- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
What Are The New COVID-19 Variants Spreading In May 2025?
Health and me
The most recent entrant to the WHO’s list is NB.1.8.1, derived from recombinant ancestor XDV.1.5.1. With multiple mutations in its spike protein, NB.1.8.1 is being closely observed for its potential to escape immune responses.
More than five years since COVID-19 was declared a pandemic, the virus is far from gone. While global headlines may no longer be dominated by daily case counts, SARS-CoV-2—the virus responsible for COVID-19—continues to evolve, adapt, and spread in communities worldwide. In May 2025, a new wave of variants is quietly shaping the trajectory of the virus and prompting renewed concern among scientists and health professionals.
Viruses are, by nature, constantly mutating. As SARS-CoV-2 moves from person to person, random genetic changes—known as mutations—accumulate. Most mutations are harmless, but some enhance the virus’s ability to spread, evade immunity, or cause severe illness.
When a group of mutations significantly alters the virus's behavior, it is classified as a variant. These variants are then grouped by the World Health Organization (WHO) and CDC into three broad categories:
- Variants Under Monitoring (VUM)
- Variants of Interest (VOI)
- Variants of Concern (VOC)
This classification is vital for public health responses, vaccine development, and treatment planning.
Current Variants Circulating in May 2025
According to global health monitoring systems, the major COVID-19 variants circulating in May 2025 include:
- KP.3
- KP.3.1.1
- LB.1
- XEC
- LP.8.1
- NB.1.8.1
Notably, all of these are descendants of Omicron, specifically from the lineage KP.1.1.3, itself a subvariant of JN.1—the dominant variant during the winter surge of 2023–2024.
| COVID-19 VARIANT | FEATURE | SYMPTOMS |
| KP.3 | KP.3 belongs to a cluster of Omicron descendants collectively referred to as FLiRT variants. This group also includes KP.2 (the prior dominant variant in the U.S.) and KP.1.1. Though KP.3 hasn’t demonstrated drastically different clinical outcomes, it continues to be the most prevalent variant across the U.S. and parts of Europe. | Fever or chills, Cough, Shortness of breath, Fatigue, Loss of taste or smell, Sore throat, Diarrhea and nausea |
| KP.3.1.1 | A sublineage of KP.3, KP.3.1.1 is emerging as a significant global variant. It is now the most common variant among the JN.1-derived strains, contributing to sustained hospital visits and positive test rates, especially in at-risk age groups. | Although not more severe in symptoms, its high transmissibility raises concerns for immunocompromised individuals and communities with low vaccination rates. |
| LB.1 | Ranked third among the current U.S. variants, LB.1 has caught attention for anecdotal reports of particularly severe sore throats. It is, again, part of the FLiRT family and a direct descendant of JN.1. | Intense sore throat, Fatigue, nasal congestion, Fever |
| XEC | XEC is different from its peers—it's a recombinant variant, meaning it emerged from the blending of two separate Omicron strains, KS.1.1 and KP.3.3, within a single infected individual. | High fever, Muscle aches, Sore throat, Dry cough, Extreme tiredness |
| LP.8.1 | First identified in July 2024 and now labeled a Variant Under Monitoring by the WHO, LP.8.1 has demonstrated significant growth in multiple countries. | Continuous cough, Loss of taste or smell, Shortness of breath, Muscle aches, Gastrointestinal discomfort |
| NB.1.8.1 | The most recent entrant to the WHO’s list is NB.1.8.1, derived from recombinant ancestor XDV.1.5.1. With multiple mutations in its spike protein, NB.1.8.1 is being closely observed for its potential to escape immune responses. | Fever, Dry cough, Sore throat, Headache, Mild gastrointestinal issues |
Can COVID-19 Tests Identify the Variant?
Most standard COVID-19 tests (PCR or antigen) only detect whether the virus is present—not which variant you’ve contracted. For that, scientists rely on genomic sequencing, which is typically used for public health tracking rather than individual diagnosis.
So if you test positive, assume you may have one of the circulating variants and act accordingly.
Do the Current Vaccines Work?
While some variants can partially evade immunity, vaccination remains one of the most effective ways to reduce severe illness, hospitalization, and death.
Current recommendations from public health agencies include:
- Getting the updated bivalent or variant-specific booster
- Wearing masks in crowded indoor settings
- Avoiding high-risk environments, especially if you're immunocompromised
- Practicing good hand hygiene
- Isolating if you feel sick
As one infectious disease expert put it, “We still have a lot of virus in circulation—masks, vaccines, and vigilance continue to be our best tools.”
In May 2025, the COVID-19 landscape continues to shift. While symptoms largely mirror earlier waves, the evolving nature of variants like KP.3.1.1, LB.1, and NB.1.8.1 highlights the importance of surveillance, booster uptake, and public awareness.
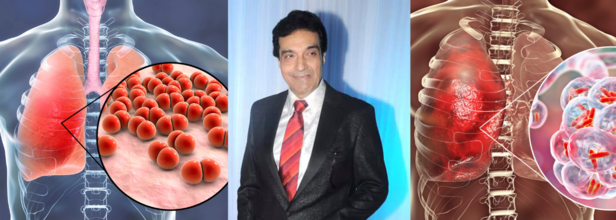
Veteran Actor Dheeraj Kumar Dies At 79 Due To Acute Pneumonia
Credits: Canva and Wikimedia Commons
Veteran actor and producer Dheeraj Kumar, best known for his contributions to Hindi and Punjabi cinema, passed away at a private hospital in Mumbai on Tuesday, July 15. He was 79.
Admitted with Pneumonia, Succumbed to Organ Failure
According to sources close to the family, Kumar had been admitted to the Intensive Care Unit after being diagnosed with acute pneumonia. His health took a critical turn on Monday as he suffered multiple organ failure and was subsequently placed on ventilator support. He breathed his last around 11 AM on Tuesday, with his son by his side in his final moments.
A Career That Began With a Talent Contest
Dheeraj Kumar’s journey into the world of entertainment began in the mid-1960s, when he participated in a talent contest that also featured Rajesh Khanna and Subhash Ghai. In a 2012 interview with The Hindu, Kumar recalled:
“In a talent contest in Mumbai in the 1960s, three were selected to be actors among some 10,000 aspirants — Rajesh Khanna, myself and Subhash Ghai... He became a superstar.”
Kumar went on to act in several films, including Rakhwala, Tyaag and Sargam, and shared screen space with many leading actors of the time. Over the years, he transitioned into television production and was known for creating popular shows such as Om Namah Shivay and Shree Ganesh. His last known collaboration with Rajesh Khanna was a TV series in 2019.
Understanding Pneumonia and Its Risks
As per the American Lung Association, pneumonia is an infection that causes inflammation in the air sacs (alveoli) of one or both lungs. These air sacs may fill with fluid or pus, leading to symptoms that range from mild to life-threatening. Acute pneumonia, in particular, can cause sudden and severe respiratory symptoms.
Some of the common symptoms include:
- Persistent cough with yellow, green, or bloody mucus
- High fever, sweating and chills
- Shortness of breath and chest pain while coughing or breathing
- Fatigue, nausea or vomiting
- Confusion, especially in older adults
Kumar’s condition is a reminder that pneumonia can escalate quickly, especially in older individuals or those with weakened immune systems.
Can Pneumonia Be Fatal?
Yes, pneumonia can be deadly—especially when left untreated or when it occurs in high-risk individuals. According to global estimates, as noted by the American Lungs Association, over 1.8 million people die from pneumonia each year, with children under five in low-income countries being the most vulnerable. In older adults, complications such as respiratory failure, sepsis, or organ failure often lead to death.
Bacterial pneumonia is more likely to require hospitalization, but viral and fungal forms can also be life-threatening. Vaccines such as the pneumococcal vaccine and flu shots can significantly reduce the risk of infection, particularly in older adults.
Maintaining overall health, timely vaccinations, and early medical intervention are critical in preventing complications.
After Jannik Sinner, Tara Moore Makes News Failing Her Doping Test, Resulting In A 4-Year Long Ban

Credits: Wikimedia Commons and Canva
After Jannik Sinner's news of anti-doping test, British tennis player Tara Moore is also making news. The 32-year-old was Britain's top ranked women's doubles player when she was provisionally banned in May 2022. Again, she has been banned for four years for a doping offence, though she had been cleared for the same by an independent tribunal just 18 months ago.
She was tested positive for nandrolone and boldenone at a tournament in the Colombian capital Bogota the previous month.
The reason Moore provided was due to the ingestion of contaminated meat. While in December 2023, an independent tribunal ruled that contaminated meat was the reason that the test came positive and Moore "bore no fault or negligence"; the International Tennis Integrity Agency (ITIA) thinks otherwise.
ITIA has been upheld by the Court of Arbitration for Sport (Cas). In the March hearing, Cas said in a media release: "After reviewing the scientific and legal evidence, the majority of the Cas panel considered that the player did not succeed in proving that the concentration of nandrolone in her sample was consistent with the ingestion of contaminated meat."
This means Moore will not be free to play again until the start of 2028 season. "The panel concluded that Ms Moore failed to establish that the ADRV (Anti-Doping Rule Violation) was not intentional. The appeal by the ITIA is therefore upheld and the decision rendered by the Independent Tribunal is set aside."
The ITIA chief executive Karen Moorhouse told BBC,"For the ITIA, every case is considered according to the individual facts and circumstances. In this case, our independent scientific advice was that the player did not adequately explain the high level of nandrolone present in their sample. Today's ruling is consistent with this position."
What Do Nandrolone Decanoate And Boldenone Do To You?
Nandrolone Decanoate: As per a 2020 study published in journal Medicina, nandrolone decanoate is an androgen, which means it plays a significant role in the development of male reproductive organs. The study notes: "The clinical use of synthetic testosterone derivatives, such as nandrolone, is focused on maximizing the anabolic effects and minimizing the androgenic ones." The study also mentions that apart from its clinical use, skeletal muscles can be considered as the primary target tissue. "Nowadays, especially athletes in power sports such as bodybuilding and weightlifting administer illegally high doses of Anabolic Androgenic Steroids (AAS) to increase their muscle mass and improve their overall performance," notes the study.
Nandrolone Decanoate injections have been classified under the Anabolic Steroids Control Act of 1990 and due to its serious health risks, it is banned by most sports organization and is also listed in the prohibition list by the World Anti-Doping Agency (WADA).
Side Effects Include:
- Infertility
- Liver Toxicity
- Impaired Lipid Profile
- High Blood Pressure
- Acne
- Hair Loss
- Gynecomastia
Boldenone: As per a 2016 study published in the Journal of Food and Drug Analysis, this AAS can be used in repairing wasting of the body caused by some emaciating disease. It can also be used for human sports for better performance and promoting the growth of skeletal muscle.
However, this is also used for increasing the body weight in livestock as growth-promoting agents. This is also one of the matters the study looks into, in order to "evaluate the safety and meat quality criteria in broilers following intramuscular injection of boldenone." This is the reason Moore too used in her defense, that the result of her positive test was contaminated meat.
The US Anti-Doping Agency (USADA) notes that there is no therapeutic or medical use for boldenone in humans. More specifically, it is not approved by the Food and Drug Administration (FDA) for use in humans for any reason. It also notes that WADA has included boldenone in its prohibited list. Since it could occur naturally at very low concentrations in the urine, WADA-accredited laboratories apply a specific analysis procedure called carbon isotope ratio mass spectrometry, or GC/C/IRMS, to differentiate between external administration and internal production.
What are the side effects? USADA notes that in men, boldenone causes decreased testosterone production and impacts the reproductive system and fertility of males. It also impacts the size of the testes, lower sperm count, and sperm mobility.
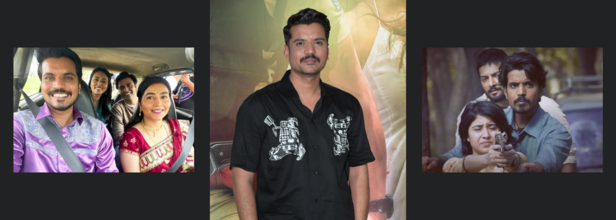
Panchayat's Asif Khan Suffers From A Heart Attack, Shares Updates
Credits: Canva
Actor Aasif Khan, known for his performances in Pataal Lok and Panchayat, recently suffered a heart attack and was admitted to Kokilaben Hospital in Mumbai. The incident occurred two days ago, sending a wave of concern among his fans and industry peers. Fortunately, his condition is now stable.
According to hospital sources, Aasif is recovering well and is likely to be discharged in a couple of days.
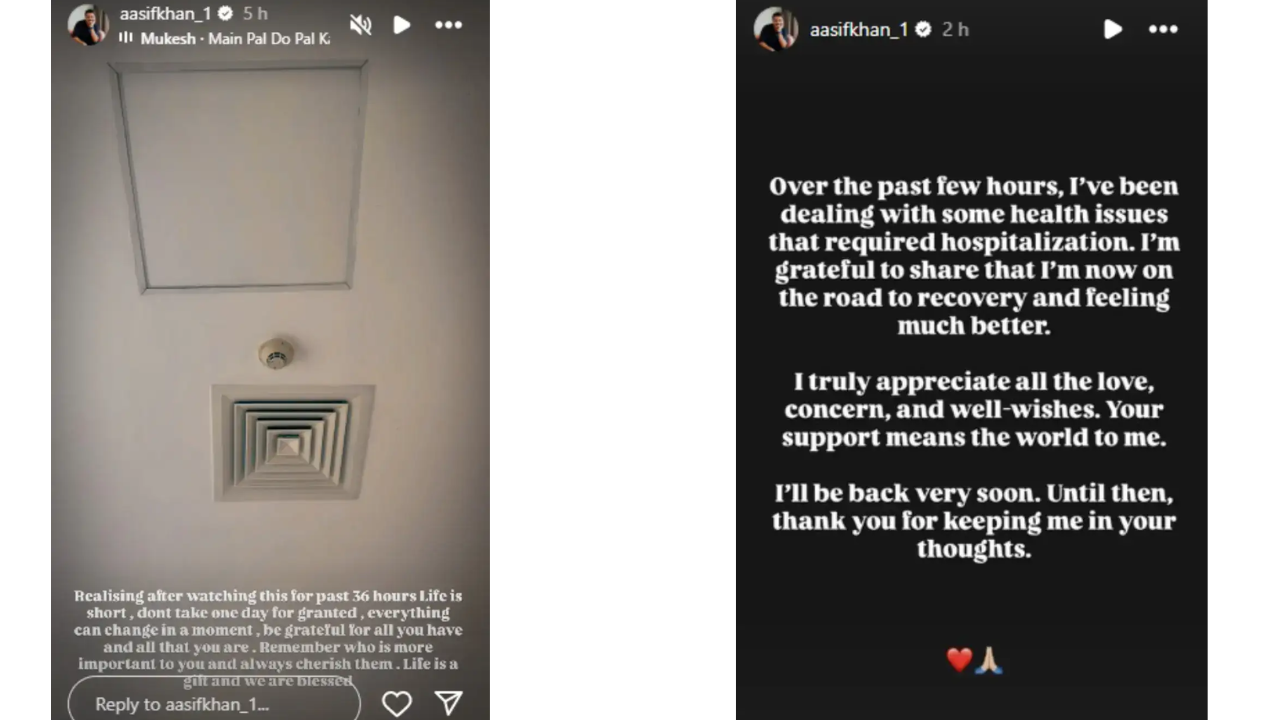
The actor took to his Instagram stories to share an update, along with a photo from his hospital bed. In a deeply reflective note, he wrote:
“Life is short, don’t take one day for granted. Everything can change in a moment. Be grateful for all you have and all that you are… Life is a gift and we are blessed.”
Recovering From Attack
In a brief statement to India Today, Aasif confirmed he had been dealing with a health issue that required hospitalization.
“I’m grateful to share that I’m now on the road to recovery and feeling much better,” he said. “I truly appreciate all the love, concern, and well-wishes. Your support means the world to me. I’ll be back very soon.”
His update comes as a reminder of how sudden and serious heart-related conditions can be—even among young and seemingly healthy individuals.
How Do Heart Attacks Happen?
A heart attack, or myocardial infarction, occurs when blood flow to a part of the heart is blocked, usually by a clot, causing damage to the heart muscle. It’s often linked to lifestyle factors like high cholesterol, smoking, stress, and lack of exercise—but can also strike unexpectedly.
While heart attacks are more common in those over 50, studies show a rising number of younger adults are now at risk. According to a 2019 study published in the Journal of the American College of Cardiology, one in five heart attack patients in the U.S. was under the age of 40.
In India, the numbers are more alarming. The Indian Heart Association notes that 50% of all heart attacks in Indian men occur under the age of 50, and 25% occur under the age of 40. Factors like sedentary lifestyles, unhealthy diets, and high stress contribute significantly.
Signs to Watch For
Aasif’s case highlights the importance of recognizing the early symptoms of a heart attack, which can include:
- Chest pain or tightness
- Pain in the left arm, jaw, or upper back
- Shortness of breath
- Cold sweat or nausea
- Unusual fatigue or lightheadedness
If any of these symptoms occur, immediate medical attention is essential. Early intervention can save lives.
For now, Aasif Khan’s fans and colleagues continue to send him strength and support. And as he put it, he’ll be “back very soon”—with renewed gratitude and, hopefully, greater awareness for all.
© 2024 Bennett, Coleman & Company Limited

