- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Started At 3,100 Infected, Deadly Mosquito-Borne Virus Has Now Affected Over 7000 In China—Is Climate Or Travel To Be Blamed?

Credits: Canva
Foshan city in Guangdong Province is experiencing the country’s largest outbreak of chikungunya, a mosquito-borne viral disease that causes debilitating joint pain, fever, and fatigue. As of July 24, 2025, 3,645 cases have been confirmed—most of them mild, but alarming due to the rapid spread and potential for further outbreaks in surrounding regions.
This surge represents the most significant chikungunya transmission on the Chinese mainland since the virus was first detected there nearly two decades ago.
The epidemic began with an imported case of chikungunya in early July in Shunde District of Foshan, which is roughly 119 kilometers north of Hong Kong. Within weeks, cases ballooned to more than 3,300 in Shunde alone. Chinese officials have not officially attributed the cause, but experts cite favorable climatic conditions—hot and humid that facilitate mosquito breeding—and increased global travel as main drivers.
Chikungunya is transmitted by the Aedes mosquito, most specifically Aedes aegypti and Aedes albopictus. Both insects are famous for their daytime aggression of biting and love for tropical and subtropical regions.
Why Chikungunya Is No Minor Illness Even After All These Years?
The World Health Organization (WHO) defines chikungunya as a disease that is marked by severe joint pain, high fever, and signs and symptoms of headache, muscle pain, rash, vomiting, and fatigue. Though the majority of Foshan cases have been reported as mild, the disabling joint pain of the disease may persist for weeks or even months and can affect daily activities and productivity.
While not usually lethal, chikungunya has the potential to create large-scale public health disturbances, particularly in highly congested urban areas with inadequate mosquito control. To date, no serious or deadly cases have been reported in this outbreak, as indicated by China's Centre for Health Protection (CHP), but public health specialists caution against taking the situation lightly.
How Climate and Travel Are Driving This Outbreak?
Specialized tropical medicine doctors attribute the peak to favorable climatic conditions that promote quick growth of Aedes populations. These are aggressive, day-biting mosquitoes that thrive in warm, wet conditions, noting how climate change plays a major role in expanding habitats for mosquitoes.
Combine this international travel—imported and first case—and lack of immunity in the general population in China, and the stage was set for an outbreak. Chikungunya is not indigenous to China, so there is no herd immunity in the general population, and it was easier for the virus to establish itself and spread rapidly.
Link Between Chikungunya Cases on the Rise Globally
This outbreak is not unique. The European Centre for Disease Prevention and Control (ECDC) has reported 220,000 cases of chikungunya and 80 deaths in 2025 thus far worldwide. The WHO has made a global call to action citing the spread of chikungunya into new regions such as France and Italy, which have each reported locally-acquired infections in 2025.
Over five billion individuals in 119 countries reside in regions exposed to chikungunya infection and thus is considered a global health issue. The tropical diseases of chikungunya, dengue, and Zika are no longer limited to the equatorial belt-they are now reported from temperate regions as well.
To date, Hong Kong—a highly populated international center—has not seen any chikungunya cases after 2020. The territory is not home to Aedes aegypti, the main vector mosquito, but Aedes albopictus, a secondary vector known to spread the disease, is found there. The CHP cautions that imported cases still have the potential to result in local transmission if infected persons are bitten by mosquitoes within their communicable period.
Macao, just south of Guangdong, has registered its first two cases of chikungunya this year, both of them imported from Foshan and nearby Nanhai. Local authorities have stepped up mosquito control as a precaution against possible spread.
How Is China Managing The Outbreak?
With not much else in its bag of tricks, Guangdong Province has increased mosquito control operations, encouraging residents to clear standing water, unblock choked drains, and observe simple household sanitation. This is essential in interrupting the mosquito life cycle because still water provides a breeding ground for Aedes mosquitoes.
The CHP also recommends applying insect repellents, especially containing DEET or other WHO-recommended active compounds, and wearing long-sleeved clothing, especially in the early morning and late afternoon when mosquitoes are most prevalent.
The United States has only two licensed chikungunya vaccines, recommended mainly for visitors going to outbreak areas. However, China also doesn't have these vaccines available, which makes its citizens susceptible to successive waves unless mass vaccination is implemented or localized vaccines are created.
This leaves health authorities with few options: mosquito control, public awareness, and early diagnosis remain the main line of defense for the time being.
This epidemic is a clear message. Diseases such as chikungunya no longer remain isolated in small enclaves of tropical countries. With the climate still rising and international travel recovering after the pandemic, infectious disease is set to travel quicker and more far-reaching than ever before.
Dr. Tsui, a Guangdong public health official, explained in a press statement that chikungunya has the potential to quickly blow into large-scale outbreaks, particularly in highly populated regions with low mosquito densities and little immunity. The burden on healthcare systems, particularly in fast-growing urban areas of Asia, is a legitimate and increasing concern.
Ahmedabad Toddler Swallows Hulk Toy, Showed X-Ray, Doctors Remove It Via Endoscopy
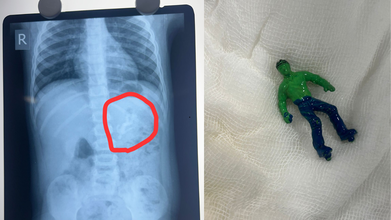
Credits: X
Ahmedabad toddler, one-and-a-half-year-old boy swallowed a 'Hulk' toy, which is based on a popular comic superhero. The toy was stuck in his stomach when his parents took him to the Civil Hospital. According to reports by News18, the child is identified as Vansh who showed the signs of discomfort and began vomiting. This is what alarmed the parents.
As per the News18 report, his mother Bhavika was suspicious when she noticed that one of his toys was missing. The child was rushed to the hospital and an X-ray revealed that he had swallowed the entire plastic toy. The toy was not broken.
Hindustan Times reported that Dr Rakesh Joshi, Head of the Department of Pediatric Surgery removed the toy through upper GI endoscopy. "Had it been a little late, the toy could have moved further from the stomach and got stuck in the intestines. In that case, there would have been a risk of intestinal blockage and even rupture," the senior doctor said.
"There is a natural valve between the esophagus and the stomach. The biggest challenge was to take out a whole toy through this valve. When we tried to grab it with the endoscope, the toy kept slipping because of the air in the stomach. Pulling the toy by its hand or foot raised the possibility of it getting stuck in the valve and causing it permanent damage," he said.
The doctor noted that if the toy had further slipped down, it would have increased the risk of intestine rupturing.
Ahmedabad Toddler Swallows Hulk Toy: What Parents Must Keep In Their Mind
Under the Toys (Quality Control) Order, 2020 issued by the Department for Promotion of Industry and Internal Trade under the Ministry of Commerce and Industry, toy safety in India was brought under mandatory BIS certification from September 1, 2020. The move aims to ensure safer toys for children while also supporting the government’s policy of curbing non-essential imports.
Industry sources estimate that more than 85 percent of toys sold in India are imported. Officials say the Toys Quality Control Order is a key step in preventing the entry of cheap and substandard toys into the domestic market, many of which fail to meet basic safety requirements.
Ahmedabad Toddler Swallows Hulk Toy: Standards for Electric and Non-Electric Toys
The quality control order clearly defines safety standards based on the type of toy. Non-electric toys such as dolls, rattles, puzzles, and board games must comply with IS 9873 (Part 1):2019. These toys do not rely on electricity for any of their functions.
Electric toys, which include at least one function powered by electricity, are required to meet the standards outlined under IS 15644:2006. Compliance with these standards is mandatory before such toys can be sold in the Indian market.
Ahmedabad Toddler Swallows Hulk Toy: Risks Linked to Untested Toys
Toys that are not tested by NABL-accredited toy testing laboratories can pose serious health risks to children. Sharp edges and poorly finished parts can cause cuts and injuries. PVC toys may contain phthalates, which are considered harmful chemicals.
Many low-quality toys have also been found to contain lead, a substance known to be particularly damaging to brain development in children. Soft toys with fur or hair can trigger allergies or become choking hazards. In some cases, small body parts can get stuck in gaps or holes, increasing the risk of injury.
Testing by NABL-accredited laboratories ensures that toys are safe, durable, and suitable for specific age groups. Parents are advised to check for IS marks on toys before purchasing, as this indicates compliance with Indian safety standards.
Ahmedabad Toddler Swallows Hulk Toy: What Parents Should Check Before Buying Toys
Experts recommend avoiding toys with small detachable parts for toddlers and young children, as they are more likely to put objects in their mouths. Toys should always match the child’s age, skill level, and interests.
Parents are also urged to look for IS marks, which confirm that the toy has been tested and certified. Loud toys should be avoided, as prolonged exposure to sounds above 85 decibels can harm a child’s hearing.
Electric toys with heating elements should be used with caution or avoided altogether due to burn risks. Finally, toys with sharp edges or shooting components should be carefully examined to prevent cuts and injuries.
Nipah Virus Outbreak In India: Myanmar Airport Tightens Health Screenings

Credits: iStock
Nipah virus outbreak in India triggered airport screenings of travelers, including in Myanmar. Many reports claim that passengers are being checked in similar ways as they were during the COVID-19 virus spread. Health and Me reported how in Thailand the health screenings of foreign travelers were taken seriously, a similar case is seen in Myanmar.
Nipah Virus Outbreak In India: How Are Travelers Screened In Myanmar?
Myanmar has tightened its health screenings and surveillance at Yangon International Airport to prevent any possible entry of Nipah virus case, reported The Global New Light of Myanmar. Travelers who are arriving from India, especially West Bengal are given special attention to check for any fever or other Nipah-related symptoms, read the report by the Ministry of Health.
The ministry also noted that health screening of passengers arriving from abroad is being conducted in line with the established guidelines for infectious diseases that could give rise to public health emergencies, Xinhua news agency reported.
Informational leaflets too are being distributed among travelers to be aware of the symptoms. Posters are also displayed at the airport. Along with all that, disease prevention and control measures are also being carried out in the airport.
Screening measures are also enhanced and implemented at Mandalay International Airport.
Nipah Virus Outbreak In India: What Is It?
As per the World Health Organization (WHO), Nipah virus infection is a zoonotic illness that is transmitted to people from animals, and can also be transmitted through contaminated food or directly from person to person.
In infected people, it causes a range of illnesses from asymptomatic (subclinical) infection to acute respiratory illness and fatal encephalitis. The virus can also cause severe disease in animals such as pigs, resulting in significant economic losses for farmers.
Although Nipah virus has caused only a few known outbreaks in Asia, it infects a wide range of animals and causes severe disease and death in people.
Nipah virus is infectious and can spread from animals like bats and pigs to humans through bodily fluids or contaminated food. It can also pass between people through close contact, especially in caregiving settings. While it can spread via respiratory droplets in enclosed spaces, it is not considered highly airborne and usually requires close, prolonged contact for transmission. Common routes include direct exposure to infected animals or their fluids, consuming contaminated fruits or date palm sap, and contact with bodily fluids such as saliva, urine, or blood from an infected person.
Nipah Virus Outbreak In India: What Are The Common Symptoms?
- Fever
- Headache
- Breathing difficulties
- Cough and sore throat
- Diarrhea
- Vomiting
- Muscle pain and severe weakness
Measles Outbreak In Disneyland: An International Traveler Gets Infected

Credits: iStock
Measles Outbreak in Disneyland: Health officials in Orange County sounded alarmed after they confirmed a recent measles case in a child who visited Disneyland last week. The Orange County Health Care Agency said on Saturday that the child was an international traveler who arrived at Los Angeles International Airport (LAX). The child then went to Disneyland on Wednesday and that is what became the potential exposure window.
As per the health authorities there could be two possibilities of getting the disease:
- Goofy’s Kitchen in Disneyland Hotel, 10:30 a.m. to 1:30 p.m. on Wednesday
- Disneyland Park and Disney California Adventure Park, 12:30 p.m. to closing on Wednesday.
Health authorities said they are coordinating with Disneyland to contact employees who may have been exposed to measles. According to Orange County health officials, visitors present at the theme park during the identified period could develop symptoms between seven and 21 days after exposure.
Measles Spreads Easily, Experts Warn
Dr Danielle Curitore, a pediatrician at St Joseph Heritage Providence, explained NBC Los Angeles that measles is highly contagious and spreads through respiratory droplets.
“Very similar to these respiratory viruses, but even more so because it can be in a close setting and if that person with measles sneezes or coughs and transmits some respiratory droplets, you are exposed,” she said. “And that room that they’ve been in is also contagious for at least two hours after they left.”
Measles Outbreak In Disneyland: Vaccination Remains The Strongest Protection
Doctors emphasize that individuals who have received the measles vaccine, particularly the recommended two doses, are generally well protected against the disease. Those who have not been vaccinated face a significantly higher risk of infection.
Read: Measles Elimination Status In The US Is ‘Not Really’ At Risk, CDC Says As Cases Surge
“Your best protection is to be vaccinated, so if you’ve been vaccinated against measles and you’ve received your two doses of measles vaccine at any point, those are usually given in childhood but you do continue to be immune as you get older,” Dr Curitore added.
New Measles Cases Reported In Southern California
Health officials have confirmed at least five new measles cases in Southern California, prompting renewed warnings and surveillance. Authorities are closely monitoring the situation to limit further spread and identify potential exposure chains.
What Is Measles?
Measles, also known as rubeola, is an extremely contagious viral illness that typically causes high fever, cough, runny nose, red and watery eyes, and a characteristic rash that begins on the face and spreads downward across the body. It spreads through respiratory droplets and can lead to severe and sometimes fatal complications, including pneumonia and inflammation of the brain known as encephalitis.
Although it is preventable through the safe and effective MMR vaccine, measles remains a serious threat in many regions. There is no specific cure, and treatment focuses on managing symptoms, according to the Cleveland Clinic.
Measles Outbreak In Disneyland: Common Symptoms To Watch For
Experts say measles symptoms often begin with signs similar to a common cold, including cough, congestion, and high fever. Some patients may also develop conjunctivitis.
“Sometimes it just starts out like the common cold cough congestion: high fever sometimes conjunctivitis can be part of it,” Dr Curitore said. “Then day three to five, you get that very classic measles rash, which usually starts on the face, center of the body.”
© 2024 Bennett, Coleman & Company Limited

