- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Robert F. Kennedy Jr.’s 8 Most Controversial Health Declarations As Potential US Health Secretary
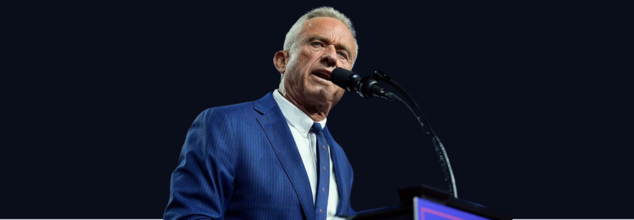
Robert F. Kennedy Jr.’s 8 Most Controversial Health Declarations As Potential US Health Secretary
Robert F. Kennedy Jr., known for his outspoken and often polarizing health views, has once again drawn attention with his potential appointment as health secretary under Donald Trump’s administration. While Kennedy has championed issues like pharmaceutical reform and food safety, many of his claims have been widely criticized as misleading or scientifically debunked. Here's a closer look at some of the most controversial statements Kennedy has made on health-related topics.
1. Vaccines and Autism
Kennedy has been a leading figure in the anti-vaccine movement, frequently questioning the safety and efficacy of routine vaccinations. He has perpetuated the long-debunked theory linking the measles, mumps, and rubella (MMR) vaccine to autism, based on a retracted study by Andrew Wakefield. Despite overwhelming scientific evidence disproving this link, Kennedy has persisted, even calling the COVID-19 vaccine "the deadliest vaccine ever made," a claim contradicted by extensive safety data.
2. Raw Milk Advocacy
Kennedy openly supports consuming raw milk, asserting its natural benefits. However, public health experts warn that raw milk can harbor dangerous pathogens, increasing the risk of foodborne illnesses. The CDC advises against its consumption, particularly amid the ongoing bird flu outbreak, which poses additional risks to dairy products.
3. Fluoride and Public Health
Kennedy has claimed that fluoride in drinking water is associated with serious health conditions, including arthritis, bone cancer, and IQ loss. However, leading health organizations like the CDC and the American Academy of Pediatrics maintain that regulated fluoride levels are safe and play a significant role in preventing cavities. Documented risks are limited to cosmetic dental issues.
4. Stem Cell Suppression
Kennedy has criticized the FDA for what he calls the "aggressive suppression" of stem cell therapies. While stem cell research holds promise for treating various illnesses, the FDA has targeted certain clinics for making unsubstantiated claims about unapproved treatments, prioritizing public safety over unregulated advancements.
5. Racist and Antisemitic COVID Claims
In one of his most controversial remarks, Kennedy suggested that COVID-19 was designed to target certain ethnic groups, sparing Ashkenazi Jews and Chinese populations. These baseless theories have been widely condemned, as public health experts attribute disparities in COVID-19 impacts to socioeconomic factors rather than genetic immunity.
6. Cellphone Radiation
RFK Jr. has suggested a link between cellphone radiation and cancer, a claim lacking definitive evidence according to the FDA and the National Cancer Institute.
7. HIV and AIDS
Kennedy has attributed AIDS to lifestyle factors rather than the scientifically established cause, HIV. Kennedy has falsely suggested that AIDS was caused in part by “heavy recreational drug use in gay men and drug addicts.”
8. Antidepressants
He has amplified unproven theories linking antidepressant use to mass shootings, a claim dismissed by mental health experts.
If confirmed as health secretary, Kennedy would oversee critical agencies, including the CDC and FDA. His controversial track record raises questions about the future direction of U.S. public health policy. With health misinformation already a pressing global concern, Kennedy’s leadership could significantly impact how health crises are managed and communicated.
As the debate over his appointment unfolds, the public health community remains watchful, emphasizing the importance of science-backed decisions in safeguarding public health.
Influenza A: After Three Child Deaths, Health Officials Urge Flu Vaccination in Canada

Credits: Canva
Three children from Ottawa and Eastern Ontario have died due to flu-related complications over the past two weeks, as an unusually early and aggressive flu season grips the region. Health officials have confirmed that the cases are linked to Influenza A, a strain currently circulating widely and affecting children more severely than usual, as per CTV news.
The children were between five and nine years old. Authorities have not released further personal details about the two Ottawa cases and one case from Eastern Ontario.
What Is Influenza A?
Influenza A is a fast-spreading respiratory virus responsible for seasonal flu outbreaks and, at times, global pandemics. It changes quickly through genetic shifts, which makes new strains harder to predict and control. The virus is grouped based on surface proteins called hemagglutinin and neuraminidase, with H1N1 and H3N2 among the most common strains in circulation. It spreads mainly through coughs, sneezes, or close contact and often comes on suddenly, causing fever, cough, body pain, and extreme tiredness. In some cases, it can lead to serious complications, especially in vulnerable groups.
Influenza A: Health Officials Call Deaths a Serious Warning
Public health leaders from Ottawa and Eastern Ontario described the deaths as a troubling reminder of how dangerous the flu can be, especially for children.
“This highlights that influenza is not always a mild illness. It can lead to serious complications that require hospitalization,” medical officers of health from both regions said in a joint statement issued on Monday, as per CTV News.
Influenza A: Child Flu Deaths Rare but Not Unprecedented in Canada
While flu-related deaths among children are uncommon in Canada, they are not unheard of. During the last severe flu season in 2022, two children in Ottawa died due to influenza.
Most flu-related deaths in Canada occur among older adults. Of the estimated 3,500 flu deaths reported nationwide each year, roughly 90 percent involve people over the age of 65. However, experts say the current Influenza A strain is behaving differently.
Influenza A Hitting Children Hard This Season
The strain of Influenza A currently circulating has been linked to a sharp rise in severe pediatric flu cases globally. Health officials say the cluster of three child deaths within such a short period, and within a relatively small geographic area, is highly unusual.
This unusual pattern prompted the regional coroner to alert public health authorities after three sudden, unexpected child deaths tested positive for Influenza A.
“It’s rare for the coroner to reach out like this,” said Dr. Trevor Arnason, Ottawa’s medical officer of health. “But this season has been particularly severe.”
Influenza A: Hospitals Strained as Pediatric Cases Rise
CHEO, Ottawa’s children’s hospital, has reported high numbers of children falling seriously ill with the flu since November. Hospitalizations have continued to rise through early December.
Last week, CHEO issued an urgent request asking family doctors to extend clinic hours and assist at the hospital’s Kids Come First clinic to help manage patient volumes.
Hospital officials have also noted that many children arriving at the emergency department with severe flu symptoms had not been vaccinated.
Influenza A: Strong Push for Flu Vaccination as Cases Surge
Public health officials, including Ontario’s Chief Medical Officer of Health Dr. Kieran Moore, are urging everyone aged six months and older to get vaccinated as soon as possible.
Dr. Arnason and Dr. Paul Roumeliotis, medical officer of health and CEO of the Eastern Ontario Health Unit, stressed that vaccination is especially important for children this season.
Influenza A: Vaccine Still Effective Despite Strain Mutation
Some people have expressed concern after reports suggested this year’s flu vaccine is not a perfect match for the circulating Influenza A strain. Health officials clarified that while the virus has mutated slightly since circulating in the southern hemisphere, the vaccine still offers meaningful protection.
“The flu vaccine may not always prevent infection, but it significantly reduces the risk of severe illness, hospitalization, and complications,” officials said. They added that the vaccine takes about two weeks to become fully effective, making early vaccination crucial ahead of the holiday season, when virus spread typically increases.
You're Breathing Your Way Into Diabetes

AIIMS Study Finds No Evidence Linking COVID-19 Vaccination To Sudden Deaths In Young Adults

Credits: Canva
There has been a long-running belief that COVID-19 vaccines are behind sudden deaths in young adults. Posts circulating on social media and unverified online claims have repeatedly linked vaccination to sudden collapses, heart attacks, or unexpected deaths, particularly among people aged 18 to 45 who seemed otherwise healthy.
These claims have caused anxiety among families, despite the absence of solid scientific backing. A new study published by AIIMS now brings much-needed clarity on whether COVID vaccines have any connection to sudden deaths in young adults.
Also Read: Can Overusing Air Purifiers Harm Your Lungs? Expert Explains
AIIMS Study Finds No Link Between Covid Vaccination And Sudden Deaths In Adults
Worries around sudden deaths in young adults have increased in recent years, especially in the period following the COVID-19 pandemic. Speculation blaming COVID vaccines gained traction across platforms, adding to public concern. However, fresh findings from a study carried out by the All India Institute of Medical Sciences (AIIMS), New Delhi, offer a clear answer. After examining detailed autopsy reports, researchers concluded that underlying heart disease, and not COVID-19 vaccination, is the leading cause of sudden deaths in younger individuals.
Heart Problems Leading Cause Among Deaths In Young People
The AIIMS study found that heart-related conditions were responsible for 42.6 per cent of sudden deaths among people aged 18 to 45 years. Within this group, heart attacks accounted for nearly 85 per cent of cardiac-related deaths. Other contributing factors included structural abnormalities of the heart, congenital defects, and inflammation of the heart muscle. Respiratory illnesses made up around 21.3 per cent of sudden deaths, with choking, pneumonia, and tuberculosis emerging as the main causes. In close to one-fifth of the cases, doctors were unable to determine the exact cause of death.
No Evidence Linking Deaths To Covid Or Vaccines
Crucially, the researchers observed no meaningful rise in sudden deaths among individuals who had previously contracted COVID-19 or received the vaccine. Of the cases analysed, only 4.3 per cent had a history of COVID infection, while 82.8 per cent had been vaccinated. Dr Sudheer Arava, Professor of Pathology at AIIMS, explained that the year-long study reviewed nearly 100 cases and found no signs of vaccine-related complications, with just one instance of myocarditis reported. The findings also pointed to differences across age groups.
Among those aged 46 to 65, nearly three-quarters of sudden deaths were linked to heart disease, while unexplained deaths were far fewer. Notably, the proportion of women among sudden deaths was higher in the younger age group than among older adults. The study carries weight as it directly challenges claims blaming COVID-19 vaccines for sudden deaths.
Doctors emphasise that lifestyle-related issues such as unhealthy eating habits, lack of physical activity, and chronic stress continue to play a major role in heart disease among younger people. This, they say, highlights the importance of early prevention and regular health screenings. Dr Arava also urged the public to rely on credible scientific information and steer clear of misinformation that could erode trust in proven public health measures, including vaccination.
© 2024 Bennett, Coleman & Company Limited

