians, American Geriatrics Society, American Osteopathic Association, National Medical Association, and the National Foundation for Infectious Diseases.
In a joint statement released Friday, the AMA and several of the disinvited organizations denounced the decision, calling it “irresponsible” and “dangerous to our nation’s health.” The statement warned that excluding their medical expertise “will further undermine public and clinician trust in vaccines.”
The groups urged the administration to reverse the decision, emphasizing the importance of transparency and collaboration in public health decision-making.
Lawsuit and Fallout
Several of the ousted organizations had previously criticized Kennedy’s overhaul of the ACIP. Last month, three of them joined a lawsuit challenging the government’s decision to halt COVID-19 vaccine recommendations for most children and pregnant women, a policy shift that has been widely criticized by public health experts.
Meanwhile, newly appointed ACIP member Retsef Levi, a professor of business management with no formal medical background, defended the administration's direction on social media. Levi wrote that future workgroups would “engage experts from an even broader set of disciplines,” and claimed that membership would be based on “merit & expertise, not organizational affiliations with conflicts of interest.”
The Department of Health and Human Services (HHS) has not yet disclosed which experts will replace the disinvited members or when the new workgroups will begin operating.
US Weighs China Travel Warning As Chikungunya Cases Near 5,000: Report

Credits: Canva
The United States Centers for Disease Control and Prevention (CDC) is assessing a potential travel notice for China following a sharp rise in cases of chikungunya, a mosquito-borne viral infection that has sparked public health alarms in southern China, as reported by the Independent and the South China Morning Post.
Nearly 5,200 infections have been reported in the Guangdong province since early July, with most of them concentrated in the city of Foshan. Health officials there have since escalated their emergency response to a level III alert, which signals a “relatively major” public health threat in China’s four-tier system.
While the CDC has not yet published a formal advisory, a spokesperson told The Independent that the agency is “aware of the reported chikungunya outbreak in Guangdong Province in China and is currently assessing the size and extent of the outbreak.”
What is chikungunya?
Chikungunya is a viral infection transmitted by the bite of an infected Aedes mosquito, the same mosquito species responsible for dengue and Zika. Symptoms typically include sudden onset of fever and joint pain, but may also include headache, muscle pain, swelling, and rash.
Although most cases are mild and self-limiting, some infections can lead to prolonged joint pain or, in rare cases, long-term complications. Serious outcomes are more likely among those with pre-existing health conditions. There are no antiviral treatments available, so prevention, particularly mosquito control and bite avoidance, remains the primary approach.
Vaccines against chikungunya have recently become available and are recommended for travelers to high-risk areas, although they are not yet widely accessible.
According to local health authorities in Foshan, around 95% of reported cases have been mild, with patients recovering within a week. However, the outbreak’s rapid spread has raised concern among international health bodies.
Global spread and WHO alert
The outbreak in China follows a global pattern of chikungunya resurgence. The World Health Organization (WHO) issued an alert last week warning of the risk of the virus repeating its global spread from two decades ago. Diana Rojas Alvarez, a medical officer with WHO, said that nearly 5.6 billion people across 119 countries live in areas where the virus could potentially spread.
Chikungunya was first identified in 1952 in Tanzania and has since been detected in more than 110 countries, including major outbreaks in India, Italy, and the Americas. The virus is not spread from person to person; instead, it is carried by mosquitoes that have fed on infected individuals and then pass it to others.
The concern is not just local: international travel plays a key role in how the virus crosses borders. Infected travelers returning to or visiting countries with mosquito populations capable of transmitting the virus can trigger new outbreaks.
China’s response: Mosquito control and surveillance
The first case in this outbreak was reported in Foshan’s Shunde district on July 8 and was believed to be imported. Since then, local and national health authorities have moved quickly to contain the spread.
Measures taken include the use of drones to detect rooftop water accumulation, the release of larva-eating fish into lakes, and widespread public awareness campaigns. Residents have been urged to eliminate standing water, install window screens, and wear protective clothing.
Hospitals in affected areas have increased bed capacity for confirmed cases and designated specialized treatment centres. Border controls have been stepped up in Hong Kong to prevent imported cases from mainland China, with expanded testing capabilities introduced at key entry points.
CDC travel warnings: What it means for travelers
The CDC’s travel health notices are used to inform travelers about global disease risks and provide precautionary guidelines. The warning system has four levels, ranging from “practice usual precautions” (Level 1) to “avoid all travel” (Level 4).
As of now, China has only a Level 1 travel health notice for measles. However, the CDC has issued Level 2 notices for chikungunya in several countries including Bolivia, Kenya, and Madagascar in recent months.
If the CDC decides to escalate China’s status, it would be a significant development, both in terms of travel planning and diplomatic perception.
US–China tension and public health
The potential issuance of a travel notice also comes against the backdrop of complex US–China relations. While the CDC’s move would be grounded in public health data, the optics of a travel warning could have broader implications.
On Thursday, Chinese foreign ministry spokesperson Guo Jiakun responded to the reports, saying that China is in communication with the WHO and “making every effort to ensure a safe environment for travelers.”
The WHO has not issued any travel restrictions related to the outbreak but continues to monitor the situation closely.
A word of caution for travelers
With mosquito-borne diseases on the rise globally, driven by climate change, urbanization, and increased mobility, health experts advise travelers to stay informed and take preventive measures.
“Mosquito control is key,” said an official from the Hong Kong Centre for Health Protection. “Simple actions like using insect repellent, sleeping under mosquito nets, and avoiding stagnant water can go a long way in preventing infection.”
As global health agencies monitor the chikungunya outbreak in China, travelers to affected areas should remain vigilant and stay updated with official advisories. Prevention remains the best protection in the face of a disease with no cure.
© 2024 Bennett, Coleman & Company Limited

