- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Scott Swift, Taylor Swift's Dad Underwent A Quintuple Bypass Heart Surgery, Here's What We Know About It So Far
Credits: Treemily
Scott Swift, 73, pop singer Taylor Swift's dad just underwent a quintuple bypass surgery, revealed Taylor during one of the episodes of Travis Kelce and Jason Kelce's New Heights podcast.
She also shared that she had moved in with her dad earlier this year to take care of him for a speedy recovery. She noted that her father has been full of gratitude after the surgery. "He was the loveliest patient ever. He just kept saying thank you over and over again."
Why Did Scott Swift Need A Surgery?
Taylor called the surgery "really intense" and said that her dad's heart always had a healthy ECG or electrocardiogram. He also ensures to get it every year to remain a step ahead of any physical ailments. However, five hard blockages were found in his heart during a resting stress test.
"He's been telling all his friends, 'You need to get the stress test,' because that's what's actually preventative. If you can find that earlier, you don't have to have a bypass surgery," she said.
Taylor confirmed that her father is doing "incredibly well" and that his humor has helped him go through during the hard times. It still is very much intact in him.
She shares that he did not know how many blockages he's had, on being told that he underwent a quintuple bypass, which means five blockages, he also joked about it. "Well, you see, I come from a very competitive family," he told Taylor.
What Is A Stress Test?
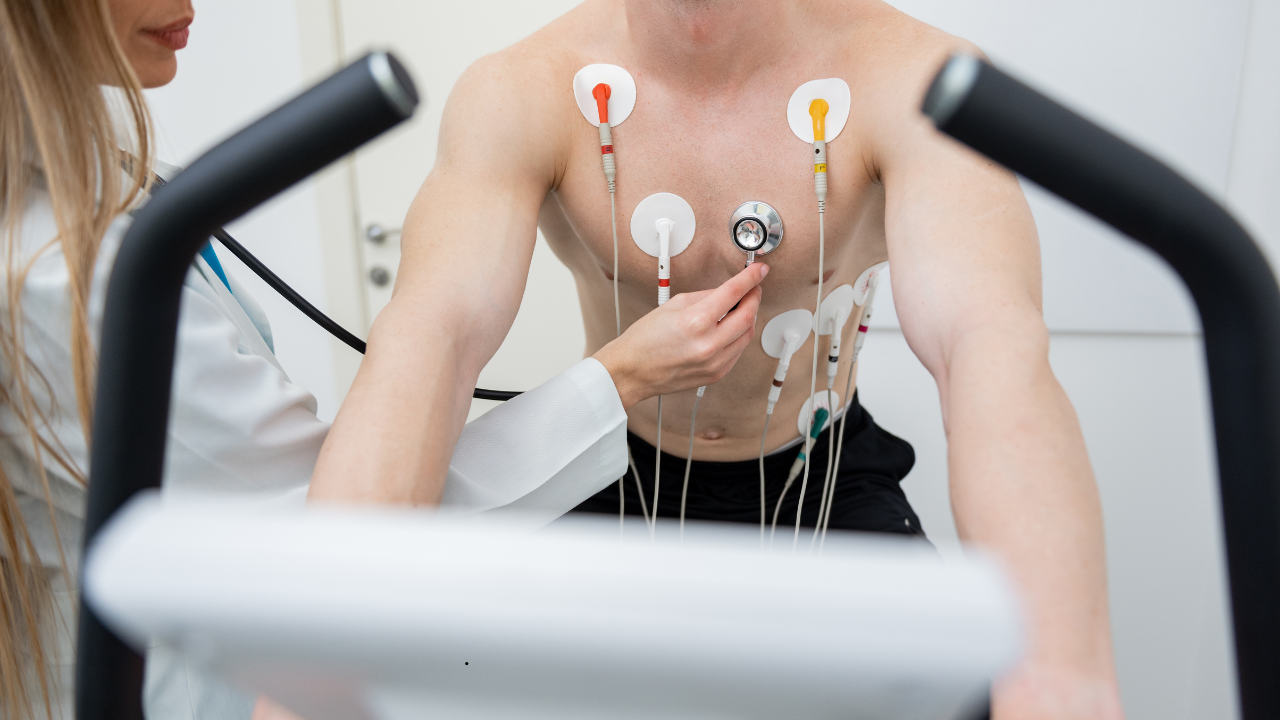
As per the National Institute of Health (NIH), US, it is a form of physical test that typically utilizes electrocardiography along with blood pressure monitoring and exercise, which involves a treadmill or bicycle.
However, in a resting stress test, the assessment happens when the heart muscle is at rest after stress. This stress helps in identifying areas of reduced blood flow like ischemia or damage to the heart muscle, which can indicate conditions like coronary artery disease.
The test involves injecting a radioactive tracer into the bloodstream, then using a special camera to take images of the heart at rest and after stress.
What Is A Bypass Surgery?
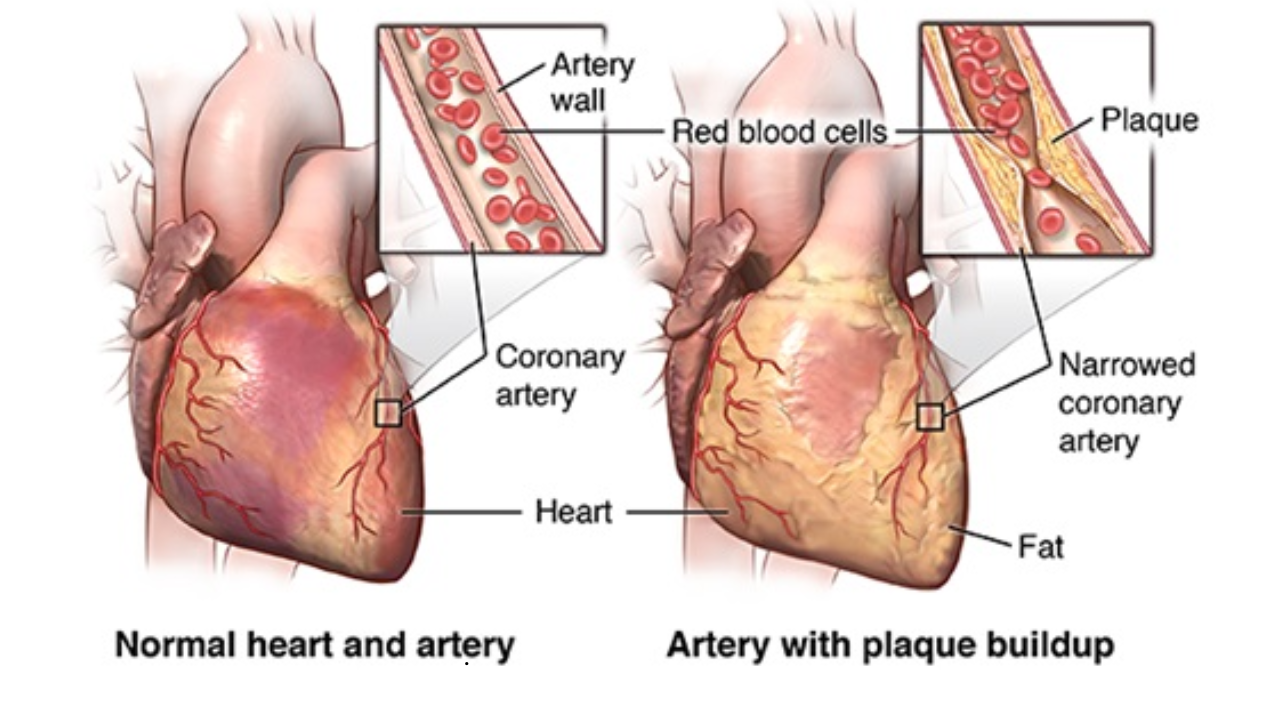
As per Johns Hopkins Medicine, bypass surgery or coronary artery bypass graft surgery (CABG) is a procedure used to treat coronary artery disease. Coronary artery disease (CAD) is the narrowing of the coronary arteries. These are the blood vessels that supply oxygen and nutrients to the heart muscle. CAD is caused by a build-up of fatty material within the walls of the arteries. This buildup narrows the inside of the arteries, limiting the supply of oxygen-rich blood to the heart muscle.
How Does It Work?
One way to treat the blocked or narrowed arteries is to bypass the blocked portion of the coronary artery with a piece of a healthy blood vessel from elsewhere in your body. Blood vessels, or grafts, used for the bypass procedure may be pieces of a vein from your leg or an artery in your chest. An artery from your wrist may also be used.
ALSO READ: 4 Rare Heart Diseases That Are Becoming Common By Each Passing Day
This surgery is done to treat a blockage or narrowing of one or more of the coronary arteries. It can restore the blood supply to your heart muscle when nonsurgical procedures are not a choice.
More Updates From The Swift Family
In addition to Scott, Taylor shared that her mom Andrea Swift, too, under a procedure. “My mom just got a new knee,” Taylor shared. “She’s doing great. She’s scampering around. We’re not quite at scampering yet, but she’s doing great.”
She noted that her parents are her best friends.
"It was actually one of the most special things that's ever happened to me, spending all that time with them this summer. You have those long talks that you don't have when it's a small, concentrated period of time.”
Delhi Hospital Gives New Life to 5-Day-Old Boy With Rare Brain Condition

In a rare medical miracle, a team of doctors in New Delhi successfully treated a five-day-old baby diagnosed with congenital hydrocephalus -- a rare neurological condition caused by the abnormal accumulation of Cerebrospinal fluid (CSF) in the brain.
While CSF acts as a shock absorber for the brain and spinal cord, as well as provides essential immunological protection, when in excess, it can increase pressure, cause tissue damage and turn fatal if untreated.
The baby boy, born to a family from Jewar in Uttar Pradesh, was born with an enlarged head that raised the potential for neurological damage.
However, as the doctors at HCMCT Manipal Hospital, Dwarka, had detected the condition during the last trimester of the pregnancy, they initiated the treatment soon after the baby was born.
“The biggest advantage was the early diagnosis during pregnancy, which allowed us to plan the surgery well in advance,” said Dr. Anurag Saxena, Cluster Head, Neurosurgery, at HCMCT Manipal Hospital.
How Did The Doctors Save His Life?
The 34-year-old expectant mother, also from Jewar in Uttar Pradesh, underwent a fetal MRI to help doctors assess the extent of the condition while she was still pregnant.
Once born, the baby boy underwent a surgical procedure that drained the excess fluid from his brain.
The highly delicate neurosurgical procedure involved the placement of a programmable ventriculoperitoneal (VP) shunt, which helped drain excess fluid from the brain and relieve intracranial pressure.
Explaining the intricacies involved in the surgery of newborns, Dr. Saxena said: "Performing neurosurgery in a newborn is always challenging due to the delicate anatomy, very low circulating blood volume, risks of hypothermia, and the complexities of anesthesia. However, timely intervention and a multidisciplinary team helped us achieve a positive outcome."
What is Congenital Hydrocephalus?
It is a rare condition present at birth, causing the head to enlarge due to excess fluid building up in the brain and increased pressure.It affects an estimated 2.2 to 18 per 10,000 live births globally. Its prevalence is much higher (up to 12.3 per 10,000) in low- and middle-income countries, particularly in Africa and Latin America.
In India, it has an estimated incidence of roughly 0.2-0.5 per 1,000 live births, though some studies suggest rates as high as 3-4 per 1,000 births. Boys are more susceptible to the condition than girls.
It can occur due to problems in brain development during pregnancy, genetic factors, or blocked fluid flow, which can further lead to serious brain damage if not treated in time. However, early diagnosis and treatment are key.
“Congenital hydrocephalus can cause serious and irreversible neurological damage. If left unaddressed, it can lead to severe brain injury, developmental delays, seizures, and may also turn life-threatening,” Dr. Saxena said.
“Following surgery, the baby showed a smooth and stable recovery in the NICU, with no post-operative complications. Early intervention not only ensured a successful surgical outcome but also significantly reduced the risk of long-term complications,” added Dr. Meenu Grewal, Consultant – Neonatologist at the HCMCT Manipal Hospital.
Andhra Pradesh Partners With Gates Foundation to Transform Healthcare System

Andhra Pradesh Health Minister Satya Kumar Yadav has announced a collaboration with the Gates Foundation to provide universal access to modern and affordable healthcare to its residents.
In alignment with Chief Minister Nara Chandrababu Naidu’s vision for ‘Healthy Andhra Pradesh', Yadav announced that the changes will make medical services more accessible and technologically advanced.
He also noted that the partnership will improve nutritional food security and public health outcomes, shift treatment planning from reactive to preventive and focus on a predictive healthcare approach. It also focuses on nutrition programs and digital medical services, moving beyond traditional treatment models.
Yadav further added that the government plans to introduce early disease detection systems, personalized health profiling, advance warning mechanisms for potential illnesses, individual health cards and expanded digital health services, including telemedicine.
The Health Minister assured residents that the State has created a high-power expert advisory group comprising of 10 international experts to review existing healthcare systems and recommend reforms, based on the Foundation's suggestion. Three sub-committees are also being formed to focus on specific areas, he added.
What Role Will AI Play In These Reforms?
In a February 15 statement, Yadav announced the launch of ‘MedTech Challenge’ to identify and demonstrate portable, affordable and scalable medical technologies using AI.“Around 100 applicants participated and, after two rounds of screening, 20 were shortlisted, he said. The shortlisted technologies are currently being tested in government hospitals under a pilot program and a final winner will be decided by the end of March.
Yadav explained that the program's focus areas included AI-based diagnostic tests, portable point-of-care testing centres, smart monitoring and wearable devices, telemedicine tools for remote areas and data integration and disease surveillance.
He said health data collected from various sources will be integrated with the RTGS “Aware” platform to enable early detection of disease outbreaks and data-driven policy formulation, which will help the state go-through with its planned reforms.
Andhra Pradesh Plans To Ban Social Media For Teenagers
The state also recently announced that it may soon follow Australia's steps and ban social media for teenagers under the age of 16 in the state.Nara Lokesh, Information Technology, Electronics and Communications, Real Time Governance and Human Resources Development Minister for Andhra Pradesh, told Bloomberg at the World Economic Forum 2026 Annual Meeting in Davos, Switzerland: "As a state, we are studying Australia’s under-16 law, and yes, I believe we need to create a strong legal enactment.
READ MORE:Living in High-Rises Linked to Higher Air Pollution Exposure, IIT Delhi Study Finds
"Youngsters below a certain age should not be on such platforms, as they do not fully understand the content they are exposed to. Thus, a strong legal framework may be required."
TDP national spokesperson Deepak Reddy supported Lokesh's claim and stated: "Children below a certain age are not emotionally mature enough to comprehend the negative and harmful content that is freely available online. That is why the Andhra government is studying global best practices and examining Australia's under-16 social media law."
If implemented successfully, Andhra Pradesh would be the first Indian state to issue the ban and could pave the way for other states to consider such policies. State officials are yet to clarify when the rule will be implemented and if any fines will be attached to it.
400K WHO-Trained Polio Workers Mobilized To Vaccinate 45 Million Children In Pakistan

Credits: WHO
One of the world's largest public health campaigns against polio has been launched for Pakistan, where around 400,000 World Health Organization or WHO-trained frontline workers have been mobilized to vaccinate 45 million children. This is the country's first nationwide polio campaign of 2026. This is in collaboration with Polio Eradication Initiative, these frontline workers are going door to door across cities and remote settlements, carrying oral drops that is the only protection against a virus which has no cure. Polio. It can even cause life long paralysis.
With over three decades of effort, polio cases in Pakistan reduced by 99.8 per cent, from roughly 20,000 cases in the early 1990s to 31 causes in 2025. The country along with Afghanistan, remains among the last places where wild poliovirus still circulates. This makes this campaign even more critical to global eradication of polio.
Read: Pakistan And Afghanistan Are The Only Countries Where Polio Remains An Endemic, Says WHO
Frontline Workers Reach The Remotest Of Settlements

“We climb mountains and walk through the snow for hours with great difficulty. There is also a risk of snow falling on us from the mountains. Yet we do not give up. We reach our assigned area to vaccinate all children and protect them from polio,” said Rabia, a vaccinator from Upper Chitral, quoted by the Polio Eradication Initiative.
During the February drive, Rabia trekked steep terrain to visit 146 households and vaccinate 85 children in remote areas.
In nearby Booni, another worker, Momina, described the work as both service and responsibility. “I thank Allah that I have gotten this opportunity to serve and I am trying my best to eradicate polio in my country,” she said, according to the initiative.
Zeenat, deployed in Khayaban-e-Sir Syed, spent long days navigating crowded neighbourhoods and climbing multiple floors to reach children inside apartment buildings. She covered 242 homes, administering oral vaccine drops to every eligible child.
“I am a mother too and I have also gotten my own children vaccinated for polio. Thank God, they are healthy and protected now,” she said in remarks shared by the Polio Eradication Initiative. “This disease has no cure. I want all parents in the country to vaccinate their children with polio drops so they don’t fall prey to paralysis.”
Health workers also marked children’s fingers after vaccination, a standard monitoring method to ensure no child is missed.
Two Drops, One Goal: Ending Polio
“The vaccine is very important for children in Pakistan because polio can infect children and paralyze them. This is why we go house-to-house to vaccinate them so that no child is paralyzed,” said Rawalpindi worker Neelum, as reported by the outlet.
Health authorities say the campaign reflects a simple but urgent public-health truth: eradication depends not just on vaccines, but on reaching every last child.
What Is Polio?
It is an illness caused by a virus that affects nerves in the spinal cord or brain stem. It can lead to a person being unable to move certain limbs, which can also lead to paralysis. Furthermore, it can also cause trouble breathing, and lead to death.
The polio virus is a naturally occurring virus that has been around since prehistoric times, as per the WHO. This disease can be found in humans and is spread through the faecal-oral route, which means it is transmitted when someone ingests food or water contaminated by human faeces.
Poliovirus is a small, single-stranded RNA virus that belongs to the Enterovirus subgroup of the Picornaviridae family and was first recognized as a distinct condition by English physician Michael Underwood in 1789. The virus was identified in 1909 by Austrian immunologist Karl Landsteiner.
About 5% of people with poliovirus get a mild version of the disease called abortive poliomyelitis. It has flu-like symptoms and can last for 2 to 3 days. The symptoms include:
Fever
Headache
Muscle Aches
Sore Throat
Stomachache
Loss of appetite
Nausea
Vomiting
A more severe form is the nonparalytic polio, affecting 1% of those infected which may have the symptoms such as:
Neck pain or stiffness
Aches or stiffness in arms or legs
Severe headache
The most serious form is paralytic polio, while the symptoms start with those of nonparalytic polio and can progress to more severe signs including:
Intense pain
Extreme sensitivity to touch
Tingling or pricking sensations
Muscles spasms or twitching
Muscle weakness progressing to a limp paralysis
© 2024 Bennett, Coleman & Company Limited

