- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
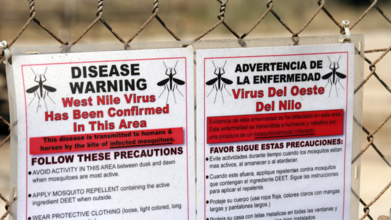
West Nile Virus Isn't Over Yet, New Cases In US On Rise
Credits: Canva
In Northeast Ohio, late summer usually means backyard cookouts, packed ballfields, and sticky, humid nights. This year, though, it has brought something less welcome: a rise in mosquito bites, and a rise in West Nile virus (WNV) cases.
Local health departments reported that two residents, one in Medina County and another in Cuyahoga County, tested positive for West Nile virus in August, according to Ideastream Public Media. Data from the Ohio Department of Health showed six confirmed cases statewide as of August 21.
Nationwide, the numbers tell a bigger story. According to the Centers for Disease Control and Prevention (CDC), there have been at least 771 human cases reported across 39 states as of September 9. Alarmingly, 490 of those cases were neuroinvasive, meaning they affected the brain or spinal cord, and were potentially life-threatening.
West Nile Virus: The Most Common Mosquito-Borne Illness
West Nile virus remains the most common mosquito-borne illness in the continental United States, according to Vector Disease Control International. Most infected people never develop symptoms, but those who do may experience fever, body aches, nausea, vomiting, or a rash.
In about 1 in 150 cases, the virus causes brain inflammation or meningitis, which can be deadly.
Older adults and immunocompromised individuals face the highest risk of severe complications. “Protecting yourself is especially important for people who are more at risk,” CBS News chief medical correspondent Dr. Jon LaPook emphasized, urging the public to use repellent, wear long sleeves, and drain standing water near their homes.
Also Read: West Nile Virus Spotted In Weld County Mosquitoes, Here’s What You Need To Know
Why This Outbreak Is Concerning
This year’s surge is not random. Mosquitoes thrive in warm, wet conditions. Longer, hotter summers and heavier rainfall, both linked to climate change, mean longer breeding seasons and more stagnant pools where larvae grow.
"It's always worse in the summer because that's when the mosquito population is at its highest," said Dr. Amy Edwards, an infectious disease specialist at University Hospitals in Cleveland, as reported in The Cool Down. She added that Ohioans face a very different risk today than a generation ago: “For people who grew up in Ohio, mosquitoes and ticks didn't used to carry disease here. Across the U.S., the rate of mosquito-borne illness is going up.”
The trend isn’t limited to West Nile. Lyme disease has been spreading to areas previously considered too cold for ticks, and dengue fever has reemerged in Florida, all signs of vector-borne diseases finding new footholds.
Also Read: Parkinson’s Mystery Cracked? Study Finds Brain Cells May Be Burning Themselves Out
Season Isn’t Over Yet
Public health officials stress that the danger is far from gone. “Infections can continue to occur until the first hard frost of the season, which is likely still many weeks away,” said Dr. Robbie Goldstein, Massachusetts’ public health commissioner, in a recent advisory. He urged people to remain vigilant, as mosquito activity remains high through early fall
The CDC updates its case counts biweekly through ArboNET, a national arboviral surveillance system. The agency notes that symptoms can take between two to fourteen days to appear after a mosquito bite, and in people with weaker immune systems, it can take even longer.
Prevention Remains the Best Defense
There is currently no specific treatment for West Nile virus. For most, recovery involves managing symptoms such as fever and fatigue. Severe cases may require hospitalization for intravenous fluids or even respiratory support.
Health experts recommend taking steps to minimize mosquito exposure:
- Use EPA-registered insect repellent containing DEET, picaridin, or oil of lemon eucalyptus.
- Wear long-sleeved shirts and pants, especially during dawn and dusk when mosquitoes are most active.
- Eliminate standing water in flowerpots, gutters, and other outdoor containers.
- Ensure window and door screens are intact to keep mosquitoes out.
West Nile Virus In The US
West Nile virus, first detected in the U.S. in 1999, is now a recurring part of late summer and early fall. Its growing prevalence serves as a warning of how climate change, urbanization, and changing ecosystems can amplify public health threats.
As the season continues, experts urge residents to stay proactive rather than complacent. The mosquito buzzing around your backyard may be more than an annoyance, it could be carrying a virus that has sickened hundreds this year and shows no sign of stopping.
UK Faces Shortage Of This Common Pain Medicine Till June

Credits: Canva
A shortage of prescription-strength co-codamol is set to continue until at least June, leaving thousands of chronic pain patients across the UK uncertain about how they will manage daily symptoms. The Scottish government has confirmed limited availability of the strongest 30/500mg tablets, while health boards warn alternative medicines may not fully cover demand.
The shortage is linked to delays in authorization by the Indian government for exporting key codeine-based ingredients needed to manufacture the drug.
Patients Told To Taper Use
Many patients say they first learned of the disruption through calls from local health services. Some have already been advised to slowly reduce their dose to avoid withdrawal symptoms.
Jocelin Harrison, who has relied on the medication for more than three decades after five spinal surgeries, said she was contacted by NHS Lanarkshire and instructed to cut down gradually.
“The only advice I’ve been given so far was to reduce the tablets and try to manage my withdrawal symptoms,” she said, as reported by the BBC.
“I was not offered any other advice or possible replacement pain killers and it’s a great worry for me and other chronic pain sufferers throughout Scotland and the UK.”
Doctors warn that abruptly stopping co-codamol can trigger headaches, nausea, sweating and a sudden increase in pain, particularly for long-term users.
Why Does This Drug Matter So Much?
Co-codamol combines paracetamol with the opioid codeine and is commonly prescribed after surgery or for persistent musculoskeletal conditions. It comes in three strengths: 8mg, 15mg and 30mg of codeine with 500mg paracetamol.
The lowest strength is available over the counter, but the stronger forms require a prescription and are widely used by patients with chronic pain. Because codeine can cause dependence, tapering rather than stopping suddenly is considered essential.
Health boards say supplies of alternative strengths are also limited, making it difficult to simply switch everyone onto another version.
Guidance issued locally states patients, except those undergoing cancer treatment, should gradually reduce usage until stopping completely. No new patients will be started on the medication until supplies stabilize.
What Are The Alternatives?
NHS Grampian has urged pharmacists to prioritize existing stock carefully. However, it stopped short of telling patients to immediately begin cutting back, highlighting variation in local guidance.
Officials acknowledge substitutes exist, but warn they cannot meet the expected rise in demand from patients switching medicines.
Authorities Now Work On Solution
Scotland’s chief pharmaceutical officer Alison Strath said the issue ultimately sits with UK-wide medicine supply systems but confirmed discussions are ongoing.
“Supply issues are expected until June 2026 and we are in regular contact with the UK government to seek assurances they are doing all they can to resolve this,” she said, adding that affected patients will be contacted directly about alternative treatment options.
The UK Department of Health and Social Care said most medicines remain readily available and manufacturers are working to restore production.
The shortage highlights the global nature of generic drug manufacturing. Medicines such as co-codamol 30/500mg are typically produced using ingredients sourced from India and China, meaning regulatory or production delays overseas can quickly affect patients at home.
For now, patients are being urged not to contact GP practices unless advised and to wait for further instructions from their health providers.
Measles Outbreak In UK: Virus Spreads Among Unvaccinated Children In London
Credits: Canva
Measles Outbreak In UK: A measles outbreak has been confirmed in London's north east area, noted the BMJ. As per the medical journal, the outbreak is among the unvaccinated children. The medical journal also noted that there have been 96 laboratory confirmed cases of measles in England between January 1 to February 9, 2026 and more than a third, which is 34 cases are from Enfield. BMJ also noted that Enfield is also the area with lowest vaccination rates.
As per the data by the UK Health Security Agency or the UKHSA, only 64.3% of 5 year-olds Enfield received both doses of the measles, mumps, and rubella or the MMR vaccine in 2024 and 2025. The majority (74 of 96, 77%) of measles cases confirmed in the UK so far this year were in children aged 10 and under. Some 64% of cases have been in London, 26% in the West Midlands, and 4% in the East Midlands.
Read: Unique Symptoms Of Measles In 2026 And How Long Does The Infection Last?
Measles Outbreak In UK: Previous Cases And How It Made A Comeback
Last month, the World Health Organization revoked the United Kingdom’s measles elimination status after the virus was found to be circulating continuously for over a year.
In 2025, a child in Liverpool died after contracting measles, prompting renewed pressure on the NHS and government to address its return. England recorded 959 laboratory-confirmed cases that year. Although lower than the 2,911 cases in 2024, it still marked the highest annual total since 2012.
Vaccine uptake has steadily declined over the past 12 years. Only 84.4% of children in the UK receive both doses of the MMR vaccine by age five, far below the 95% coverage needed for herd immunity.
Why Has Measles Return To The UK?
In late 2023, measles outbreaks were reported in the UK, which led to a surge in cases in 2024. Vaccination uptake at the end of 2024 was 92% for the first dose, however, for the second dose, it was below 82%.
Dr Vanessa Saliba, consultant epidemiologist at UKHSA said, "Infections can return quickly when childhood vaccine uptake falls - measles elimination is only possible if all eligible children receive two MMRV doses before school. The NHS is making vaccination easier, including offering the second MMRV dose earlier at a new 18-month appointment to boost uptake and support elimination goals."
Read: UK Loses Measles Elimination Status: Why Is This Disease Making A Comeback?
She also noted that children and adults must get vaccinated as NHS also offers catch-up jabs.
Dr Baharat Pankhania, from the University of Exeter, as reported by the BBC said, "Measles is an infection that can be prevented by vaccine - and it's extremely concerning that in the UK we now have pockets of low or no vaccine uptake. We urgently need to remedy this situation." Pankhania also noted that there is a need to make the access to GPs easier, and for an effort that could immunize babies in their homes and counter wrong information around vaccine safety.
India AI Summit: Union Health Minister Nadda Launches SAHI And BODH Initiatives To Boost AI In Healthcare

The Union Minister of Health and Family Welfare, JP Nadda, today launched two key national initiatives -- the Strategy for Artificial Intelligence in Healthcare for India (SAHI) and the Benchmarking Open Data Platform for Health AI (BODH) to boost the role of AI in the country's healthcare ecosystem.
The initiatives, launched at the India AI Summit at Bharat Mandapam, in the national capital, are aimed at promoting safe, transparent, and accountable AI in healthcare. It will also help strengthen the digital health ecosystem for equitable healthcare access.
What is SAHI and BODH?
SAHI is a national guidance framework to enable the safe, ethical, evidence-based, and inclusive adoption of AI across India’s healthcare system.
It aims to provide strategic direction on governance, data stewardship, validation, deployment, and monitoring of AI solutions, while supporting States and institutions in responsible adoption aligned with public health priorities.
"SAHI is not merely a technology strategy but a governance framework, policy compass, and national roadmap for the responsible use of AI in healthcare,” said Nadda.
He stated that SAHI will guide India in leveraging AI in a manner that is ethical, transparent, accountable, and people-centric. Nadda also emphasized that SAHI provides a structured framework for collaboration, ensuring that innovation flourishes while public interest remains paramount.
The second initiative, BODH, was developed by the Indian Institute of Technology Kanpur in collaboration with the National Health Authority. It is a privacy-preserving benchmarking platform that enables rigorous evaluation of AI models using diverse, real-world health data without sharing underlying datasets.
As a digital public good under the Ayushman Bharat Digital Mission, it is designed to strengthen trust, transparency, and quality assurance in Health AI deployment.
"The collaboration between Government and academia has led to the development of BODH -- the Benchmarking Open Data Platform for Health AI -- which provides a structured mechanism for testing and validating AI solutions before deployment at scale,” said Nadda.
Nadda reiterated that AI solutions must be rigorously evaluated for performance, reliability, and real-world readiness. Together, SAHI and BODH represent India’s commitment to building a trustworthy, inclusive, and globally competitive health AI ecosystem grounded in innovation, responsibility, and public trust.
AI An Indispensable Enabler to Viksit Bharat
Earlier, delivering the keynote address at a session themed “Innovation to Impact: AI as a Public Health Game-Changer”, at the Summit, Anupriya Patel, Union Minister of State for Health and Family Welfare, highlighted AI as an "All-Inclusive Intelligence".
She also emphasized AI's potential in addressing "health inequities across the country".
Patel called technology -- particularly AI "an indispensable enabler" in India's race towards the vision of a Viksit Bharat by 2047.
She highlighted the potential role of AI on India’s vast and diverse population, the rural–urban divide, and the dual burden of communicable and non-communicable diseases, which present unique challenges.
She also noted that AI has been integrated across the entire continuum of healthcare -- from disease surveillance and prevention to diagnosis and treatment.
© 2024 Bennett, Coleman & Company Limited

