- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Virologist And A COVID-19 Vaccine Critic, Steven Hatfill, Asked to Resign From US Health And Human Services
Credits: Reuters
Virologist Steven J Hatfill, long known for his controversial views on COVID-19 vaccines and treatments has now been asked to resign from his role as Chief Medical Officer at the US Department of Health and Human Services' (HHS) Administration for Strategic Preparedness ad Response (ASPR).
He was a vocal critic of the mRNA vaccines and proponent of hydroxychloroquine as the treatment for COVID-19. He has now been asked to step down, this has come in less than six months of him joining the agency,
Resignation Request From Senior Officials
According to Hatfill, the request for his resignation came directly from Matt Buckham, Chief of Staff at ASPR, who informed him that Health Secretary Robert F. Kennedy Jr. had personally asked for his removal.
“He stated that they were taking ASPR in a different direction,” Hatfill said in a written statement released Sunday. “I refused to resign and asked to speak to the Secretary directly. It appears that the Secretary is being sequestered, and HHS is in a free fall.”
While Hatfill maintains he has not yet been formally terminated, an administration official speaking anonymously described his removal as “for cause,” indicating that the decision had already been finalized internally, as reported by Bloomberg.
Was There A Dispute Over Vaccine Policy and Public Messaging?
Hatfill’s departure follows growing internal tensions over the administration’s recent decision to terminate nearly two dozen mRNA-related vaccine projects valued at around $500 million.
The decision, supported by a 181-page report that Hatfill helped compile, argued that mRNA-based vaccines “fail to protect effectively against upper respiratory infections like COVID and flu.” The claim echoed statements made earlier this year by Secretary Kennedy, who has long questioned the efficacy and safety of certain vaccines.
However, health experts and multiple peer-reviewed studies have repeatedly found that COVID-19 vaccines significantly reduce the risk of severe illness, hospitalization, and death — even if they do not always prevent mild infections.
Controversial Statements Hatfill Has Made
Shortly after contributing to the vaccine report, Hatfill appeared on Stephen K. Bannon’s War Room podcast, where he made several alarming claims about vaccine safety.
“It was more dangerous to take a vaccine than it was to contract COVID-19 and be hospitalized with it,” he said during the interview. He further alleged, without evidence, that “the vaccines have injured hundreds of thousands” and that an unknown number of people had died from vaccination.
These remarks drew widespread criticism from the scientific community, with experts reiterating that vaccine safety is continuously monitored through established federal systems and that serious adverse effects remain exceedingly rare.
Before joining HHS, Hatfill served as a White House adviser during President Donald Trump’s administration, where he promoted hydroxychloroquine as a potential COVID-19 treatment — a claim that was later discredited and led U.S. regulators to revoke its emergency authorization in 2020.
Hatfill also gained notoriety in the early 2000s when he was named a “person of interest” in the FBI’s investigation into the 2001 anthrax attacks that killed five people and sickened 17 others. He was formally cleared of any wrongdoing in 2008, and the government paid him $4.6 million to settle a lawsuit related to the case.
Coronavirus-Like Virus Discovered in South American Bats, Researchers Say

Credits: Canva
COVID-19, a pandemic that shook the world, and its variant, still continues to be around, especially the new 'Frankenstein' strain, that is said to be the contagious of all. However, the answer to what really was the source of the virus has not been found. Though there are certain theories that associate bats with it. While researchers have time and again said that more research is needed in this. A coronavirus carrying a genetic feature was found in the viruses that cause COVID-19 and MERS. This has been discovered in bats in Brazil. This may put some light back into the global range of bat-borne viruses that are capable of jumping to other species.
What Is The Virus Called?
The virus is called the BRZ batCoV. It was detected in Pteronotus parnellii, a small insect-eating 'mustached' bat, which is common across Latin America, The samples were collected in the states of Maranhao and Sao Paulo and the findings were released in a study as a preprint ahead of peer review publication. The study can be accessed at bioRXiv, and is titled: A Divergent Betacoronavirus With A Functional Furin Cleavage Site In South American Bats.
What Did The study Find?
The study, released Monday as a preprint pending peer review and publication, identifies the virus as part of the betacoronavirus family, the same group that includes SARS-CoV-2, MERS-CoV, and the original SARS virus. Genetic sequencing revealed a small segment of the virus’s spike protein that can be cleaved by enzymes in both animal and human cells, a trait that allows certain coronaviruses to infect cells more efficiently.
Interestingly, such furin cleavage sites have not been observed before in bat coronaviruses from the Americas, suggesting that these features may have evolved independently within South American bat populations.
The discovery is significant because a similar cleavage site in SARS-CoV-2’s spike protein sparked widespread debate during the pandemic, with some alleging it was evidence of laboratory engineering. However, subsequent research has demonstrated that comparable sites occur naturally in several coronaviruses, including this newly identified Brazilian strain, underscoring that such adaptations can emerge through normal viral evolution.
The new study is led by scientists from the University of Osaka. They had identified a previously unknown coronavirus in bats from South America, the first of its kind detected in the Western Hemisphere. The research, conducted by Kosuke Takada and Tokiko Watanabe in collaboration with teams from the University of São Paulo, the University of Wisconsin–Madison, and several international laboratories, found that the virus is related to MERS-like coronaviruses but distinct enough to form its own lineage.
Until now, similar viruses have only been found in bats across Asia, Africa, and the Middle East. The discovery marks a major step in understanding the global diversity and evolution of coronaviruses, particularly those circulating among wildlife.
Importantly, researchers emphasize there is no evidence that the newly detected virus infects humans. However, they note that such discoveries highlight the urgent need for continued monitoring of animal populations that could harbor viruses capable of crossing into humans.
Experts say the finding reinforces the value of global wildlife surveillance programs, which serve as an early warning system for potential zoonotic threats. Tracking these viruses before they spill over into human populations remains a critical step in preventing future pandemics.
Delhi Air Pollution: Damage Risks Are Beyond Your Lungs, It Can Affect Your Kidney Too, According To Doctor
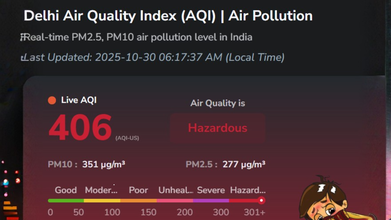
Credits: AQI.in
As of 6.17am on October 30, 2025, the AQI in Delhi is recorded at 406, and falls under the category 'Hazardous'. Major pollutants are PM2.5, PM10, CO, So2, No2, and O3. We have long known air pollution's impact on respiratory health and lungs, however, it is beyond that. With levels as high as 'hazardous', the pollution could also damage our kidneys.
Dr Sanjeev Gulati, nephrologist in Fortis, Delhi, writes that the detrimental effects of air pollution are not only evident in the respiratory and circulatory system, but it can also extend to renal function. He writes, "The kidneys are particularly vulnerable to the toxic effects of environmental pollutants due to their critical role in filtration. Environmental and occupational exposure to pollutants remains a common cause of kidney disease globally, especially in developing countries."
Up to 22% of the global disease burden and 23% of deaths are attributed to environmental pollution. There have been various studies that show the long-term exposure from particulate matter and how it is linked to an increased risk of membranous nephropathy and decline in renal function.
What Is Membranous Nephropathy?
It is a kidney disease caused by the damage to the kidney's filtration system. This could lead to significant protein leakage into the urine. This could happen due to the PM exposure.
In fact, a 2025 study published in the Journal of the American Society of Nephrology highlighted the role of air pollution in the rising risk of new kidney diseases. The study was able to track 2.5 million veterans, who were free of kidney diseases in 2003 and 2004, over an average of 8.5 years. The researchers then compared their health outcomes to air pollution levels. The study then found that for every 10 microgram increase in pollution per cubic meter of air, there was a 25 to 37% increase in new kidney disease case, a 36% rise in rapid kidney function decline, and a 31% increase in the risk of kidney failure requiring dialysis.
How Does Pollution Damage Your Kidney?
Dr Sean Hashmi, MD, MS, FASN, a board-certified nephrologist and obesity medicine specialist in the Southern Carolina, US, in a video on his YouTube channel that he uploaded to explain the impact of air pollution on kidney says, "your kidney is force to process a chemical soup day after day after day. And the main villain here is PM2.5."
Dr Hashmi notes that once the PM2.5 is in your bloodstream, your body treats them like foreign invaders. "This triggers powerful inflammation throughout your system. Inflammation is your immune system's response to injury and threat. However, when inflammation becomes chronic [due to long exposure of PM2.5], it can damage healthy tissues."
He says, as a result, these particle-filled blood arrives in your kidney. "Your kidneys have millions of tiny filters glomerulus, they are like cluster of blood vessels that act like coffee filters for your blood. The constant flow of abrasive particles creates low-grade sand blasting on these fragile filters. Over years this leads to permanent scarring and reduced kidney functions."
A Mysterious New Fungal Infection Is Spreading In UK Hospitals, Health Expert Warns

Credits: Canva
Health officials across the UK are on alert after identifying a new fungal infection spreading in hospitals. Known as Candidozyma auris (C. auris), this yeast has been named a critical priority pathogen by the World Health Organisation (WHO) because of its growing resistance to treatment and potential danger to vulnerable patients. The UK Health Security Agency (UKHSA) is now working with NHS England and other health partners to monitor rising detections of C. auris, which until recently had been rare in the country. Globally, the infection has been linked to a high death rate, raising concern for hospitalised patients with weakened immune systems.
What Is Candidozyma Auris?
C. auris is a type of fungus that can lead to severe infections, particularly among those who are already ill. Some strains have shown resistance to multiple antifungal drugs, making treatment difficult. It spreads most often in hospitals and long-term care facilities. According to the Cleveland Clinic, infections may include:- Ear infections
- Wound infections
- Urinary tract infections (UTIs)
- Bloodstream infections that can spread throughout the body
Unlike other Candida species, C. auris does not typically live naturally on the body. People usually contract it from contaminated hospital surfaces or from someone who already has the infection. For healthy individuals, the risk of infection remains low.
How Common Are Candidozyma Auris Infections?
C. auris remains uncommon but is considered an emerging infectious disease due to the rising number of reported cases since 2019. Healthcare professionals are increasing infection-control measures to contain its spread in hospitals and care homes.Symptoms Of Candidozyma Auris
The symptoms vary depending on which part of the body is infected. Common signs include:- Fever
- Chills
- Fatigue or extreme tiredness
- Low blood pressure
- Rapid heartbeat (tachycardia)
- Low body temperature (hypothermia)
- Ear pain, pressure, or a sense of fullness (in ear infections)
According to a UKHSA statement, C. auris was first discovered in 2009 in the ear of a patient in Japan and has since been detected in over 40 countries across six continents. The agency explains that the fungus is particularly concerning because it can survive for long periods on surfaces—even in hospital settings—and is often resistant to both standard medical treatments and disinfectants.
Since 2015, several long-lasting outbreaks of C. auris have occurred in UK hospitals, requiring intensive control measures to stop further transmission. Peaks in cases have mostly been linked to these outbreaks.
Can Candidozyma Auris Be Cured?
C. auris infections can often be treated with a type of antifungal medication called echinocandins. However, certain strains are developing resistance, making them more difficult to cure. In such cases, doctors may need to combine different drugs to eliminate the infection. Before starting any medication, it is important to consult a qualified healthcare professional for proper diagnosis and treatment advice.
© 2024 Bennett, Coleman & Company Limited

