- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Ozempic Came From A Monster’s Venom-The Creature That Made Weight Loss A Trend

Image Credit: Canva
Ozempic has stormed the world, grossing billions and becoming a household name not only for controlling blood sugar but also for its dramatic weight-loss effect. But before it was a celebrity-favored fad, its beginnings were anything but glamorous. This medical wonder has its roots in an unexpected place: a toxic desert lizard with a remarkable talent for living on a few meals a year—the Gila monster.
The Gila monster (Heloderma suspectum), which inhabits the deserts of North America, is famous for its slow movements and highly toxic venom. Its bite is lethal enough to kill small animals and inflict extreme pain on humans. But lurking in this venom was a breakthrough that led to Ozempic. Researchers examining the venom of the Gila monster discovered that it consisted of a novel hormone that delays digestion and modulates blood glucose levels—an advantage that enables the lizard to get by on a meager diet.
Also Read: Ozempic Users Found To Age Back By More Than 3 Years, Finds New Trial; Peer Review Pending
In the early 21st century, endocrinologist Daniel Drucker asked for a hormone that mimicked the appetite-inhibiting and blood sugar-controlling action of human glucagon-like peptide-1 (GLP-1) yet would not be quickly broken down in the body. He was prompted by the research of scientists John Eng, Jean-Pierre Raufman, and John Pisano, who had cloned the proteins in Gila monster venom and found two similar in structure to human GLP-1.
Drucker and his colleagues at the University of Toronto obtained a Gila monster from the Utah Zoo breeding program to further study its distinctive biochemistry. Their work identified Exendin-4, a protein that closely resembled GLP-1 but persisted much longer in the blood. This discovery ultimately gave rise to synthetic GLP-1 agonists, transforming the treatment of type 2 diabetes and, more recently, obesity.
Though promising, it took decades before the discovery found its way into an FDA-approved drug. The initial GLP-1 agonist based on Gila monster venom was approved to treat diabetes in 2005. The two decades that followed saw the formulation of more advanced drugs such as semaglutide, which is the active component in Ozempic and its weight loss equivalent, Wegovy.
Also Read: What Is Ozempic Smell? Another Unusually Side Effect Your Weight-Loss Injection Might Come With
Now, millions depend on Ozempic to control diabetes and shed pounds, with demand so great that worldwide shortages have been reported. Its popularity has created a surge in off-label use, with social media spreading trends of dramatic weight loss among celebrities and influencers. But the tale of Ozempic is only one illustration of how nature's most toxic animals have led to life-saving medical breakthroughs.
Other Drugs that Came from Poisonous Animals
Ozempic is hardly the first life-saving medication to be developed from the animal world's toolkit of toxins. From the beginning of time, scientists have turned to nature to find answers to human illnesses, and in the process, have developed some of the most crucial medical advances.
One of the highest-selling medicines in the world, Lisinopril, has its roots in the Brazilian viper (Bothrops jararaca). The venom from the snake includes enzyme inhibitors that inhibit the blood of its prey from clotting so the venom can travel quickly. Researchers took this process and developed angiotensin-converting enzyme (ACE) inhibitors, which decrease blood pressure and are commonly used to treat heart disease and hypertension.
Far down in the ocean, the Caribbean sea sponge (Tectitethya crypta) has been secretly making substances that defend it from foreign DNA brought by predators and prey. Those unusual nucleosides were the foundation for cytarabine, a drug used to treat leukemia and non-Hodgkin's lymphoma through chemotherapy. This discovery reaffirmed the belief that even the most basic life forms can be the solution to revolutionary cures.
In a breathtaking illustration of the paradoxical position of nature in medicine, deathstalker scorpion venom (Leiurus quinquestriatus) brought about the solution to the treatment of brain tumors. A team led by oncologist Jim Olson found that a peptide found in the venom, chlorotoxin Cy5.5, attaches itself only to brain tumor cells and leaves healthy tissue intact. This resulted in the creation of Tozuleristide, a fluorescent tag that aids surgeons in precise identification and resection of cancerous tissue.
The popularity of Ozempic and other venom-based medications indicates the yet unutilized potential of the biochemistry of nature. From fungal-sourced antibiotics to animal-venom-derived painkillers, researchers are learning every day about the possibilities for leveraging the might of nature. Researchers now search for potential new treatments for neurological conditions, pain, and heart disease from the spider venom, cone snail toxin, and even the bat's saliva.
But these findings are also a harsh reminder that most of these species are threatened by habitat loss, climate change, and human use. The Gila monster, for instance, is threatened by land development and wildlife trade. Conservation of these species and their habitats is not only a conservation issue, it is an issue of future medical advancement as well.
The Invisible “Brain-Eating” Bacteria Lurking in Water Pipes That Can Cause Deadly Infections
Credit: Canva
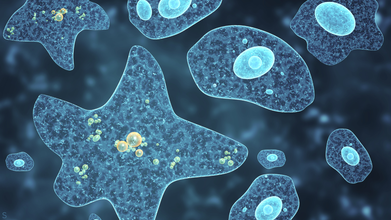
Environmental and public health scientists have begun warning against the dangers of having free living amoeba in water systems that are capable of triggering severe diseases in humans.
In a recent perspective article published in Biocontaminant, the researchers noted that climate change, deteriorating water infrastructure and limited systems for monitoring and detection are the key factors that have allowed these pathogens to spread and persist.
Corresponding author Longfei Shu of Sun Yat sen University explained: "What makes these organisms particularly dangerous is their ability to survive conditions that kill many other microbes.
"They can tolerate high temperatures, strong disinfectants like chlorine and even live inside water distribution systems that people assume are safe."
The scientists also emphasized that not only can amoebae spread illnesses on its own, it can also act as hidden carriers for other harmful microbes.
By sheltering bacteria and viruses inside their cells, amoeba these unicelled organisms protect these pathogens from disinfection and help them persist and spread in drinking water systems. This so-called Trojan horse effect may also contribute to the spread of antibiotic resistance among humans.
How Dangerous Is Amoeba?
Amoeba are single-celled organisms that naturally live in soil and water. Most species do not cause harm yet some can prove to be fatal.
Some of the diseases caused by this kind of bacteria include Amebiasis (Amoebic Dysentery), an intestinal infection by Entamoeba histolytica, causing diarrhea, cramps and potential liver abscesses as well as Primary Amoebic Meningoencephalitis (PAM) from Naegleria fowleri, a rare but nearly always fatal brain infection from contaminated water entering the nose.
Effects of amoeba-caused infections range from intestinal issues (liver abscesses, anemia, peritonitis) to severe neurological damage (coma, seizures, death) from brain-eating types, with Acanthamoeba causing eye infections (keratitis).
Experts recommend thoroughly washing your hands after toilet use and before handling food, drinking clean water especially in unsanitary conditions and avoiding getting water up your nose in warm freshwater to prevent such infections.
The Indore Crisis
This comes days after the recent Indore sewage water controversy which has claimed the lives 10 people and left over 1,400 people hospitalized, according to Indore Mayor Pushyamitra Bhargava.
However, locals claim that the outbreak has instead caused the death of 17 residents, including a six-month-child. The situation has also left Parvati Bai, 67, with kidney failure, a brain stroke and symptoms of Guillain-Barré Syndrome, or GBS.
GBS is a rare condition where your immune system attacks the nervous system and can cause paralysis as well as death, in certain cases.
The outbreak occurred due to lapses in civic infrastructure. Investigation revealed that a toilet constructed directly above a main drinking pipeline near a police outpost, without a mandatory safety tank resulted in the sewage mixing with drinking water.
New FDA Approved Blood Test Can Predict Alzheimer’s Disease Before Symptoms Appear

Credit: Canva
The US Food and Drug Administration has approved the use of a blood test which can help diagnose Alzheimer’s disease in adults aged 55 and above.
The blood test, known as Lumipulse, can detect amyloid plaques associated with Alzheimer’s disease and has proven to be a “less invasive option” that “reduces reliance on PET scans and increases diagnosis accessibility.”
FDA Commissioner Martin A. Makary said of the landmark decision, "Alzheimer’s disease impacts too many people, more than breast cancer and prostate cancer combined.
"Knowing that 10% of people aged 65 and older have Alzheimer's, and that by 2050 that number is expected to double, I am hopeful that new medical products such as this one will help patients."
It remains unclear when this test will be available for commercial use across the world.
What Is Alzheimer’s Disease?
Alzheimer's disease is one of the most common forms of dementia and mostly affects adults over the age of 65.About 8.8 million Indians aged 60 and above are estimated to being living with Alzheimer's disease. Over seven million people in the US 65 and older live with the condition and over 100,00 die from it annually.
Alzheimer's disease is believed to be caused by the development of toxic amyloid and beta proteins in the brain, which can accumulate in the brain and damage cells responsible for memory.
Amyloid protein molecules stick together in brain cells, forming clumps called plaques. At the same time, tau proteins twist together in fiber-like strands called tangles. The plaques and tangles block the brain's neurons from sending electrical and chemical signals back and forth.
Over time, this disruption causes permanent damage in the brain that leads to Alzheimer's disease and dementia, causing patients to lose their ability to speak, care for themselves or even respond to the world around them.
While there is no clear cause of Alzheimer's disease, experts believe it can develop due to genetic mutations and lifestyle choices, such as physical inactivity, unhealthy diet and social isolation.
Early symptoms of Alzheimer's disease include forgetting recent events or conversations. Over time, Alzheimer's disease leads to serious memory loss and affects a person's ability to do everyday tasks.
There is no cure to this progressive brain disorder and in advanced stages, loss of brain function can cause dehydration, poor nutrition or infection. These complications can result in death.
How Does The Test Work?
Lumipulse detects amyloid plaques and tangles in blood plasma and calculates the numerical ratio of the levels of the two proteins. Based on the ratio, the test shows a positive or negative result for the disease.As explained by Dr Abhay Moghekar, an associate professor of neurology at Johns Hopkins University School of Medicine, who helped study and evaluate the test for FDA approval, "If this test is positive, there’s a greater than 90% chance that you have amyloid plaque in your brain.
"Getting a blood test is gonna be far easier, quicker and cheaper,” he said. “It’s going to allow early access to therapy, so it is going to revolutionize care of patients with dementia."
However, the federal agency also noted certain limitations associated with the test such as it can only be used for patients 55 and older who are already experiencing memory problems.
The FDA also cautions that the test is not intended as a standalone diagnostic tool for Alzheimer’s and results should be interpreted based on the patient’s medical history and other assessments, such as cognitive testing.
What Happens When You Stop Using Weight Loss Injections?

Credit: Canva
People who stop using weight-loss medications can regain weight and return their original size within two years, a new BMJ study says.
Researchers have found that those who lose weight using blockbuster GLP-1 drugs such as Ozempic could regain about 0.4kg every month after quitting these treatments. In contrast, those who lost weight through exercise, diet and other factors only gained 0.1kg.
Investigator Dr Susan Jebb, from Oxford University told the BBC, "People buying these need to be aware of the risk of fast weight regain when the treatment ends."
Ozempic (semaglutide) is a prescription injectable GLP-1 medication primarily approved for adults with Type 2 diabetes to manage blood sugar levels. However, the drug has gained immense popularity among those trying to lose weight as it can reduce hunger and help people feel full for longer, which forces the body to burn fat deposits to stay functional.
In clinical trials, people with obesity using semaglutide have shown to lose an average of about 15% of their body weight over 68 weeks. Most people begin to see noticeable results within 8 to 12 weeks of taking the drug.
The official price in India for a once-weekly Ozempic injection pen ranges from approximately ₹8,800 for the 0.25 mg dose to around ₹11,175 for the 1 mg dose per month. Insurance coverage is generally inconsistent for weight loss indications.
What Did The Study Find?
The researchers analyzed 37 studies that included 9,341 participants out of which nearly half had taken had taken GLP-1 medications. This included 1,776 people who received the newer, more effective drugs semaglutide, sold as Ozempic and Wegovy by Novo Nordisk , and tirzepatide, sold as Mounjaro and Zepbound by Eli Lilly.
Apart from discovering that patients could regain all their weight in 1.7 years, the scientists also found that those who lost weight using semaglutide and tirzepatide, cwould gain 0.8 kg per month.
Dimitrios Koutoukidis, Oxford University researcher and senior study author, “But because people on semaglutide or tirzepatide lose more weight in the first place, they all end up returning to baseline at approximately the same time".
Heart health risk factors, such as blood pressure and cholesterol levels, that benefited from the drugs were projected to return to pre-treatment levels within 1.4 years after stopping the medications.
Why Does The Weight Come Back?
Dr Adam Collins, an expert in nutrition at the University of Surrey, told the BBC that when the body stops receiving a regular dose of appetite suppressants such as GLP-1 drugs, hunger returns and can lead to overeating.
He told the publication, "Artificially providing GLP-1 levels several times higher than normal over a long period may cause you to produce less of your own natural GLP-1, and may also make you less sensitive to its effects.
"That's not a problem when taking the drugs, but as soon as you withdraw this GLP-1 'fix', appetite is no longer kept in check and overeating is far more likely.
"This is further exacerbated if the individual in question has relied solely on GLP-1 to do the heavy lifting... artificially suppressing their appetite without them establishing any dietary or behavioural changes that would help them in the long run."
© 2024 Bennett, Coleman & Company Limited

