- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories

Study links bottled water to high BP (Image: FreePik)
Study Links Drinking from Plastic Bottles to Increased Blood Pressure
Microplastics, found in plastic bags, storage containers, and bottle caps, are perilous to health. Previously, they have been linked to heart issues, hormone imbalances, and even cancer, but now a study has connected it to blood pressure. The study, conducted by the Department of Medicine at Danube Private University in Austria, found that drinking from plastic bottles may increase blood pressure due to microplastics entering the bloodstream.
For the study, researchers provided a group of participants with fluids not stored in plastic bottles and observed a notable decrease in their blood pressure. "Remarkable trends were observed. The results of the study suggest, for the first time, that a reduction in plastic use could potentially lower blood pressure, probably due to the reduced volume of plastic particles in the bloodstream," the research team wrote. "Based on the findings, indicating a reduction in blood pressure with decreased plastic consumption, we hypothesize that plastic particles present in the bloodstream might contribute to elevated blood pressure," they said.
The study concluded with a recommendation to avoid beverages, including water, packaged in plastic bottles. A few years ago, scientists found that humans ingest about 5 grams of microplastics weekly through fluids in plastic bottles. This amount of microplastic is equivalent to a credit card.
Here's how you can prevent microplastics from entering your bloodstream
To prevent microplastics from entering the body, the scientists suggested boiling and filtering tap water. They said that these methods can reduce the presence of microplastics and nanoplastics by nearly 90%. Talking about blood pressure, they admitted that factors like gender differences in heart function and the possible impact of lower phthalate exposure weren't included in the study, but they should be looked into further.
Know more about microplastics
Microplastics are tiny plastic particles, less than 5 millimetres in size, that result from the breakdown of larger plastic waste. These particles are pervasive in the environment, found in oceans, rivers, and soil, contaminating ecosystems worldwide. Microplastics are not only polluting our planet but are also entering our food and water supply, posing significant health risks.These particles have been linked to various health issues, including heart problems, hormone imbalances, and even cancer. Microplastics can disrupt ecosystems by affecting marine life and contaminating food chains, leading to broader environmental impacts.

Credits: Canva
Maternal Mortality On Rise In US, Reports CDC
After two years of decline in maternal mortality, especially in the number of women dying during or shortly after childbirth in the US, the numbers are again on the rise. As per the newly released data from the Centers for Disease Control and Prevention (CDC), the 2024 figures have renewed concerns about maternal health in the country. US has already been at one of the highest maternal mortality rates among the high-income countries.
The CDC's provisional report stated that 688 women died last year due to pregnancy-related complications. This is a slight increase from the 669 deaths reported in 2023. The maternal mortality rate also rose and reached to 19 deaths per 100,000 live births. This is up from 18.6, the rate recorded a year earlier.
While the numbers do remain below the peak figures which was noted in the COVID-19 pandemic in 2021 and 2022, the reversal of a two-year downward trend has raised alarms.
What Are Maternal Deaths?
As per CDC, maternal deaths occur during pregnancy, childbirth, or within 42 days after delivery. The major point here is that the deaths must occur due to pregnancy-related conditions. These include excessive bleeding, infections, and blood vessel blockages, which continue to be among the leading causes.
The COVID-19 Effect
The numbers of maternal deaths in the US surged during the COVID-19 pandemic. This proved to be dangerous for pregnancy women, since many healthcare systems and hospitals have become overwhelmed. It also led to gaps in care. During the worst phases of pandemic, some physicians also reported burnout. This could have also been the reason why pregnancy related concerns which required immediate attention could have been downplayed.
As the pandemic receded in 2022 and 2023, the number of maternal deaths declined, in part because of improved COVID-19 prevention and treatment protocols. However, experts warn that the progress made during those years is now being undermined by new and persistent challenges.
The Reason Behind These Numbers:
As per the public health experts, there are several factors that have lead to an increase in the number of maternal mortality:
Limited Access to Care: The closure of rural hospitals across the U.S. continues to make it harder for women in remote areas to access prenatal and emergency care.
Legal and Regulatory Changes: The 2022 Supreme Court ruling that overturned Roe v. Wade has had a ripple effect on maternal healthcare. Some doctors, concerned about legal consequences, are reportedly hesitant to provide certain treatments during pregnancy-related emergencies. In states with strict abortion laws, this has translated into delays in care — potentially putting mothers at greater risk.
Worsening Inequities: The U.S. has long-standing racial disparities in maternal health outcomes. Research has consistently shown that Black women die from pregnancy-related complications at much higher rates than white women, due to a combination of systemic racism, limited access to quality care, and implicit bias in medical settings.
The major concern is also that among the many wealthy countries, US has continued to stand out in a way that is not good for it. It has one of the highest maternal mortality rates in the developed world.
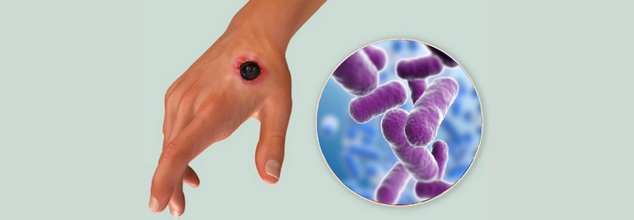
Thailand Confirms First Anthrax Death In 30 Years Raises Alarm Over Potential Spread
Thailand's health officials reported on Wednesday the first human anthrax death since 1994, a tragic first in the northeastern province of Mukdahan. A 53-year-old man who had slaughtered and eaten raw beef developed cutaneous lesions and systemic symptoms before dying from infection despite being treated. Another case was confirmed in a friend with the same exposure, and three more suspected cases are being investigated. This unusual death has triggered an emergency public health response from several government agencies.
Anthrax is caused by the spore‑forming bacterium Bacillus anthracis, which mainly infects grazing livestock and wildlife. Humans become infected by direct contact with infected animals, contaminated animal products, or by eating undercooked meat. There are three clinical forms:
Cutaneous anthrax, the most prevalent, develops from itchy papules, which become black eschars, and is usually lethal if untreated.
Gastrointestinal anthrax, caused by the ingestion of tainted meat, causes acute pain in the abdominal area, nausea, and hemorrhagic diarrhea.
Inhalational anthrax—isolated, yet fatal—is produced when the spores are breathed in and manifest as respiratory insufficiency and systemic shock.
Unlike most infectious diseases, anthrax is not transmitted person-to-person. Early antibiotic treatment is effective, but delay in diagnosis can permit the bacteria to spread and cause life-threatening illness.
All About the Mukdahan Outbreak
The epidemic hub was in Don Tan district, Mukdahan Province, literally on the other side of the Mekong River from Laos, where 129 cases of anthrax (one fatal) were reported during the last year. Thai authorities have tracked down 638 people possibly exposed via butchering or eating raw beef: 36 butchers and 602 consumers are now being closely monitored and administered prophylactic antibiotics
Dr. Weerawat Manosuthi, Thailand's Disease Control Department spokesman, reported, "All those who are suspected to have come into contact with contaminated meat are under observation," emphasizing the need for expedient containment measures to avoid further infections.
Following the death and second confirmed case, Thailand's Agriculture Ministry has declared a 5‑kilometer cordon of quarantine around the animal exposure site. In this cordon, 1,222 cattle will be vaccinated by the Livestock Department, although none have as yet shown signs of disease or unexplained death
In the meantime, all suspected human contacts are on a course of ciprofloxacin or doxycycline, under close observation for the first symptoms of the disease. Clinics have been set up to identify anthrax signs, including painless ulcers on the skin and swollen lymph nodes, and to provide quick diagnostic tests, such as PCR assays.
Anthrax is also endemic in Southeast Asia, and border states have recently struggled with outbreaks as well. Laos's outbreak in 2024 and Vietnam's 13 cases reported in May 2023 underscore the impermeable nature of zoonotic disease transmission across the region. Thai health officials are meeting with their colleagues in Laos, Cambodia, and Vietnam to exchange information and coordinate surveillance efforts along borders.
Dr. Narong Chankaeo, head of the Mukdahan provincial health department, cautioned that environmental conditions—like flooding which exposes spores to the surface—could cause future outbreaks. "Increased surveillance in border towns and among cattle handlers is a must," he said.
Why Anthrax Reemerges?
In Mukdahan, the eating of raw beef dishes is a cultural norm that adds to risk. Flooding during certain seasons can disrupt spores hidden beneath the soil, infecting pastures and water sources. Added to unregulated butchering practices—frequently without protective equipment—these create a perfect storm for the reemergence of anthrax.
Experts also point out that years without a fatal case could have bred complacency both among the public and veterinarians. Dr. Saneemongkol Sawettanan, an epidemiologist at Bangkok's Ministry of Public Health, added, "We need to retrain rural health workers and farmers of livestock about anthrax prevention—lapses in awareness can be fatal."
From Rapid Response to Long‑Term Prevention
Although Thailand's rapid quarantine and vaccination campaign are essential initial actions, long‑term prevention involves a One Health strategy—aligning human, animal, and environmental health initiatives. These are:
- Routine cattle vaccination in areas of high risk
- Public awareness on proper meat handling
- Surveillance of anthrax spores in water and soil
- Exchange of data across borders and joint simulation of outbreaks
Through an improvement in veterinary services and public health infrastructure, Thailand can decrease the chances of future deaths.
Thailand’s first anthrax death in three decades is a stark reminder that even well‑known pathogens can re‑ignite under conducive conditions. As global travel and trade resume post-pandemic, zoonotic threats remain ever‑present. The Mukdahan outbreak underscores the importance of:
- Maintaining robust vaccination programs for livestock
- Ensuring rapid diagnostic capacity at local clinics
- Fostering regional collaboration on disease surveillance
- Balancing cultural practices with food safety education
What is Anthrax?
Anthrax is an uncommon but sometimes life-threatening illness caused by the spore-forming bacterium Bacillus anthracis that is naturally distributed in soil. Although it only infects animals and wild animals, humans are at risk when they have direct or indirect exposure to infected animals or contaminated animal products.
Unlike most contagious diseases, anthrax is not directly spread from human to human. Yet, skin sores from anthrax do carry a slight risk if a person touches them or contaminated objects (fomites) directly. The majority of human infections happen when bacterial spores gain entry into the body through cuts in the skin, eating undercooked contaminated meat, or through inhaling airborne spores.
Symptoms to Know
There are four major forms of anthrax infection, each having different symptoms. Incubation usually lasts between one to six days, but inhalation anthrax can take weeks to appear.
Cutaneous Anthrax (Skin-Related)
This is the most frequent and least deadly form of anthrax. It happens when the bacteria get into the body through a cut or scratch on the skin. If medical treatment is sought soon enough, cutaneous anthrax seldom develops life-threatening complications.
Common signs and symptoms are:
- A small, itching bump that looks like an insect bite and soon develops into a painless ulcer with a black center
- Swelling around the infected sore
- Swollen lymph nodes near the infection site
- At times, flu-like signs and symptoms like fever or headache
When Should You Seek Medical Attention?
Since initial anthrax symptoms may be similar to those of run-of-the-mill viral infections—such as the flu—it's simple to miss the early warning signs. But if you suspect exposure, particularly in a work environment where contact with infected animals or animal by-products may occur, immediate medical assessment is paramount.
Consult a doctor immediately if you experience strange skin lesions, fever, or respiratory disease following exposure in areas where anthrax infection is known to exist. Early treatment with antibiotics can make a big difference.

Credits: Canva
CDC Reports 216 Child Deaths From Flu This Season, The Worst Since Swine Flu Outbreak
The Centers for Disease Control and Prevention (CDC) has officially reported the largest number of pediatric deaths in more than 15 years, topping even last year's death count and paralleling the killing impact of the 2009-2010 swine flu pandemic. At least 216 U.S. children have lost their lives from influenza-related causes through the current 2023–2024 flu season as of early May, a count that experts cautioned will likely still grow as further data are accumulated.
Dr. Sean O'Leary, a pediatric infectious disease physician at the University of Colorado and a spokesperson for the American Academy of Pediatrics, noted that the reported death toll is probably an underestimation. "This number that we have now is almost certainly an undercount," he said in an interview with the Associated Press, adding that final counts from CDC flu data are usually revised and finalized during the fall.
One of the most disturbing factors contributing to the surge in child flu deaths is the dramatic decline in rates of flu vaccination among children. The vaccination rate has plummeted from 64% five years ago to only 49% this flu season, reports Dr. O'Leary. The seriousness of the decline cannot be overstated—particularly with the fact that flu vaccines, though they cannot always prevent illness, are shown to significantly reduce the risk of hospitalization and death.
The information indicates that a majority of the deaths were preventable. The number of children who received vaccinations among the 216 that passed away was not released by the CDC, nor did they provide expert insight within the report. Nevertheless, it is hard to ignore the trend between declining flu vaccine usage and higher mortality.
Adults were not exempt from this year's flu season either. The CDC estimates that this season's flu has sickened at least 47 million people, hospitalized 610,000, and killed 26,000 in all ages up to this point. In adults who were hospitalized with flu, 95% had one or more underlying conditions, including diabetes or heart disease. But the scenario is very different among children: only around 53% of the nearly 2,000 hospitalized children researchers examined had an underlying condition, including asthma or obesity. This means many of the sickened children were otherwise well.
These kinds of statistics confirm the capricious and sometimes indiscriminate nature of the flu virus—especially in years when several aggressive strains are in circulation at the same time.
Why This Year Was Particularly Challenging?
The season of 2023–2024 has been peculiar when it comes to virology. Rather than a single prevalent strain, two distinct Type A strains—H1N1 and H3N2—have been spreading extensively, making it even more complex in terms of diagnosis, treatment, and prevention. Fortunately, the flu vaccine has been working fairly well, based on previous CDC information that indicated that it was efficient in cutting down hospitalizations and deaths.
Nevertheless, a large number of Americans did not get vaccinated or got vaccinated too late. Misinformation, logistical challenges, and decreased access to pediatric vaccination services have all contributed.
The healthcare infrastructure also has a part in these results. As Dr. O'Leary noted, pediatrician clinics nationwide are running short on staff and are seeing fewer after-hours clinics, which makes it harder for families to get their children vaccinated. Although pharmacies have become the default choice for many adults who are seeking vaccines, they are not all equipped—or even permitted by law—to vaccinate children.
This access structural gap is an increasingly pressing concern, particularly as more Americans are turning to retail healthcare environments for routine vaccinations.
Why is Vaccine Hesitancy and Political Rhetoric a Dangerous Mix?
Superimposed over this entire crisis is a general collapse in childhood vaccination rates across the board—led in part by a steady stream of misinformation online and amplified by political leaders. Robert F. Kennedy Jr., now the U.S. Secretary of Health and Human Services, publicly sided with vaccine-critical language, which restarted debates that swept up speed during the COVID-19 pandemic. His divisive stance is thought to have impacted public trust and potentially led to a general collapse in vaccine confidence.
Experts fear that this politicization of public health measures may be eroding decades of effort in infectious disease prevention.
Flu Activity Now in Decline
There is some relief: the CDC says flu activity is now declining, with all 50 states reporting low or minimal levels. But for the families of the 216 children who died this season, it comes too late.
Public health officials continue to strongly recommend annual flu vaccinations for everybody six months and older, warning Americans not to get complacent. "My hope is that this season will be a little bit of a wake-up call," said Dr. O'Leary. "We actually do need to vaccinate our kids against influenza."
The increase in pediatric flu fatalities in the 2023-24 season is a failure of public health with several contributing layers—vaccine hesitancy, systemic gaps in healthcare, and politicization of science. And yet, it's also an moment of clarity. Influenza is a serious, occasionally fatal virus, and vaccines are among our most effective weapons in limiting its spread.
As flu season comes to a close, the call to action is clear: heightened awareness, greater vaccine availability, and a collective effort to restore trust in public health must be top priorities to avoid another tragic year.
© 2024 Bennett, Coleman & Company Limited

