- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Is Hormone Replacement Therapy for Menopause? What Will Change Under Recent FDA Guidelines?
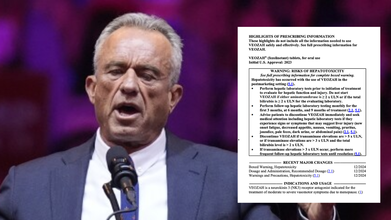
Credits: AP, FDA
US Secretary of Health and Human Services Robert F Kennedy Jr has announced the new plans of the Food and Drug Administration (FDA) to remove the "black box" warning on the hormone treatments used by women with menopause symptoms. This is the big, lengthy, physical black box on the label of the menopause hormone therapy that includes the risks like cardiovascular disease, stroke, breast cancer, and dementia. FDA is now saying that it will take away the black box warning.
This is based on a 2002 study, as quoted by RFK Jr too that warns that the use of menopause hormone therapy could raise the risk of all the conditions mentioned inside the black box.
However, since then, it was found that some of those risks, mentioned on the label, were, in fact, misrepresented and overstated. It was found that within the 10 years of menopause onset, this therapy could really be beneficial, reports CNN. It was found that the therapy would not only prevent women from hot flashes and night sweats, which are the typical symptoms of menopause, but it would also benefit them in the long run, by protecting from bone fractures.
The FDA hopes to remove this label starting in the next few months, with the hope that it would also remove the fear around women into using these therapy treatment.
The CNN reported that while the new label will still have some of those warning, however, it won't be the "absolute, strongest warning" on the label that is the first thing the women see.
What Is Hormone Therapy For Menopause?
As per the Cleveland Clinic, hormone replacement therapy or HRT, is a treatment that helps people with symptoms of menopause.
Healthcare providers also call it hormone therapy (HT), especially when you receive it after age 50. Hormone replacement therapy or HRT is the term providers use when you receive the treatment at a younger age, especially before age 40.
When you’re moving into menopause, your ovaries naturally slow down and produce much less estrogen. That drop can trigger a bunch of uncomfortable symptoms, like:
- Hot flashes
- Night sweats
- Vaginal dryness or pain during sex
- Mood swings, low moods, or irritability
- Trouble sleeping
- Pee leakage
Hormone replacement therapy (HRT) basically gives your body back the hormones it’s no longer making enough of. Once those levels stabilize, many people feel a lot better. HRT can also help protect your bones, since low estrogen is linked to conditions like osteoporosis and osteopenia.
That said, HRT isn’t a one-size-fits-all solution. Whether it’s right for you is something worth discussing with your healthcare provider. It can ease symptoms, but it also comes with its own risks. A good, honest conversation about the pros and cons will help you figure out what’s best for your body.
Is Hormone Therapy Same As The Hormone Replacement Therapy?
Hormone therapy (HT) is a broader term that implies to any type of treatment involving hormones. It could include any therapy involving hormone, including hormone therapy for cancer, or to treat certain hormone imbalances. However, hormone replacement therapy (HRT) usually means the hormones are replacing the natural hormones your body is no longer making, especially for people in their 30s or early 40s.
There are two types of HRT, estrogen therapy and combination therapy, which means a combination of estrogen and progesterone.
Alex Singleton Opens Up About His Surgery For Testicular Cancer

Credits: AP
Alex Singleton, American football linebacker has undergone a surgery on Friday to have a cancerous tumor removed from one of his testicles. He told this to his teammates and coaches in an emotional team meeting on Monday morning. His family and few of his close friends, including some team officials were the only ones who knew.
"Cancer is a scary word, still is, still freaks me out just saying it," he said to one of the local reporters, as reported by ESPN.
How Was He Diagnosed?
His diagnosis came in ways one would not expect. Before the Houston Texans game on Wednesday, Singleton, 31, was to take the league-mandated random drug test, which showed that he had elevated levels of hormone hCG in his system. He said that he knew he was not taking hCG. This is what led him to make an appointment with a urologist and then he underwent several tests. He also underwent a CT scan and ultrasound scan and received the notice last Monday that a tumor on his testicle was cancerous. After this, his surgery was scheduled.
However, he told his doctors that he wanted to play in Thursday night's game against the Las Vegas Raiders.
What Is Testicular Cancer?
As per the Urology Care Foundation and the American Urological Association, testicular cancer happens when cells in the testicle grow to form a tumor. Though this is rare, more than 90% of testicular cancers begin in the germ cell, which produce sperm.
There are two types of germ cell cancers (GCTs). Seminoma can grow slowly and respond very well to radiation and chemotherapy. Non-seminoma can grow more quickly and can be less responsive to those treatments. There are a few types of non-seminomas: choriocarcinoma, embryonal carcinoma, teratoma and yolk sac tumors.
There are also rare testicular cancers that don’t form in the germ cells.
What Are The Common Symptoms Of Testicular Cancer?
Some of the symptoms of testicular cancer could be difficult to note at first, however, there are symptoms that one should note for:
- Painless lump in the testicle
- Swelling of testicles, with or without pain
- Dull ache or pain in the testicle, scrotum, or groin
- Tenderness or changes in the male breast tissue
The Urology Care Foundation notes that around 75 of 100 men who have swelling or a lump in their testicles have cancer. Most masses in the scrotum outside of the testicle are not cancer, however, you must tell your doctor if you do detect a lump.
The longer you wait the more chances are for the cancer to grow and spread.
Who Are More Prone To Testicular Cancer?
The risk of testicle cancer rises for men with
- Family history: If you had someone in your family, including your father or brother with testicular cancer
- Undescended Testicles: If your testicles did not drop before birth. This is also called cryptorchidism, when the testicles do not drop from abdomen into the scrotum before birth as it should. About 8 out of 100 of patients get cancer like this.
- GCINS: These are odd cells in the testicle called germ cell neoplasia in situ (GCNIS) and they are typically found during an infertility test.
Can You Check For Lumps Yourself?
Yes, you can. The process is to first be relaxed, then to firmly roll each testicle between the thumb and forefingers to check for any lumps or if any of the testis feel larger than the other. See if you feel any lump or pain around the area. Make it a habit, and look for any changes in size, shape or texture.
Hormone Replacement Therapy For Menopause No Longer Carries a ‘Black Box’ Safety Warning — What Does This Mean?

Credits: Canva
Hormone Replacement Therapy: The U.S. FDA has announced it will remove the long-standing black box safety warnings from all hormone replacement therapy (HRT) products used to manage menopause and perimenopause symptoms. The move comes after new evidence suggested that earlier studies overstated the risks of heart disease, stroke, and cancer linked to HRT.
The U.S. Food and Drug Administration (FDA) has announced that it will remove the black box safety warnings from all forms of hormone replacement therapy (HRT)—including creams, pills, and other treatments used to manage menopause and perimenopause symptoms.
The warnings, which appeared on labels for over two decades, suggested that these therapies could increase the risk of cancers, dementia, heart disease, and strokes. However, FDA Commissioner Dr. Marty Makary told CBS News that those cautions likely discouraged many women from using treatments that might actually improve their long-term health.
“We now have a more nuanced understanding,” Dr. Makary said, as per CNN News. He further said, “We want to put that fear in context and let people know that there are tremendous long-term health benefits.”
Hormone Replacement Therapy: What Is It?
HRT, or Hormone Replacement Therapy, is a treatment that helps restore hormones the body no longer produces in sufficient amounts. It is most often prescribed to ease menopause symptoms such as hot flashes by supplementing estrogen and progesterone, the hormones that naturally decline during this stage. According to the NHS, HRT may also be recommended for other hormonal deficiencies, including those caused by thyroid or pituitary gland disorders.
Hormone Replacement Therapy: What Does Removing the Black Box Safety Warning Mean?
Removing the black box warning signals a significant shift in how hormone replacement therapy is viewed by regulators and the medical community. The decision suggests that the potential benefits of properly prescribed HRT now outweigh the earlier perceived risks.
It also means that doctors may feel more confident recommending these treatments for women struggling with menopause symptoms such as hot flashes, mood changes, and vaginal dryness—especially when therapy is started around the time of menopause rather than years later.
However, experts still stress that hormone replacement therapy is not one-size-fits-all. Women should discuss their personal and family medical history with their doctor to decide whether HRT is the right choice for them.
Hormone Replacement Therapy: Why Hormone Replacement Therapy Had the Warning?
In 2002, the landmark Women’s Health Initiative study linked hormone therapy to higher rates of breast cancer and stroke, prompting the FDA to issue the now-familiar black box warning—the strongest alert it can give.
But since then, newer research has challenged those early conclusions. Studies now show that hormone replacement therapy, particularly when started early, may reduce the risk of heart disease, improve bone health, and even protect against cognitive decline.
This shift in scientific understanding pushed many doctors to call for the warning’s removal, arguing that the outdated label created unnecessary fear and confusion among women seeking menopause relief.
Hormone Replacement Therapy: How the FDA Reached Its Decision
As per USA Today, in July, the FDA organized an expert panel to evaluate whether the warnings should remain, especially for low-dose vaginal estrogen products. After the meeting, the agency opened a public comment period and received nearly 3,000 responses by late September.
The American College of Obstetricians and Gynecologists (ACOG) has long supported reviewing the label on low-dose vaginal estrogen, which acts locally rather than systemically. However, ACOG also raised concerns that the July panel lacked the depth and transparency of a standard FDA advisory committee meeting.
“A two-hour expert panel should not replace a full advisory committee discussion,” ACOG stated in its formal comment, urging the FDA to hold separate, detailed reviews for vaginal and systemic hormone therapy options.
Despite these reservations, the FDA shared several supporting studies, including evidence that hormone replacement therapy can reduce the risk of Alzheimer’s disease, heart attack, and hip fractures. Many of these findings date back to research published between the 1980s and early 2000s.
The FDA’s decision to drop the black box warning from menopause-related hormone treatments marks a turning point in women’s health care. As research continues to clarify the true risks and benefits of hormone replacement therapy, the move could help many women make more informed and less fearful decisions about managing menopause safely and effectively.
Can’t Control Cholesterol With Statins? Scientists Say A New Experimental Pill Shows Strong Results

Credits: Canva
For many people living with high cholesterol, diet changes and daily statin therapy may not be enough to hit their target levels. A new experimental pill, however, could provide an additional option for those struggling to control their low-density lipoprotein (LDL), or “bad,” cholesterol.
Recent Phase 3 trial data revealed that participants who took the investigational drug ‘enlicitide’ alongside their usual cholesterol-lowering treatment saw reductions in LDL cholesterol of up to 60% after 24 weeks. This was compared to participants who continued their standard therapy with a placebo. The study included adults with elevated LDL and either a history of major cardiovascular events or an increased risk of such events, as per CNN.
The results, which have not yet appeared in a peer-reviewed journal, were shared at the American Heart Association’s Scientific Sessions.
High LDL cholesterol contributes to plaque buildup in arteries, which can increase the risk of heart disease, which is the leading cause of death in the U.S., with a fatality occurring roughly every 34 seconds.
New Daily Pill May Cut Bad Cholesterol By 60%
Merck, the company behind enlicitide, intends to apply for FDA approval early next year, according to Dr. Puja Banka, associate vice president of clinical research and global clinical development.
“We aimed to see what enlicitide could achieve on top of statins, because about 70% of patients on lipid-lowering therapy still don’t reach guideline-directed targets,” said Banka.
When Statins Alone Are Not Enough
The trial enrolled 2,912 adults, averaging 63 years old, who had previously suffered a heart attack or stroke or were at medium-to-high risk for one over the next decade. Data was collected across 14 countries between August 2023 and July 2025.
All participants had elevated LDL levels despite at least 30 days on stable lipid-lowering therapy, mostly statins. About 97% were on statins, and 26% were taking another cholesterol-lowering medication. During the trial, some participants were given enlicitide once daily, while others received a placebo, as per CNN.
Enlicitide belongs to a class of drugs called PCSK9 inhibitors, which work by helping the body clear LDL cholesterol from the bloodstream. Statins, by contrast, block a liver enzyme to increase LDL removal.
“Because enlicitide works differently from statins, it’s expected to further lower LDL cholesterol when used in combination,” explained Dr. Kristin Newby, a cardiologist at Duke University School of Medicine, who was not involved in the trial.
As per CNN, after 24 weeks, participants on enlicitide experienced sustained LDL reductions through 52 weeks, along with:
- A 53% drop in non-HDL cholesterol
- A 50% decrease in ApoB, a protein that carries harmful cholesterol in the body
- A 28% reduction in lipoprotein(a), a type of fat linked to heart disease
Safety and Side Effects
Around 10% of participants on enlicitide experienced serious adverse events, compared with 12% in the placebo group. Side effects were generally balanced between both groups, with no particular event standing out. Reported issues included gastrointestinal symptoms and certain infections.
“This suggests no major or frequent safety concerns,” said Newby, as per CNN. “However, larger, long-term studies and post-marketing surveillance will be needed to monitor for rarer side effects. The key takeaway is that enlicitide is highly effective at lowering LDL cholesterol—about 55% more than placebo when added to statins—and helps more people reach treatment goals.”
A New Option for Cholesterol Management
For patients who don’t fully respond to statins, injectable PCSK9 inhibitors are already available. But unlike those treatments, enlicitide is an oral daily pill, offering an easier administration route that some patients may prefer. Banka called it “the first oral PCSK9 inhibitor to complete Phase 3 trials.”
Previously, studies have shown that injectable PCSK9 inhibitors, like evolocumab (Repatha), can reduce the risk of first-time major cardiovascular events in adults with atherosclerotic cardiovascular disease or diabetes. In trials across 33 countries, 12,257 adults taking evolocumab for an average of 4.6 years saw a 25% reduction in heart attack, stroke, or coronary deaths compared with placebo. The FDA has already approved evolocumab for patients with established cardiovascular disease or as an add-on therapy for high cholesterol.
The new enlicitide trial marks the first demonstration of a non-statin PCSK9 inhibitor improving cardiovascular outcomes in patients without a prior heart attack or stroke who were already on intensive lipid-lowering therapy.
© 2024 Bennett, Coleman & Company Limited

