- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Stranger Things Star Millie Bobby Brown Lives With Unilateral Deafness: Here’s What The Condition Means

Credits: Canva/AP
Millie Bobby Brown has built an impressive career, all while quietly managing a few health concerns along the way. From becoming a household name through Netflix’s hugely popular Stranger Things to leading films like Enola Holmes, the Gen Z actor (now a married mother of one) has made a strong mark in Hollywood. What many people may not realise is that her work has, at times, been shaped by a hearing-related condition. Brown has lived with hearing loss for most of her life, a fact that often goes unnoticed.
Millie Bobby Brown Reveals Having Unilateral Deafness
Brown first spoke publicly about her hearing condition in a 2017 interview with Variety, where she shared that she has had hearing loss in one ear since birth. Even early in her career, she was clear that she would not allow it to stand in the way of her passion for performing. “I just started to sing, and if I sound bad I don’t care, because I’m just doing what I love,” she said at the time. “You don’t have to be good at singing. You don’t have to be good at dancing or acting. If you enjoy it and it makes you happy, you should do it.”
While Brown rarely focuses on her hearing loss, she has spoken about how it affects her daily life. In a conversation with Call Her Daddy host Alex Cooper, she explained that certain sounds, like loud chewing, do not bother her because she can mostly hear herself when she eats. She also shared that her husband, Jake Bongiovi, whom she married in 2022, sometimes jokes that she has “selective hearing.” In reality, she says sounds often feel “muffled, like being underwater.” Brown admitted that she does miss important moments, including hearing directors call out “action” or “cut” on set.
What Is Unilateral Deafness?
Unilateral hearing loss happens when hearing is affected in one ear while the other ear functions normally. Even with hearing in one ear, this condition can make it difficult to understand speech clearly and to identify where sounds are coming from.
The level of hearing loss in one ear can range from mild to severe. When there is little to no hearing at all in one ear, it is described as severe or profound hearing loss, also known as single-sided deafness. Unilateral hearing loss may be present at birth, develop gradually, or appear suddenly. Depending on the cause, options such as hearing aids or cochlear implants may help improve hearing, according to the Cleveland Clinic.
Unilateral Deafness: What Are The Symptoms?
Many symptoms of unilateral hearing loss are similar to those seen with hearing loss in both ears. You may:
- Ask people to repeat what they’ve said
- Increase the volume on your television, laptop, or phone
- Struggle to follow conversations, especially in noisy places like restaurants or busy workplaces
- If hearing is affected in only one ear, tinnitus, or ringing, may occur on that side alone. You may also notice that you tend to rely more on one ear when speaking on the phone or listening to others.
- Although unilateral hearing loss often develops slowly, it can also happen suddenly. If you experience a sudden loss of hearing in one ear, it’s important to seek medical advice promptly.
What Causes Unilateral Hearing Loss?
Doctors do not yet fully understand all the reasons why hearing loss occurs in just one ear. Causes can differ between adults and children. In children, hearing loss may be linked to genetics or infections. Possible causes include:
- Noise-related hearing damage
- Certain inherited conditions, such as neurofibromatosis Type 2, which can lead to acoustic neuromas in one ear
- Head injuries
- Traumatic brain injury (TBI)
Unilateral Hearing Loss: Is There Treatment Available?
According to the American Academy of Audiology, treatment depends on the underlying cause and the severity of the hearing loss. Available options may include:
- Hearing aids: These are typically worn to support sound perception when one ear is affected
- Contralateral routing of signal (CROS) devices: This setup uses two devices. One acts as a microphone on the non-hearing side and sends sound to a hearing aid worn on the functioning ear
- Cochlear implants: These may help restore hearing in the affected ear and improve speech understanding and sound awareness
- Bone-anchored hearing aids: These devices transmit sound from the non-hearing ear to the hearing ear through bone conduction
- Frequency modulation (FM) systems: FM systems use radio signals to send sound directly from a microphone to a receiver, such as a hearing aid worn on the non-hearing ear
Can Alzheimer’s Disease Be Reversed? Here’s What the New Research Shows

Credits: Canva
In what researchers are calling an important scientific advance, a team in the US has shown through animal experiments that Alzheimer’s disease may be reversible, overturning a belief that has shaped medical thinking for more than 100 years. For generations, the neurodegenerative condition was considered permanent and progressive. The findings, published in Cell Reports Medicine, are based on multiple preclinical mouse models as well as examinations of human Alzheimer’s brain tissue.
The study found that preserving a healthy balance of NAD, a molecule central to cellular energy production, could both prevent and reverse Alzheimer’s-related damage. NAD plays a key role in brain function and is now seen as a major contributor to the disease process. Researchers also observed that NAD levels drop much more sharply in the brains of people with Alzheimer’s, a pattern that was mirrored in mouse models of the condition.
Don't Miss: Taking Tramadol? Scientists Warn It May Cause More Harm Than Relief
Alzheimer’s Disease Can Be Reversed, New Study Shows
“We were extremely encouraged by what we observed,” said Andrew A. Pieper, the study’s senior author and Director of the Brain Health Medicines Center at the Harrington Discovery Institute, University Hospitals, as per Sciencedirect. “By restoring the brain’s energy balance, we saw both structural and functional recovery in mice with advanced Alzheimer’s.”
Pieper noted that the effect appeared consistently across two very different mouse models, each driven by separate genetic mechanisms linked to Alzheimer’s in humans. “Seeing recovery in models caused by distinct genetic pathways strengthens the case that restoring NAD balance in the brain could have real therapeutic potential for patients,” he said.
For the study, researchers examined mice engineered to carry genetic mutations known to cause Alzheimer’s disease in people. One group of mice carried multiple human mutations affecting amyloid processing, while the second group carried a human mutation in the tau protein.
After confirming that brain NAD levels dropped sharply in both human Alzheimer’s tissue and mouse models, the team tested whether stopping this decline before symptoms appeared could prevent disease, and whether restoring NAD levels after the disease had progressed could reverse it. To do this, they used a well-studied drug called P7C3-A20 to restore NAD balance in the brain.
The results were striking. Not only did maintaining NAD levels prevent Alzheimer’s from developing in mice, but starting treatment later, after the disease was already advanced, allowed the brain to repair the main pathological damage caused by the genetic mutations. In both mouse models, cognitive abilities were fully restored.
What Is NAD In Alzheimer’s?
In Alzheimer’s disease, NAD, short for nicotinamide adenine dinucleotide, is an essential coenzyme whose levels naturally decline with age. This decline disrupts energy production, mitochondrial health, DNA repair, and the ability of neurons to withstand stress. Research suggests that increasing NAD levels, often through precursors such as nicotinamide riboside, may reverse Alzheimer’s-related damage, improve memory, and correct abnormal RNA processing in animal models. Because of this, NAD has become a major area of focus for developing new Alzheimer’s therapies, according to the National Institutes of Health.
Why NAD Is Important In Alzheimer’s
- Energy and Mitochondria: NAD is necessary for producing ATP, the cell’s main energy source, and for keeping mitochondria functioning properly, both of which are critical for healthy brain cells.
- Cellular Stress: NAD supports neurons in responding to and surviving stress. When NAD levels fall in Alzheimer’s, these protective mechanisms weaken.
- DNA Repair: NAD is involved in repairing DNA damage, which increases as amyloid-beta accumulates in the brain. Low NAD levels interfere with this repair process.
- RNA Splicing: Emerging research shows that NAD may help correct faulty RNA splicing events linked to Alzheimer’s. This process may involve a protein called EVA1C and could contribute to improved memory and better clearance of harmful proteins.
Next Steps Toward Human Trials
The findings also pave the way for further research and eventual testing in people. The technology behind the treatment is currently being developed for commercial use by Glengary Brain Health, a Cleveland-based company co-founded by Dr. Pieper.
“This recovery-based treatment approach now needs to be tested in carefully designed clinical trials to see if the benefits seen in animals can be replicated in humans,” Pieper said.
He added that future laboratory work will focus on identifying which components of brain energy balance matter most for recovery, exploring additional strategies that could complement this approach, and determining whether similar methods could work for other long-term, age-related neurodegenerative diseases as well.
Adenovirus Cases Rise In UK, Health Authorities On Alert

Credits: Canva
Adenovirus, or what some people are calling the mystery disease is going to be the next worry in the UK, after superflu had already grappled the healthcare system. Along with H3N2 and its variant superclade K, people are now worrying about this mystery disease.
Adenovirus is highly contagious and causes mild cold or flu-like symptoms, though severe cases could lead to stomach flu and vomiting. Many describe this virus as 'heartier' than others. The reason is that the virus can survive longer on surfaces and even resist the common disinfectants used. This is what makes it highly transmissible.
Is There Any Treatment For Adenovirus?
As of now, there is no treatment for adenovirus, it could however be managed and monitored. What helps is regular handwashing and thorough cleaning of surfaces.
The good news is that cases of adenovirus are actually dropping in the UK, as confirmed lab reports. The cases last week were 1.2 per cent, whereas the week prior, it was at 1.7 per cent, as also reported by the Independent.
What Are The Symptoms Of Adenovirus?
While a lot of the symptoms mimics of those in flu or COVID, including shortness of breath, a sore throat and or a runny nose. However, there are certain unique symptoms of adenovirus that include:
- Diarrhea
- Pink Eye or conjunctivitis
- Ear infection or otitis media
- Swollen lymph nodes
- Pneumonia
- Stomach pain
- Nausea
- Vomiting
Other rare symptoms could also include impact on your bladder or nervous system. As viruses in your bladder can also cause urinary tract infections, and the same virus in your nervous system can cause condition that can affect your brain. These conditions also include encephalitis and meningitis.
The symptoms usually start to subside within two days, however, if the symptoms stay even after three days without any relief, it might be a red flag. The best thing to do during such a situation is to go consult your GP.
Also Read: Unique Symptoms Of Mysterious Adenovirus And How Long Infection Now Last
Is Adenovirus Spreading Faster Than Flu and Covid?
Experts have noted that due to its ability to stay longer in the environment and being highly transmissible, it is in fact, spreading faster than flu and COVID. Eric Sachinwalla, Jefferson Health's medical director said that this virus is still unfamiliar and thus not much can actually be done to treat adenovirus. Speaking to PhillyMad, he said, "It is pretty contagious because it is heartier than other viruses - soap and water, or everyday disinfectant, won't kill it, so it tends to live in the environment longer."
What Are The Ways To Stay Safe From Adenovirus?
Since adenovirus spreads through close contact and is resistant to many everyday disinfectants, hygiene remains the key. The best way to stay safe is by avoiding close contact, especially with those who are unwell. You may also keep an eye on your symptoms, including your body temperature and take steps to prevent the virus from spreading by taking precautions, as well as getting the flu jab.
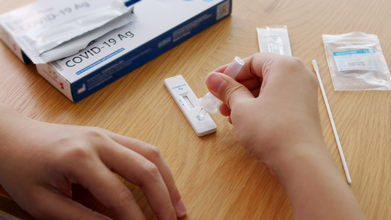
WHO Approves Two COVID-19 Rapid Antigen Tests, Check The Details Here
Credits: iStock
The World Health Organization (WHO) on December 24 prequalified two rapid antigen diagnostic tests (Ag-RDTs) for SARS-CoV-2. This virus is known to have caused COVID-19. As per the WHO, these two tests are called SD Biosensor STANDARD Q COVID-19 Ag Test and the ACON Biotech Flowflex SARS-CoV-2 Antigen Rapid Test (Self-Testing).
At first these tests got temporary emergency approval from the WHO during the pandemic. This was done so the countries could start using them quickly even though long-term data was limited. This emergency approval helped the tests reach over 100 countries when they were urgently needed.
What Has Changed Now?
The WHO has now given these tests full prequalification, which means it has a stronger and long-term approval. This means that the WHO has thoroughly checked and confirmed that the tests consistently meet global standards for quality, safety, and accuracy.
Why Does This Matter?
- The tests can now be officially bought and used by global organizations and governments
- They can be included in bulk purchasing to lower prices and increase supply
- This makes reliable COVID-19 testing more affordable and accessible, especially in low-and middle-income countries
COVID-19 Is Far From Being Over
Even though WHO officially ended COVID-19 emergency phase over two years ago, the virus is still circulating globally. In fact, this year, we have seen variants of COVID-19 circulating around, causing the most unique symptoms, including razor-blade like throat. Variants like JN.1, Stratus, Nimbus, LP8.1, and BA.3.2 were all that we saw in 2025.
While the good news is that infection levels are relatively stable, but the virus has not completely disappeared and testing is still necessary, especially in poorer countries.
Many low-income countries do not have easy access to labs or expensive PCR testing. So there is still a need for a strong, but cheaper and reliable way to detect COVID-19, and these tests may as well do that.
Why Rapid Antigen Test Matters
- Give results in 15–30 minutes
- Cost less than PCR tests
- Don’t require labs or specialized equipment
- This means they can be used in small clinics, community centers, mobile vans, or remote areas, where lab testing isn’t practical.
However, it is important to note that rapid antigen tests are not replacement for PCR tests. They simply complement the PCR tests by allowing faster, on-the-spot decisions, especially when the lab capacity is limited.
What Makes It Essential Today?
Rapid antigen tests could help with spotting and stopping local outbreaks quickly, protecting high-risk people and healthcare workers, and staying prepared for future respiratory pandemics.
The WHO is also pushing for decentralized, quality-checked testing as part of universal healthcare and global health security, so countries aren’t caught unprepared when the next outbreak happens.
When Is It A Right Time To Get Yourself Checked For COVID-19?
If you notice these following symptoms as noted by the Centers for Disease Control and Prevention (CDC), it is best that you get yourself a COVID-19 test:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Sore throat
- Congestion or runny nose
- New loss of taste or smell
- Fatigue
- Muscle or body aches
© 2024 Bennett, Coleman & Company Limited

