- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
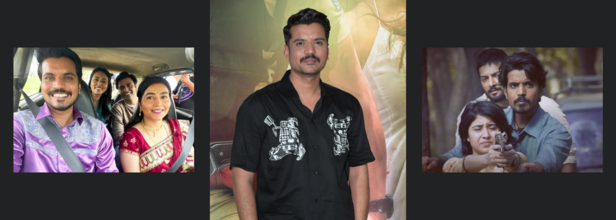
Panchayat's Asif Khan Suffers From A Heart Attack, Shares Updates
Credits: Canva
Actor Aasif Khan, known for his performances in Pataal Lok and Panchayat, recently suffered a heart attack and was admitted to Kokilaben Hospital in Mumbai. The incident occurred two days ago, sending a wave of concern among his fans and industry peers. Fortunately, his condition is now stable.
According to hospital sources, Aasif is recovering well and is likely to be discharged in a couple of days.
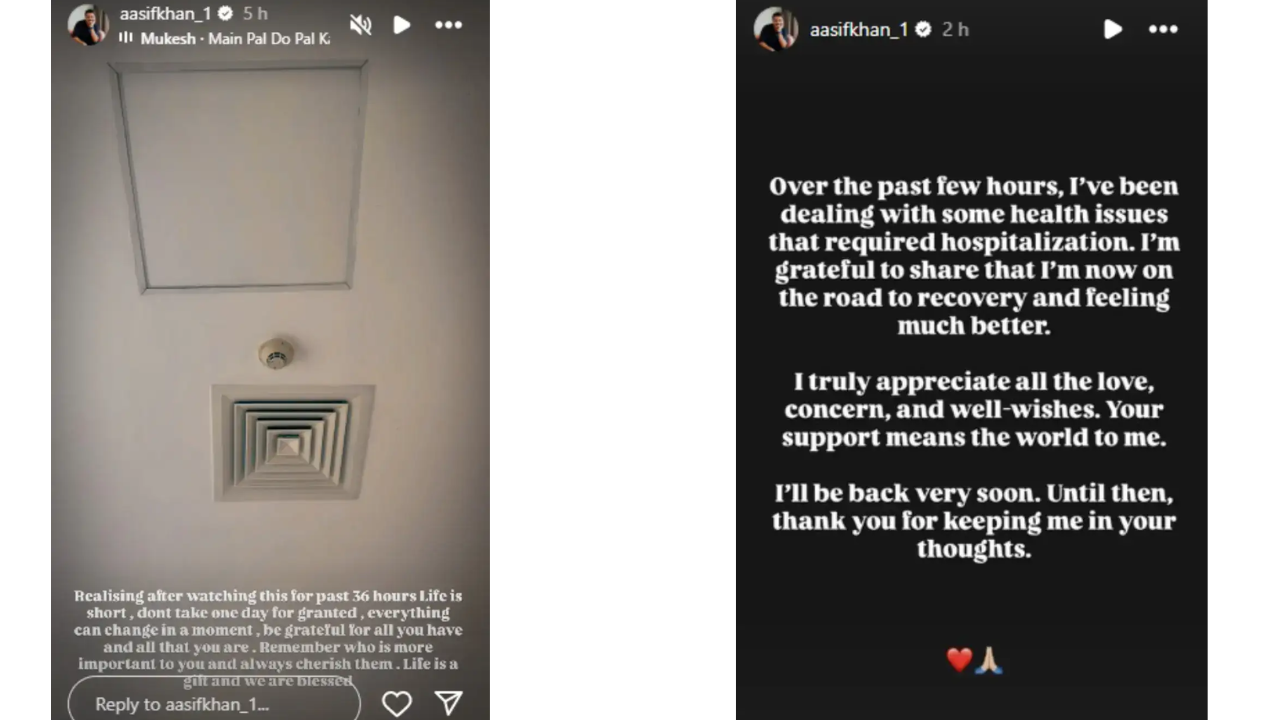
The actor took to his Instagram stories to share an update, along with a photo from his hospital bed. In a deeply reflective note, he wrote:
“Life is short, don’t take one day for granted. Everything can change in a moment. Be grateful for all you have and all that you are… Life is a gift and we are blessed.”
Recovering From Attack
In a brief statement to India Today, Aasif confirmed he had been dealing with a health issue that required hospitalization.
“I’m grateful to share that I’m now on the road to recovery and feeling much better,” he said. “I truly appreciate all the love, concern, and well-wishes. Your support means the world to me. I’ll be back very soon.”
His update comes as a reminder of how sudden and serious heart-related conditions can be—even among young and seemingly healthy individuals.
How Do Heart Attacks Happen?
A heart attack, or myocardial infarction, occurs when blood flow to a part of the heart is blocked, usually by a clot, causing damage to the heart muscle. It’s often linked to lifestyle factors like high cholesterol, smoking, stress, and lack of exercise—but can also strike unexpectedly.
While heart attacks are more common in those over 50, studies show a rising number of younger adults are now at risk. According to a 2019 study published in the Journal of the American College of Cardiology, one in five heart attack patients in the U.S. was under the age of 40.
In India, the numbers are more alarming. The Indian Heart Association notes that 50% of all heart attacks in Indian men occur under the age of 50, and 25% occur under the age of 40. Factors like sedentary lifestyles, unhealthy diets, and high stress contribute significantly.
Signs to Watch For
Aasif’s case highlights the importance of recognizing the early symptoms of a heart attack, which can include:
- Chest pain or tightness
- Pain in the left arm, jaw, or upper back
- Shortness of breath
- Cold sweat or nausea
- Unusual fatigue or lightheadedness
If any of these symptoms occur, immediate medical attention is essential. Early intervention can save lives.
For now, Aasif Khan’s fans and colleagues continue to send him strength and support. And as he put it, he’ll be “back very soon”—with renewed gratitude and, hopefully, greater awareness for all.
FDA Recalls Popular Chocolate Snack Over Laceration Risk: What You Need To Know

Credits: Canva
True Fru product recall: The U.S. Food and Drug Administration (FDA) announced that Tru Fru, LLC is voluntarily recalling certain Tru Fru freeze-dried products due to the possible presence of metal. The recall was prompted by Georgia Nut Company, which manufactures these products for Tru Fru, after a customer raised concerns.
Tru Fru produces chocolate-covered fruit snacks, including freeze-dried and frozen fruits like strawberries, bananas, and pineapple, coated in dark, milk, or white chocolate, and some varieties with peanut butter.
True Fru Product Recall: How To Recognize the Recalled Items?
The FDA published the recall notice on September 29, 2025. It covers specific batches of Tru Fru Freeze-Dried Strawberries in Dark & White Chocolate and Strawberries & Crème, available at major retailers nationwide, including Albertson’s, CVS, Food Lion, H-E-B, Hungryroot, Ingles Markets, Kroger, Stew Leonard’s, and Target, as per All Recipes.
To check if your product is affected, look for the 10-digit manufacturing code on the back of the package. The first four characters of the code identify the recalled batches.
Affected Products Include:
1) Tru Fru Freeze-Dried Strawberries in Dark & White Chocolate (3.4 oz)
UPC: 850048358270 | Item #: 10300458
Manufacturing codes starting with: 517B–532B (see full list above)
2) Tru Fru Freeze-Dried Strawberries in Dark & White Chocolate (1.7 oz)
UPC: 850048358331 | Item #: 10300442
Manufacturing codes starting with: 514A–526A
3) Tru Fru Freeze-Dried Strawberries in Dark & White Chocolate (13 oz)
UPC: 850048358379 | Item #: 10300474
Manufacturing codes starting with: 515A–516C
4) Tru Fru Freeze-Dried Strawberries & Crème (3.4 oz)
UPC: 850048358249 | Item #: 10300455
Manufacturing codes starting with: 520B–524E
True Fru Product Recall: What Did The Company Say?
The company warned that hard or sharp foreign objects in their food products could cause injuries, including cuts or punctures to the mouth, tongue, throat, stomach, or intestines, as well as damage to teeth and gums. The recall affects products distributed across the U.S. at major retailers such as Albertson’s, CVS, Food Lion, H-E-B, Hungryroot, Ingles Markets, Kroger, Stew Leonard’s, and Target. The recall was prompted by a customer report, and so far, no injuries or illnesses have been reported according to the FDA.
True Fru Product Recall: What to Do If You Have A Recalled Product?
Do not eat any of the recalled items. They should be discarded immediately. Customers seeking compensation can fill out Tru Fru’s online form to receive a coupon. No injuries have been reported so far, but if you have any concerns, contact your doctor. Swallowing metal pieces can cause cuts or tears in the mouth, throat, stomach, or intestines, and can damage teeth or gums.
Tru Fru is not the only recent recall due to foreign object risks. The USDA recently issued a health alert for a ready-to-eat pasta meal sold at Walmart because of possible listeria contamination.
The recalled product is Marketside Linguine with Beef Meatballs and Marinara Sauce, sold in 2 oz plastic trays. The affected “best if used by” dates are September 22, 24, 25, 29, 30, and October 1, 2025. These were sold nationwide at Walmart. Consumers are advised not to eat the pasta and should either throw it away or return it for a full refund.
Premature Baby In Alberta Dies From Measles As Cases Rise In Canada

(Credit-Canva)
The province of Alberta has reported its first death linked to measles since the highly contagious virus resurfaced in Canada. An infant died shortly after birth when the mother had contracted measles during pregnancy. This tragic event follows a similar case in Ontario in June. Health Minister Adriana LaGrange called the loss "heartbreaking" and urged the public to take protective steps, emphasizing the extreme risks posed by measles to certain groups.
The National Foundation for Infectious Diseases (NFID) explains that measles is a highly contagious disease caused by a virus. This virus lives in the mucus found in a sick person's nose and throat.
Measles spreads very easily through the air when an infected person coughs, sneezes, or talks. Up to 90% of people nearby who haven't had the vaccine will likely get infected. A sick person can spread measles to others starting four days before the rash appears and for four days after it appears.
Are Measles Cases Rising?
According to the Government of Alberta, measles is back, and it's spreading quickly. Since March, there have been nearly 2,000 cases reported in Alberta. This is a huge number for a disease that was supposed to be gone from the country since 1998.
Most of the sickness is happening in the southern and northern parts of Alberta. More than 150 people have been so sick they needed to be admitted to the hospital. Out of those, 15 people needed care in the intensive care unit (ICU).
Who is Getting Infected With Measles?
The vast majority of the people who have gotten sick are children and teenagers. The data shows that 89% of those infected had not been vaccinated against measles. Measles spreads so easily that just one sick person can infect up to 18 people who haven't had their shots.
How Serious Is Measles?
The NFID explains that about 1 out of 5 unvaccinated people in the U.S. who get measles will need to be hospitalized. This risk is highest for children under age five.
- 1 out of every 1,000 people with measles will get brain swelling, which can cause permanent brain damage.
- As many as 1 out of 20 children with measles will get a serious lung infection called pneumonia.
- Sadly, 1 to 3 out of every 1,000 people who get measles will die.
The number of cases has been high recently. As of October 2025, there have been 1,544 confirmed cases across 42 US states, with three confirmed deaths. This is the highest number of cases since the disease was eliminated (gotten rid of) in the U.S. in the year 2000. Most of these recent cases (92%) were in people who were not vaccinated.
Measles Symptoms and Immune System Risk
Measles is one of the easiest viruses to catch because it travels through the air. You can get it just by breathing the air near a sick person.
The symptoms to watch for are:
- A very high fever.
- A cough, a runny nose, or red, watery eyes.
- A classic rash that starts on the face and spreads down the body.
Measles can give your immune system "amnesia," which means it wipes out the memory of old infections. You become vulnerable again to common sicknesses like the flu or colds that you had already fought off and beaten in the past. This makes you more likely to get seriously ill from other things for months or even years after you recover from the measles.
How Can You Prevent Measles?
The best defense against measles is the vaccine. The shot is very good at stopping the infection and is free in Alberta.
Before Getting Pregnant
If you are planning to have a baby, you should make sure you have had two doses of the measles vaccine before you get pregnant. You cannot get the shot while pregnant.
Check Your Status
If you don't know if you've been vaccinated, you can call 811 (Health Link) for free information.
Trump Administration Quietly Approves Abortion Pill Mifepristone Amid RFK Jr.’s FDA Safety Review

Credits: Canva
The Trump administration has quietly approved a new generic version of the abortion pill mifepristone, a move announced by the Food and Drug Administration this week that has drawn sharp criticism from anti-abortion leaders.
The decision comes less than two weeks after Health and Human Services Secretary Robert F. Kennedy Jr. and FDA Commissioner Martin Makary confirmed a review of abortion pill safety, a review initially welcomed by anti-abortion activists. Now, those same leaders are questioning the administration’s commitment to their cause, marking one of the first notable pushbacks Trump has faced from his usually loyal socially conservative base.
Trump Administration Quietly Approves Generic Mifepristone, Sparking Backlash
Federal regulators have approved a new generic version of the abortion pill mifepristone, a routine regulatory step that immediately drew criticism from anti-abortion groups and politicians aligned with the Trump administration.
The approval was announced by Evita Solutions, the drugmaker, on its website. The company’s low-cost version of mifepristone is approved for ending pregnancies up to 10 weeks gestation. Students for Life Action, an anti-abortion organization, responded to the news calling the move “a stain on the Trump presidency” and describing it as further evidence that the “deep state at the FDA must go.”
The decision shows the ongoing tension between expanding access to abortion medication and opposition from socially conservative groups who remain critical of regulatory agencies’ role in approving such drugs.
What Is Mifepristone?
According to the FDA, mifepristone blocks the hormone progesterone, which is essential for a pregnancy to continue. Used in combination with misoprostol, it can safely end an intrauterine pregnancy up to ten weeks gestation (70 days or less since the first day of the last menstrual period).
The approved dosing schedule is:
- Day 1: 200 mg of mifepristone taken orally
- 24–48 hours later: 800 mcg of misoprostol taken buccally (in the cheek) at an appropriate location
- 7–14 days later: follow-up with a healthcare provider
Mifepristone: Who Will Make It?
The generic version will be produced by Evita Solutions LLC, a company that says its mission is to “normalize abortion” and make it “accessible to all.” The FDA confirmed the approval, stating that the submitted application contained sufficient data to meet federal standards.
Mifepristone: Safety and Controversy
Decades of peer-reviewed studies show that serious adverse reactions to mifepristone occur in fewer than 0.5 percent of patients, and the drug has been FDA-approved and widely used for over 20 years.
Despite this, earlier this year, a report by the Ethics and Public Policy Center, a right-wing think tank, questioned the safety of the pill, claiming serious complications were 22 times higher than previous estimates and urging the FDA to reconsider its approval.
This latest approval underscores the ongoing tensions in U.S. abortion politics, as the Trump administration’s decision to quietly greenlight generic mifepristone clashes with the expectations of socially conservative supporters.
© 2024 Bennett, Coleman & Company Limited

